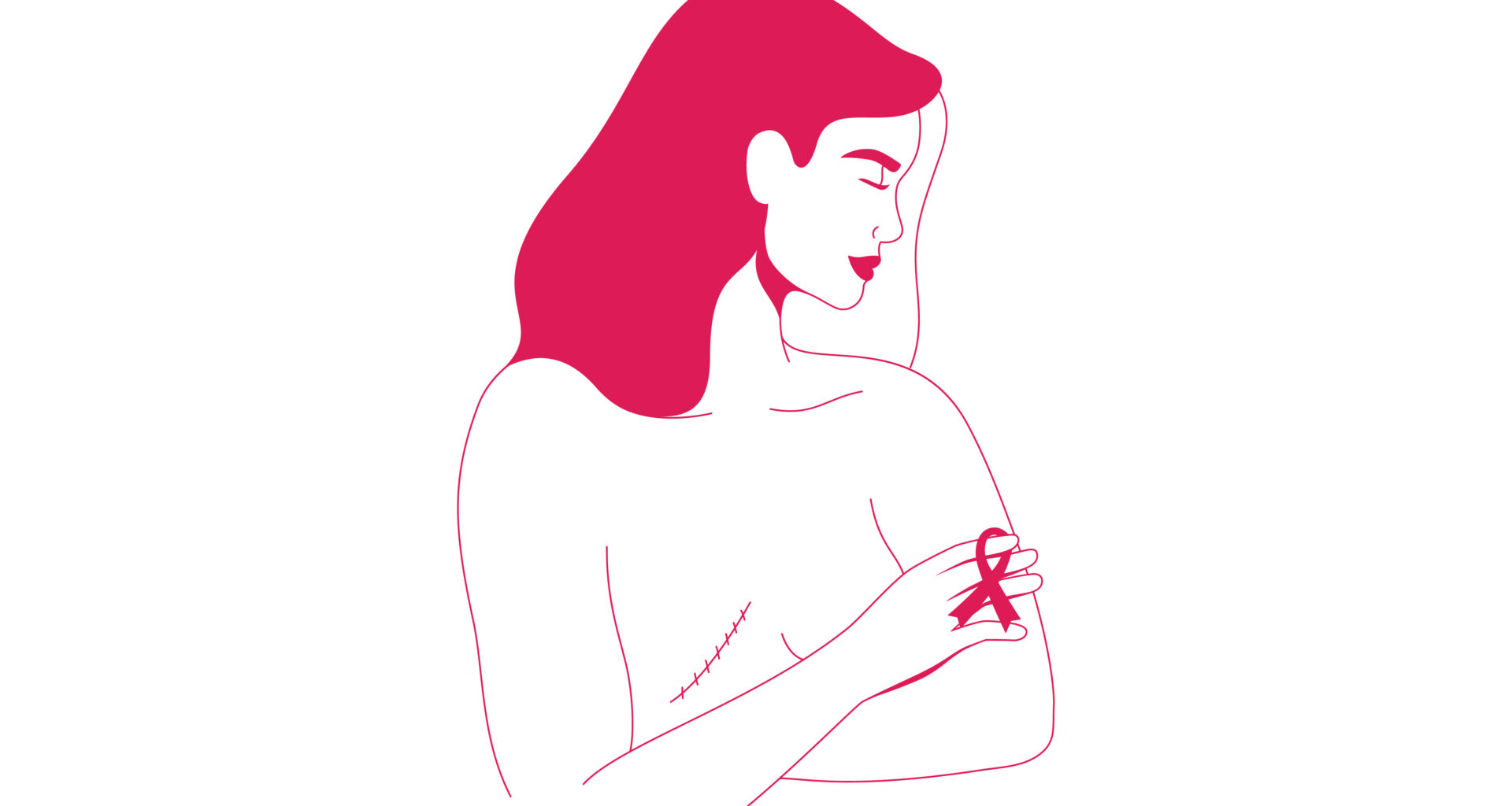
Although mastectomy is often a necessary and life-saving treatment option for many women with breast cancer, the surgery may contribute to worse sexual health, body image, and several other physical and emotional challenges after surgery, according to a recent systematic review on the effects of mastectomy in women with breast cancer. Surgeons said the research underscores the importance of screening women before they undergo mastectomy. The research was presented at the 2025 American College of Surgeons (ACS) Clinical Congress in Chicago and published in the Journal of the American College of Surgeons.
“As surgeons, we often focus on the medical side of care. There is no universal or standardized approach to counseling women on the full range of physical and emotional outcomes after mastectomy,” said Lauren Raymond-King, MD, lead author of the research and a surgical resident at Yale School of Medicine. “As a result, many women go into surgery with an incomplete understanding of what to expect in the long-term, not just physically, but emotionally and psychologically, after undergoing a mastectomy.”
Though a common procedure, mastectomy is a major surgery that requires long-term follow-up care. More than a quarter of patients with breast cancer typically undergo mastectomy, and many patients are staying in the hospital for shorter periods after surgery—a trend that prompted the investigators to analyze patients’ outcomes after mastectomy through a systematic review.
Of nearly 3,000 studies identified, researchers analyzed 20 studies that met their inclusion criteria, examining the effects of mastectomy on quality of life, sexual health, and psychosocial well-being. All the articles focused on the experience of women with stage I to III breast cancer. Studies involving women with stage IV breast cancer, as well as women who elected to undergo a prophylactic mastectomy for cancer risk reduction, were excluded from the study because of the distinct needs and different overall medical decision-making for these patients.
Key Findings
Worse psychosocial outcomes for women who undergo mastectomy: Of 20 studies analyzed, 15 reported worse psychosocial outcomes for patients undergoing mastectomy in at least one psychosocial domain.
No standardized approach to assess postsurgical quality of life: There were 38 different patient-reported outcome measures identified across the 20 studies. The most commonly assessed psychosocial domains were body image (55%), sexual health or sexual function (50%), pain or physical function (45%), and quality of life (40%); fewer assessed psychosocial health (35%) and satisfaction (25%).
Need for a standardized approach: Most patient-reported outcome measures (PROMs) were used only once (72%), with studies ranging from using one PROM to up to eight different PROMs to assess psychosocial outcomes after surgery. This wide variation underscores the need to better prepare women with a validated screening tool or other methods before they undergo mastectomy, the authors said.
“Breast cancer impacts so many patients in our country, and there’s constant research being done to improve survival outcomes,” said Elizabeth Berger, MD, MS, FACS, senior author of the research and Assistant Professor of Surgery at Yale School of Medicine. “Now that there are so many more survivors of breast cancer, we can’t miss the opportunity to study quality-of-life outcomes for our patients, since they are living so much longer after their diagnosis and treatment.”
The study is limited by the research included in the systematic review, which may vary in quality and study design, making it difficult to draw conclusions across the studies, the authors noted. Future research will focus on developing a validated screening tool designed to assess the readiness of women facing mastectomy.
Disclosure: The authors reported no conflicts of interest.