Cultural Context and the Limits of Genetic Counseling
Premarital screening and genetic counseling are widely recognized as essential strategies for identifying at-risk couples and enabling informed decisions regarding marriage. However, in Arab-Muslim cultures, marriage involves complex emotional, familial, and religious considerations. Even when couples are informed of their genetic risk, many still choose to marry due to cultural values and fear of social stigma associated with breaking engagements or annulments [78, 79]. In some contexts, prenatal diagnosis and therapeutic abortion are available, yet these options are often avoided due to religious prohibitions or moral hesitation. These findings highlight the crucial need to strengthen health literacy related to hemoglobinopathies, including thalassemia, in ways that are compatible with the sociocultural landscape [27]. Without culturally informed education, prevention strategies may have limited reach and effectiveness [27, 78, 79].
Curricular Gaps and Misconceptions in Secondary Education
An analysis of Tunisia’s biology curriculum for public secondary schools reveals that thalassemia is not mentioned, and sickle cell disease appears only marginally, and solely as an academic concept. Core aspects such as prevalence, severity, symptoms, psychosocial impact, and available therapies are omitted. Consequently, students lack the foundational knowledge required for informed health-related decisions. Survey findings confirm widespread misconceptions: many students confuse thalassemia with iron-deficiency anemia or infectious diseases, indicating severe gaps in health literacy. These misunderstandings are more pronounced among students in literary tracks, reflecting inequitable curricular exposure to genetics and chronic disease education.
This educational disparity is not unique to Tunisia. Similar findings have been reported in Saudi Arabia [80] and Bangladesh, where students from scientific backgrounds demonstrated significantly higher knowledge levels compared to their peers from literary disciplines [81]. Studies consistently demonstrate that targeted education enhances students’ acceptance of prevention strategies and promotes informed behaviors [80,81,82,83,84,85]. For example, Iran’s integration of mandatory premarital screening and school-based education has led to a significant reduction in thalassemia incidence [85]. Indonesian studies also show improved knowledge and attitudes toward premarital screening among Muslim couples following tailored educational interventions [86]– [87].
Health and Genetic Literacy: Current Status and Implications
The current status of health and genetic literacy among Tunisian adolescents reveals a profound gap between the demands of contemporary public health challenges and the educational preparation offered by the school system. Despite the increasing relevance of hereditary diseases such as thalassemia in Tunisia and across the Mediterranean region, students, particularly those outside the scientific track, have limited access to accurate, contextualized, and actionable information about these conditions. The findings of this study indicate that even when students demonstrate a basic awareness of genetic inheritance, their understanding remains superficial, fragmented, and often clouded by persistent misconceptions.
In many cases, students confuse thalassemia with iron-deficiency anemia, underestimate the severity and chronic nature of the disease, or are unaware of its prevalence and genetic transmission. Such confusion is not merely a reflection of individual ignorance; it points to deeper systemic deficiencies in how health and genetics are addressed in the educational landscape. The lack of a structured curriculum on health literacy [88] and the marginal treatment of genetic diseases within biology courses contribute to a passive and disengaged approach to personal and familial health. Moreover, the absence of emotional and civic framing around hereditary health risks limits students’ ability to relate biomedical knowledge to their own lives and social responsibilities.
The implications of this low level of genetic literacy are significant. Without a clear understanding of how genetic diseases are inherited and how they affect individuals and families, adolescents are unlikely to recognize the importance of preventive measures such as premarital screening or genetic counseling. This absence of understanding hinders the development of health-promoting attitudes and behaviors, both at the individual and community levels. In a context where consanguineous marriages remain culturally accepted and often preferred, the lack of genetic awareness may perpetuate avoidable health burdens and intergenerational suffering.
Furthermore, the study shows that even students in the scientific track, who have relatively more exposure to genetics, struggle to integrate what they learn into meaningful frameworks for action. The content is often presented in a purely technical or abstract manner, without connection to the sociocultural realities or emotional experiences of the students. This disconnection inhibits the development of what could be termed functional genetic literacy: the capacity not only to comprehend biomedical information but also to use it in making informed decisions that are emotionally grounded and socially responsible.
Addressing these shortcomings requires a redefinition of health and genetic literacy as more than the acquisition of factual knowledge [88]. It must be understood as a multidimensional competence that includes cognitive, emotional, ethical, and civic dimensions. A literate individual in this sense is not only capable of understanding genetic information but also of assessing its personal and societal implications, communicating effectively about health risks, and acting in ways that promote collective well-being.
Functional Literacy in Human Genetics
Functional literacy in human genetics refers to the capacity to understand, interpret, and apply genetic information to real-life contexts such as health risk assessment, reproductive decision-making, and disease prevention. The results of this study reveal critical deficiencies in this domain among Tunisian secondary school students. Nearly half of the respondents did not know that thalassemia is a hereditary condition. A significant portion of students, regardless of academic track, held erroneous beliefs, including the idea that thalassemia is either infectious or caused by nutritional deficiencies. Even among students in the scientific stream, where some exposure to genetics is expected, the understanding of fundamental mechanisms, such as autosomal recessive inheritance, was inconsistent and fragmented. Only a small minority demonstrated the ability to accurately assess genetic risk within premarital or reproductive scenarios, highlighting a concerning lack of both durable and applicable knowledge.
This situation is even more pronounced among students in the literary track, who receive little to no instruction in genetics as part of their formal education. These students struggled significantly with questions related to genetic mechanisms, risk perception, and disease prevention. The absence of genetics education in this track reveals a profound equity gap: it systematically excludes a substantial portion of the youth population from engaging meaningfully with health information that is vital for their personal and familial well-being. This exclusion perpetuates social and health inequalities, particularly in a context where hereditary diseases like thalassemia are highly prevalent and closely linked to reproductive choices.
The complexity of genetic concepts compounds the problem. Genetics relies heavily on specialized, abstract terminology, such as “heterozygote” or “autosomal”, that is rarely encountered in everyday language. As several studies have emphasized [89,90,91,92], mastering such terminology is indispensable for understanding core biological processes. However, this linguistic barrier creates an additional layer of exclusion for students with limited scientific exposure or weak proficiency in academic language. The role of language in learning becomes particularly salient when viewed through the lens of Vygotski’s socioconstructivist theory [93], which posits that conceptual development is inextricably linked to mastery of the language tools used to mediate knowledge. From this perspective, students cannot develop robust scientific understanding without opportunities to engage with, and appropriate, the specific discourse of genetics.
Considering these findings, it is clear that improving functional literacy in human genetics requires much more than increasing content coverage. It demands pedagogical approaches that scaffold the acquisition of technical vocabulary, contextualize genetic knowledge in meaningful scenarios, and provide equitable learning opportunities across all academic tracks. Without such reform, a large segment of the student population will remain ill-equipped to make informed health decisions, thereby limiting the effectiveness of any public health strategy aimed at preventing hereditary conditions like thalassemia.
Addressing functional genetic literacy must be framed as both an educational and public health imperative. Equipping all students with the ability to understand and act upon genetic information is not only a matter of cognitive development but also of health justice, especially in societies facing a high burden of genetic diseases and entrenched disparities in access to scientific education.
Emotional and Behavioral Attitudes Toward Thalassemia
Surveyed students did not perceive thalassemia as a serious disease. Many ranked it below cancer, cardiovascular disease, or diabetes in terms of perceived danger. Fear of being affected was low, especially among male students. Female students expressed more concern, suggesting gendered differences in health perception. However, the overall absence of fear signals a lack of disease awareness, not courage or negligence.
Misinformation was also evident in attitudes toward contagion and life limitations. A substantial proportion believed thalassemia was contagious and did not interfere with academic or professional success. Such misconceptions diminish students’ perceived urgency to engage in preventive actions.
On the behavioral side, while half of the students supported premarital counseling, only 40% found prenatal diagnosis useful. Concerns about needle procedures, risk to the fetus, and fear of abortion decisions may explain this hesitancy. In terms of communication, many agreed that hiding illness was preferable, a belief likely rooted in fear of stigma. Students observed that society, school, and the workplace are often unkind to the chronically ill, a finding consistent with other studies documenting the stigma surrounding hemoglobinopathies [7, 8, 94, 95].
Only half of respondents would inform their partners of their carrier status, highlighting social and familial pressures. Nevertheless, in the domain of social engagement, most students expressed willingness to support thalassemia-affected children and agreed on the value of blood donation, even without understanding its role in treatment. These attitudes can be leveraged through awareness programs.
Structural Determinants: Socioeconomic, Cultural, and Religious Barriers
Efforts to improve health literacy must contend with broader structural and cultural barriers. In Tunisian and other Arab-Muslim societies, thalassemia prevention strategies, such as genetic counseling or partner screening, challenge prevailing beliefs about fate (“maktoub”), divine will, and the sanctity of marriage.
Macrosocial inequalities exacerbate these challenges. In Tunisia, the absence of a national carrier screening policy and the limited availability of specialized care centers reflect a broader trend of prioritizing communicable diseases over hereditary disorders, which affect politically and economically marginalized populations. The epidemiological hierarchy favors diseases that pose a public health threat over those that cause chronic personal suffering. Without international funding or public pressure, non-transmissible diseases like thalassemia remain neglected.
Bio-social inequalities are also evident. Women bear a disproportionate burden, both as carriers and caregivers. In many Arab-Muslim cultures, women are often blamed for their children’s genetic conditions [66, 96]. This leads to silence, stigma, and isolation. Fear of judgment or abandonment often prevents mothers from seeking timely care. Children with thalassemia experience school discrimination due to their condition being poorly understood. These findings echo studies across the Middle East that highlight gendered vulnerability and silence surrounding genetic conditions.
Curricular Implications and a Path Forward
The findings of this study point to critical shortcomings in the current Tunisian educational curriculum, particularly in its ability to prepare students, regardless of academic track, for active engagement in health prevention. The biology curriculum, as it stands, offers limited, decontextualized information on hereditary diseases, often disconnected from real-world concerns and emotional relevance. This disconnect is particularly pronounced in the literary and technical tracks, where students have little or no exposure to genetic topics. As a result, large segments of the adolescent population are denied access to the knowledge and critical thinking skills necessary to understand, assess, and respond to hereditary health risks such as thalassemia.
The absence of a structured and inclusive health education component in the national curriculum further exacerbates these inequities. This structural void reinforces patterns of social and scientific exclusion, whereby only students in science-focused streams have partial access to biomedical information, while others remain uninformed or misinformed. Such asymmetry in knowledge access deepens existing disparities and weakens collective health preparedness. Therefore, reform is urgently needed to integrate thalassemia-related content into a cross-cutting health education program, accessible to all students, regardless of academic specialization.
A curriculum reform guided by the principles of health literacy would not only improve scientific knowledge but also foster personal relevance and emotional engagement, two essential conditions for behavioral change. In this regard, the Common-Sense Model (CSM) of illness representation provides a valuable theoretical framework. By addressing students’ lay perceptions and misconceptions about health threats, early educational interventions can reshape cognitive representations and encourage proactive health behaviors. Applying the CSM to school-based health education allows educators to engage with students’ intuitive beliefs and help them develop more accurate, evidence-based understandings of genetic risks, including thalassemia [97].
Such an approach calls for the development of interdisciplinary modules that blend biology, ethics, civic education, and psychosocial perspectives. These modules should emphasize not only the biomedical dimensions of thalassemia but also its emotional, familial, and social implications. Introducing these topics in a way that speaks to students’ lived experiences can bridge the gap between abstract content and real-life decision-making. This is particularly relevant in a context like Tunisia, where cultural, religious, and familial values significantly influence marriage choices and reproductive health behaviors.
A path forward would involve phased implementation of curricular innovations, beginning with the integration of pilot modules in selected schools. These modules should be evaluated for pedagogical impact and adapted accordingly before national scaling. Simultaneously, teacher training initiatives must be developed to equip educators with both content knowledge and participatory pedagogical techniques. Collaboration with public health institutions, NGOs, and community leaders will be essential to ensure that educational reforms are scientifically grounded and socially relevant.
Curricular transformation must be conceived not as an isolated educational endeavor, but as a public health imperative. By embedding genetic literacy and preventive thinking within the educational system, Tunisia can take a decisive step toward empowering its youth to make informed, ethical, and culturally sensitive health decisions [63, 88]. Such reform will serve not only the goal of thalassemia prevention but also the broader objective of strengthening civic responsibility and health resilience among future generations.
Recommendations for Policy and Practice
The findings of this study strongly advocate for the formulation and implementation of a comprehensive, long-term strategy to address the educational and public health gaps in thalassemia prevention among Tunisian youth. A coordinated national response, grounded in evidence and adapted to the sociocultural context, is necessary to build the genetic and health literacy required for meaningful primary prevention. This response must operate on multiple time scales, short, medium, and long term, each involving specific actions, institutional collaboration, and sustained political commitment.
In the short term, the priority should be to build national capacity for delivering accurate, relevant, and culturally sensitive education on thalassemia and genetic risk. This begins with targeted training for biology and health education teachers at the secondary school level. Educators must be equipped not only with scientific knowledge about hemoglobinopathies but also with pedagogical tools and strategies for engaging adolescents from diverse academic and social backgrounds. Teacher training should integrate content on genetics, hereditary transmission, premarital screening, and sociocultural perceptions of disease, while fostering inclusive classroom dialogue to challenge stigma. Simultaneously, awareness campaigns tailored to youth should be launched at the national level, using digital platforms, school-based events, and media to disseminate accessible, age-appropriate information on thalassemia. These campaigns should be developed in partnership with health professionals, educators, and civil society organizations to ensure credibility and reach.
Over the medium term, Tunisia should aim to integrate a dedicated thalassemia education module into the official secondary school curriculum. This module should be interdisciplinary in nature and delivered not only in scientific streams but also in literary and technical tracks, thus ensuring equitable access to knowledge regardless of academic orientation.
The educational content must go beyond the biological aspects of the disease and include psychosocial, cultural, and ethical considerations. The module should emphasize the hereditary nature of thalassemia, the importance of premarital screening, the challenges faced by affected individuals, and the potential of preventive measures. Classroom activities may involve case studies, group discussions, role-playing scenarios, and peer education strategies to foster both cognitive and emotional engagement. Institutional collaboration between the Ministries of Education and Health will be essential to support curriculum design, teacher recruitment and training, and school-level implementation. A national monitoring and evaluation framework should be established to track the effectiveness of the new curriculum in terms of knowledge acquisition, attitude change, and behavioral intentions among students.
In the long term, the goal should be to institutionalize a national thalassemia prevention policy that includes both educational and biomedical components. This policy would mandate premarital genetic counseling and carrier screening as part of routine reproductive health services, while also embedding genetic education within the broader public health strategy. To support this objective, specialized centers for genetic counseling and hemoglobinopathy care should be established or reinforced across the country, particularly in underserved regions. These centers would not only provide diagnostic and therapeutic services but also serve as hubs for community education and support.
Public communication campaigns should continue to evolve, addressing stigma, promoting solidarity with affected families, and normalizing conversations around genetic risk. Religious and community leaders should be engaged to ensure that prevention messages are compatible with prevailing moral and cultural frameworks, particularly with respect to marriage, reproduction, and divine will.
Crucially, all these actions must be informed by ongoing research and data collection. This includes assessing students’ evolving levels of genetic literacy, tracking the uptake of premarital screening, and evaluating the social impact of education programs. Regular feedback from teachers, students, parents, and health professionals should be integrated into program revisions, ensuring that thalassemia education remains relevant, effective, and inclusive. Collaborative efforts with regional and international partners may provide technical expertise, financial support, and opportunities for comparative evaluation.
Overall, these policy recommendations emphasize the importance of a multi-sectoral, equity-focused, and culturally grounded approach to thalassemia prevention. By investing in health and genetic literacy through the education system, Tunisia can equip its youth with the knowledge and agency to make informed reproductive decisions, reduce hereditary disease burden, and foster a public health culture that is inclusive, proactive, and responsive to emerging challenges.
Pilot Thalassemia Education Module: Concept and Evaluation
In light of the study’s findings and the critical need to enhance genetic and health literacy among Tunisian adolescents, we propose the development and experimental implementation of a pilot thalassemia education module in selected secondary schools. This module is envisioned as both a pedagogical and public health intervention, aiming to increase students’ understanding of thalassemia, its hereditary transmission, and the importance of preventive behaviors such as premarital screening and informed reproductive decision-making.
The conceptual framework guiding the module’s design is rooted in health literacy theory, which emphasizes not only the acquisition of factual knowledge but also the development of critical thinking, risk perception, and decision-making skills in health-related contexts. In addition, educational psychology principles, particularly those related to active learning, socio-constructivist engagement, and emotional involvement, will inform the instructional strategies used. The module is thus intended to promote not only cognitive comprehension but also emotional and ethical reflection, enabling students to make sense of thalassemia not simply as a genetic disorder but as a socially situated condition that affects individuals, families, and communities.
The content of the module will be interdisciplinary and adapted to the Tunisian curricular context. It will cover basic genetic concepts relevant to hemoglobinopathies, the epidemiological profile of thalassemia in Tunisia and the Mediterranean region, the clinical manifestations and psychosocial consequences of the disease, and the available preventive strategies. A particular emphasis will be placed on understanding autosomal recessive inheritance patterns, the implications of consanguineous marriage, and the social and cultural representations of genetic diseases. The module will also encourage reflection on students’ own values, beliefs, and future aspirations with regard to marriage and health, fostering a sense of personal relevance and agency.
In terms of pedagogy, the pilot module will prioritize active learning methods that encourage student participation and peer interaction. These may include scenario-based discussions, group debates, role-playing exercises, problem-solving tasks, and the analysis of testimonial materials from individuals living with thalassemia. The goal is to create a learning environment where students feel empowered to ask questions, challenge misconceptions, and engage critically with the content. The use of digital tools, audiovisual resources, and culturally adapted materials will further enhance accessibility and engagement.
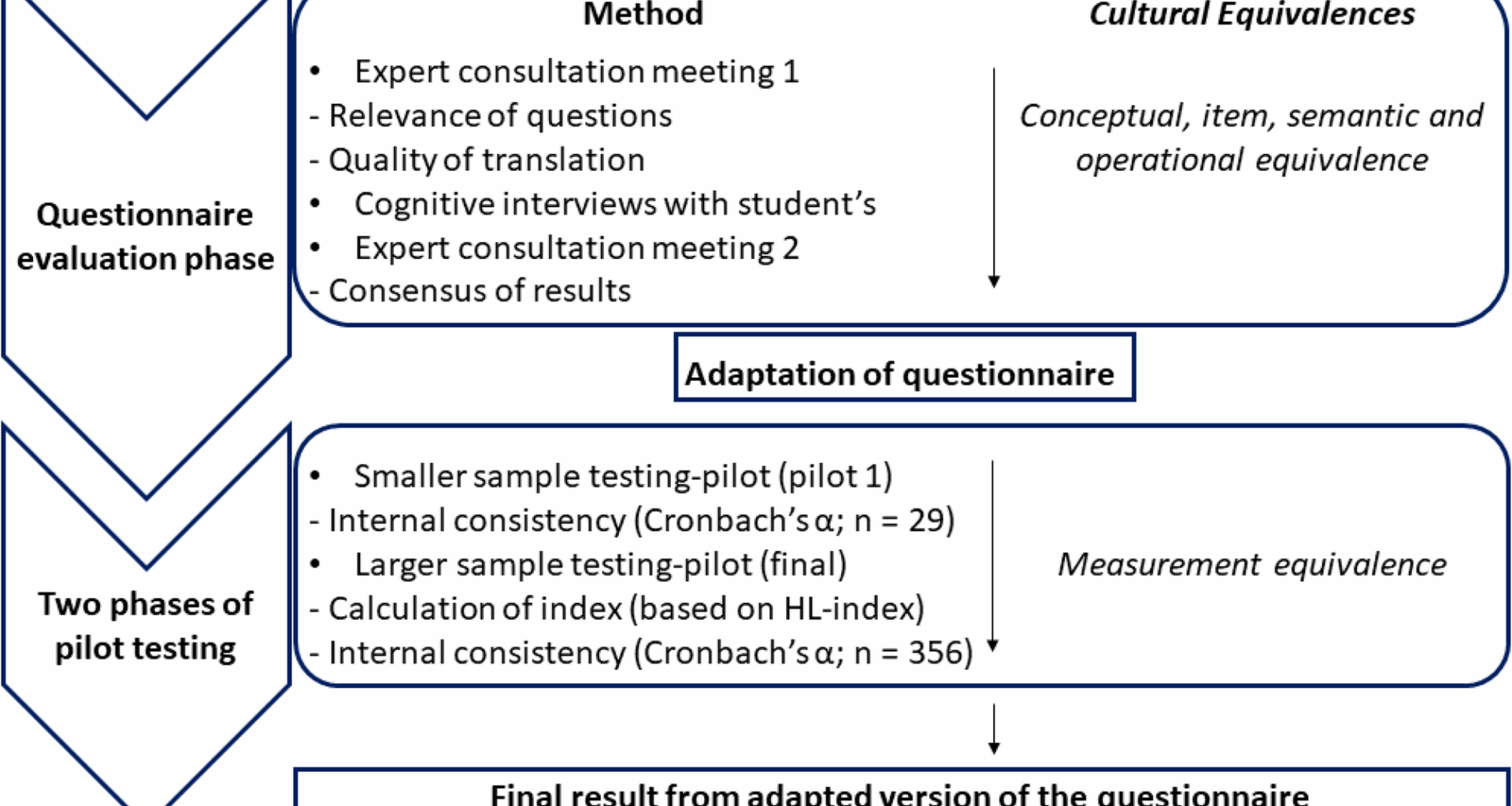
The evaluation of the pilot module will adopt a mixed-methods approach to assess both its feasibility and its educational impact. Quantitative data will be collected through pre- and post-intervention questionnaires measuring students’ knowledge, attitudes, and intentions regarding thalassemia and genetic screening. These instruments will be developed based on validated health literacy and genetic literacy scales, adapted to the local context. Qualitative data will be gathered through focus group discussions and interviews with students, teachers, and school administrators, aiming to capture perceptions of the module’s relevance, clarity, cultural appropriateness, and emotional impact. Teachers will also be asked to document their experiences and challenges in delivering the module, providing essential feedback for future adjustments.
The implementation will be conducted in collaboration with the Ministry of Education, regional educational authorities, and local health professionals, ensuring that the module is both scientifically accurate and pedagogically sound. Schools will be selected based on their geographical, sociocultural, and academic diversity, allowing the evaluation to capture a range of learning contexts and identify potential barriers to scale-up.
The ultimate aim of this pilot initiative is to generate empirical evidence that can inform national curriculum reform and guide the integration of genetic health education into the broader framework of adolescent health promotion. If proven effective, the module could serve as a model for other health-related topics requiring sensitive, interdisciplinary, and youth-centered approaches. It would also position Tunisia as a regional pioneer in the educational response to hereditary diseases, aligning with global public health strategies promoting health literacy and disease prevention from an early age.
Future Directions and Research Priorities
Building upon the insights gained from this study, several future directions emerge to deepen the understanding of health literacy and to optimize educational strategies for thalassemia prevention among adolescents. First, it is essential to expand the empirical research base through longitudinal studies that assess the long-term impact of school-based genetic education interventions. While short-term improvements in knowledge and attitudes are valuable, they do not necessarily translate into sustained behavioral changes.
Future studies should therefore investigate whether early exposure to health education influences young people’s reproductive decisions, including their willingness to undergo premarital screening or seek genetic counseling in adulthood.
Another priority involves exploring the differential effects of educational interventions across various sociocultural, regional, and socioeconomic contexts in Tunisia. The country exhibits considerable heterogeneity in terms of health service access, educational quality, and cultural attitudes toward genetic disorders. Understanding how these contextual factors shape adolescents’ reception of health information, and their decision-making processes will be crucial for designing equitable and culturally appropriate interventions. Comparative studies involving rural and urban populations, as well as different educational tracks (scientific, literary, vocational), could provide valuable insights into the conditions that enhance or hinder the effectiveness of health literacy efforts.
A third area for future research concerns the role of emotions, stigma, and family dynamics in shaping adolescents’ perceptions of genetic risk and their openness to preventive action. Given the sensitivity of the topic and the cultural significance of marriage and reproduction in Tunisian society, educational approaches must go beyond cognitive instruction and address the emotional and relational dimensions of health literacy. Interdisciplinary research combining education sciences, medical anthropology, and psychology could help elucidate how fear, shame, family loyalty, and social expectations interact with young people’s learning processes and health behaviors.
Technological innovation also presents a promising avenue for expanding the reach and appeal of health literacy interventions. Future research should examine the integration of digital tools, such as mobile health applications, serious games, and interactive learning platforms, in the promotion of genetic awareness among youth. These tools offer opportunities for personalization, interactivity, and real-time feedback, which may be particularly effective in engaging adolescents and reinforcing learning outcomes. Evaluations of these technologies should assess not only usability and engagement but also their impact on knowledge retention, critical thinking, and behavioral intentions.
In addition, further investigation is needed into the training needs of educators tasked with delivering health-related content. Teachers play a pivotal role in mediating complex scientific information and facilitating sensitive discussions in classrooms. Research should therefore explore the competencies, attitudes, and support systems required for teachers to feel confident and prepared to engage students in topics such as thalassemia, genetic inheritance, and reproductive health. Pilot training programs and capacity-building workshops could be tested and evaluated to inform national teacher training frameworks.
Finally, it is important to pursue interdisciplinary and international collaborations that allow for knowledge exchange and comparative analysis. Lessons learned from other countries with similar epidemiological and sociocultural profiles, particularly in the Mediterranean and North African regions, can inform the development of contextually adapted strategies. Joint research projects, regional networks, and shared data platforms would strengthen the evidence base and support the formulation of coherent, evidence-informed policies for thalassemia prevention.
Broader Public Health Implications
The insights gleaned from this study have significant implications for public health policy and practice, particularly in the context of hereditary disease prevention and health equity. Thalassemia, as a genetic disorder with profound physical, psychosocial, and economic consequences, presents a paradigmatic challenge for integrating non-communicable disease prevention within existing health frameworks. The chronic nature of thalassemia, combined with its inherited transmission and potential for stigmatization, calls for a multidimensional approach that transcends conventional biomedical interventions.
A critical implication of our findings is the recognition of health literacy as a foundational component of effective public health strategies. Enhancing genetic literacy among adolescents empowers future generations to make informed reproductive choices, reducing the incidence of new thalassemia cases and mitigating the disease burden at the population level. Such literacy is not merely the acquisition of scientific knowledge but also encompasses the development of risk awareness, emotional readiness, and social competencies necessary to navigate complex health decisions. Therefore, public health initiatives must prioritize education as a primary prevention tool alongside screening and clinical services.
Moreover, addressing thalassemia prevention through education contributes directly to the reduction of health disparities. In Tunisia and similar contexts, disparities in access to health information, healthcare infrastructure, and social support disproportionately affect marginalized populations, including those in rural or socioeconomically disadvantaged areas. By integrating genetic education into the school system, especially targeting all academic tracks and geographic regions, policy makers can promote equity in health knowledge and preventive capacities. This approach aligns with global health priorities emphasizing universal health coverage and the social determinants of health.
The psychosocial dimension of thalassemia also demands public health attention. Stigma and discrimination associated with hereditary diseases often lead to concealment, delayed diagnosis, and psychological distress for affected individuals and their families. Our study highlights the widespread misconceptions and social taboos surrounding thalassemia, which undermine both individual well-being and community support structures. Public health campaigns must therefore incorporate stigma reduction strategies, fostering inclusive attitudes and normalizing conversations about genetic risks within communities. Engaging community leaders, religious authorities, and media outlets can facilitate culturally sensitive messaging that respects prevailing values while encouraging openness.
Furthermore, the findings reinforce the imperative to adopt a life-course perspective in public health. Early intervention during adolescence, a critical developmental stage characterized by identity formation and future planning, offers a unique opportunity to shape health behaviors and attitudes that will persist into adulthood. Equipping young people with the knowledge and skills to understand and manage hereditary risks enhances their capacity for self-care and informed participation in reproductive health decisions, contributing to broader societal health gains.
Finally, the integration of thalassemia education within the public health agenda must be accompanied by systemic investments in healthcare infrastructure, including accessible genetic counseling services, diagnostic laboratories, and specialized treatment centers. Without these complementary components, educational efforts risk being undermined by gaps in service availability and quality. A comprehensive public health strategy, therefore, requires coordinated action across education, health care delivery, community engagement, and policy regulation.
In conclusion, the broader public health implications of promoting thalassemia-related health literacy are profound. This approach advances disease prevention, reduces inequities, addresses psychosocial challenges, and fosters a culture of informed health decision-making. It exemplifies the potential of health education as a transformative force within public health, particularly in contexts facing the dual burdens of hereditary and chronic diseases.
A Call for Intersectoral Collaboration
Addressing the complex challenges posed by thalassemia prevention requires more than isolated efforts from the health or education sectors alone. It demands a concerted, intersectoral approach that brings together diverse actors across governmental, academic, civil society, and community domains. The findings of this study highlight that sustainable and effective health education interventions, particularly those targeting adolescents, must be situated within a broader ecosystem of collaboration, where shared responsibilities, resources, and expertise are mobilized in a coordinated manner.
The education sector plays a central role in this collaborative framework. Ministries of education are pivotal in integrating genetic literacy into national curricula and in ensuring that teachers are adequately trained and supported to deliver sensitive content related to hereditary diseases and reproductive health. Such efforts must be undertaken in dialogue with public health institutions, whose input ensures the scientific accuracy and relevance of educational content. Joint planning between these two sectors can foster the development of contextually appropriate modules, continuous teacher training, and systematic evaluation mechanisms to monitor outcomes over time.
The health sector, for its part, must move beyond a purely clinical approach and embrace its role in upstream prevention. Ministries of health and relevant health agencies must invest in public health communication campaigns, expand access to voluntary screening and counseling services, and facilitate the development of community-based support systems. Collaboration with schools offers a strategic entry point to reach adolescents and their families with preventive messaging and services, particularly in regions where health infrastructure may be limited. Intersectoral agreements and shared budget lines can institutionalize such cooperation and enhance its sustainability.
Academic and research institutions also have a vital role to play. Universities and teacher training institutes can contribute to the co-construction of evidence-based educational tools and to the training of a new generation of professionals who are equipped to address the intersection of genetics, education, and public health. Moreover, interdisciplinary research initiatives can generate the data needed to guide national strategies and to evaluate the long-term impact of intersectoral interventions.
Civil society organizations, including youth associations, parent groups, and patient advocacy networks, bring community knowledge, lived experience, and outreach capacity that are indispensable for grounding interventions in local realities. Their participation ensures that policies and programs are responsive to the concerns and expectations of the populations they intend to serve. They can also act as powerful mediators between institutions and communities, helping to build trust, reduce stigma, and promote active engagement in genetic health education.
Religious and cultural institutions represent another important, yet often overlooked, stakeholder. Given the centrality of marriage and family life in Tunisian society, and the influence of religious and traditional authorities on social norms, their involvement can facilitate the acceptance of preventive measures such as premarital screening and genetic counseling. Intersectoral collaboration should therefore include dialogue with these actors to ensure that public health messages are communicated in ways that are culturally respectful and socially legitimate. Ultimately, the prevention of thalassemia and the promotion of genetic health literacy must be framed as a shared societal objective. It is only through coordinated intersectoral collaboration that structural, institutional, and cultural barriers can be effectively addressed.
This study serves as a call to action for national and local decision-makers to invest in integrated policies that cut across traditional sectoral boundaries. By fostering synergies among education, health, research, civil society, and cultural institutions, Tunisia, and other countries facing similar public health challenges, can build a more resilient, equitable, and informed system of hereditary disease prevention.
Limits
Limitations include convenience sampling and self-report biases, as noted previously. The COVID-19 pandemic further impacted reliability, with school closures reducing participation (n = 356/500 targeted) and remote learning limiting interviewer-student interaction. Pandemic-related stress may have influenced responses, potentially amplifying reported knowledge gaps (e.g., 35% identified thalassemia as hereditary) or stigma (e.g., 42% rural students linked it to shame), posing challenges to generalizability.
Due to the restrictions imposed by COVID-19, we opted for a convenience random sampling strategy, requiring parental consent as well as approval from school directors and teachers to conduct our study in classrooms. Despite respecting the sample size determined by the Solvin formula, the sampling was limited to two public schools in urban and rural areas, which may affect the generalizability of the results. A larger-scale longitudinal survey could confirm our findings. Additionally, our results are based on self-reported data collected by teachers and are therefore subject to social desirability bias.
Conclusion
By situating thalassemia prevention within the broader framework of health literacy and educational equity, this study addresses a critical and underexplored gap in the literature, namely, the intersection of genetic disease prevention, adolescent education, and culturally responsive health promotion in North Africa. It demonstrates that addressing hereditary conditions such as thalassemia cannot be reduced to biomedical strategies alone; it requires cultivating an emotionally engaged and socially empowered youth population capable of making informed, autonomous, and culturally appropriate health decisions. In Tunisia, as in many Global South contexts, thalassemia prevention offers a valuable lens through which to interrogate broader questions of social justice, civic responsibility, and the transformative role of education in building equitable health systems. However, the current educational framework remains ill-equipped to meet this challenge.
Our findings show that the existing biology curriculum in Tunisian secondary schools does not foster meaningful or comprehensive understanding of genetic conditions. Students lack the conceptual and emotional tools necessary to recognize thalassemia as a serious public health issue. Misconceptions, particularly the conflation of thalassemia with iron deficiency anemia, are widespread, weakening the perceived urgency of preventive measures. Among humanities-track students, the disease is often trivialized or viewed as irrelevant, while even science-track students struggle to translate fragmented genetic knowledge into actionable understanding due to a lack of contextual and emotionally engaging learning approaches.
Despite these educational shortcomings, our data reveal a strong latent potential for empathy and prosocial motivation among Tunisian adolescents, even in the absence of formal health education. This highlights an urgent opportunity for intervention. To capitalize on this potential, we propose a stepwise roadmap for implementation, beginning with pilot programs in selected schools that integrate interactive, interdisciplinary learning modules on thalassemia and other hereditary conditions. These modules should be co-developed with local NGOs to ensure cultural relevance and contextual appropriateness. The second step involves systematic evaluation of these pilots to generate evidence for scalability. Based on this evidence, national curriculum updates can be initiated, integrating genetics and health literacy into both scientific and literary tracks. Concurrently, targeted teacher training programs must be developed to support the pedagogical shift toward participatory, emotionally resonant, and conceptually rigorous instruction.
This roadmap aligns directly with the World Health Organization’s framework for adolescent health promotion, which emphasizes the importance of health literacy, life skills education, and the active participation of youth in shaping their own health trajectories. By embedding thalassemia prevention into this broader agenda, the study not only offers a practical contribution to national curriculum reform but also advances global efforts to empower adolescents as agents of change in public health. Through this integrative approach, linking education, health, and civic engagement, Tunisia can begin to address both the immediate challenge of thalassemia and the deeper structural inequities that shape health outcomes across generations.