Collaborators GD. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the global burden of disease study 2021. Lancet. 2023;402(10397):203–34.
Buse JB, Ginsberg HN, Bakris GL, Clark NG, Costa F, Eckel R, Fonseca V, Gerstein HC, Grundy S, Nesto RW, et al. Primary prevention of cardiovascular diseases in people with diabetes mellitus: a scientific statement from the American heart association and the American diabetes association. Diabetes Care. 2007;30(1):162–72.
Tuttle KR, Bakris GL, Bilous RW, Chiang JL, de Boer IH, Goldstein-Fuchs J, Hirsch IB, Kalantar-Zadeh K, Narva AS, Navaneethan SD, et al. Diabetic kidney disease: a report from an ADA consensus conference. Am J Kidney Dis. 2014;64(4):510–33.
Collaborators. GDaI.Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet (London England). 2020;396(10258):1204–22.
Xu Y, Lu J, Li M, Wang T, Wang K, Cao Q, Ding Y, Xiang Y, Wang S, Yang Q, et al. Diabetes in China part 1: epidemiology and risk factors. Lancet Public Health. 2024;9(12):e1089–97.
National Bureau of Statistics of China. China Statistical Yearbook. 2019. Beijing:Peking union medical college publishing house;2019. https://www.stats.gov.cn/sj/ndsj/2019/indexeh.htm
Wang L, Gao P, Zhang M, Huang Z, Zhang D, Deng Q, Li Y, Zhao Z, Qin X, Jin D, et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA. 2017;317(24):2515–23.
Wang L, Peng W, Zhao Z, Zhang M, Shi Z, Song Z, Zhang X, Li C, Huang Z, Sun X, et al. Prevalence and treatment of diabetes in China, 2013–2018. JAMA. 2021;326(24):2498–506.
Chinese Diabetes Society. Guideline for the prevention and treatment of diabetes mellitus in China (2024 edition). Chin J Diabetes Mellitus. 2024;17(01):16–139.
Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, Peters AL, Tsapas A, Wender R, Matthews DR. Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American diabetes association (ADA) and the European association for the study of diabetes (EASD). Diabetes Care. 2012;35(6):1364–79.
Committee on Quality of Health Care in America, Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academies; 2001.
Faiman B, Tariman JD. Shared decision making: improving patient outcomes by understanding the benefits of and barriers to effective communication. Clin J Oncol Nurs. 2019;23(5):540–2.
Jaeken J, Billiouw C, Mertens L, Van Bostraeten P, Bekkering G, Vermandere M, Aertgeerts B, van Mileghem L, Delvaux N. A systematic review of shared decision making training programs for general practitioners. BMC Med Educ. 2024;24(1):592.
Davidson KW, Mangione CM, Barry MJ, Nicholson WK, Cabana MD, Caughey AB, Davis EM, Donahue KE, Doubeni CA, Kubik M, et al. Collaboration and shared decision-making between patients and clinicians in preventive health care decisions and US preventive services task force recommendations. JAMA. 2022;327(12):1171–6.
Elwyn G, Edwards A, Kinnersley P, Grol R. Shared decision making and the concept of equipoise: the competences of involving patients in healthcare choices. Br J Gen Practice: J Royal Coll Gen Practitioners. 2000;50(460):892–9.
Shay LA, Lafata JE. Where is the evidence? A systematic review of shared decision making and patient outcomes. Med Decis Making. 2015;35(1):114–31.
Kaplan SH, Greenfield S, Ware JE. Jr. Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care. 1989;27(3 Suppl):S110–127.
Bruch JD, Khazen M, Mahmic-Kaknjo M, Légaré F, Ellen ME. The effects of shared decision making on health outcomes, health care quality, cost, and consultation time: an umbrella review. Patient Educ Couns. 2024;129:108408.
Wang MJ, Hung LC, Lo YT. Glycemic control in type 2 diabetes: role of health literacy and shared decision-making. Patient Prefer Adherence. 2019;13:871–9.
Yao M, Finnikin S, Cheng KK. Call for shared decision making in china: challenges and opportunities. Z Fur Evidenz Fortbild Und Qualitat Im Gesundheitswesen. 2017;123–124:32–5.
Stacey D, Légaré F, Lewis K, Barry MJ, Bennett CL, Eden KB, Holmes-Rovner M, Llewellyn-Thomas H, Lyddiatt A, Thomson R, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;4(4):Cd001431.
Huang R, Gionfriddo MR, Zhang L, Leppin AL, Ting HH. Montori vm. Shared decision-making in the People’s Republic of China: current status and future directions. Patient Prefer Adherence. 2015;9:1129–41.
Rongchong H, Mingyue X, Hongzhou G. Current status and challenges of shared Decision-Making in China. Natl Med J China. 2020;100(30):2346–50.
Yunpeng T, Chengzhi L. Reflections on the practice of shared Decision-Making by clinical physicians. Med Philosophical. 2024;45(10):16–9.
Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P, Cording E, Tomson D, Dodd C, Rollnick S, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27(10):1361–7.
Légaré F, Ratté S, Stacey D, Kryworuchko J, Gravel K, Graham ID, Turcotte S. Interventions for improving the adoption of shared decision making by healthcare professionals. Cochrane Database Syst Rev. 2010;(5):Cd006732.
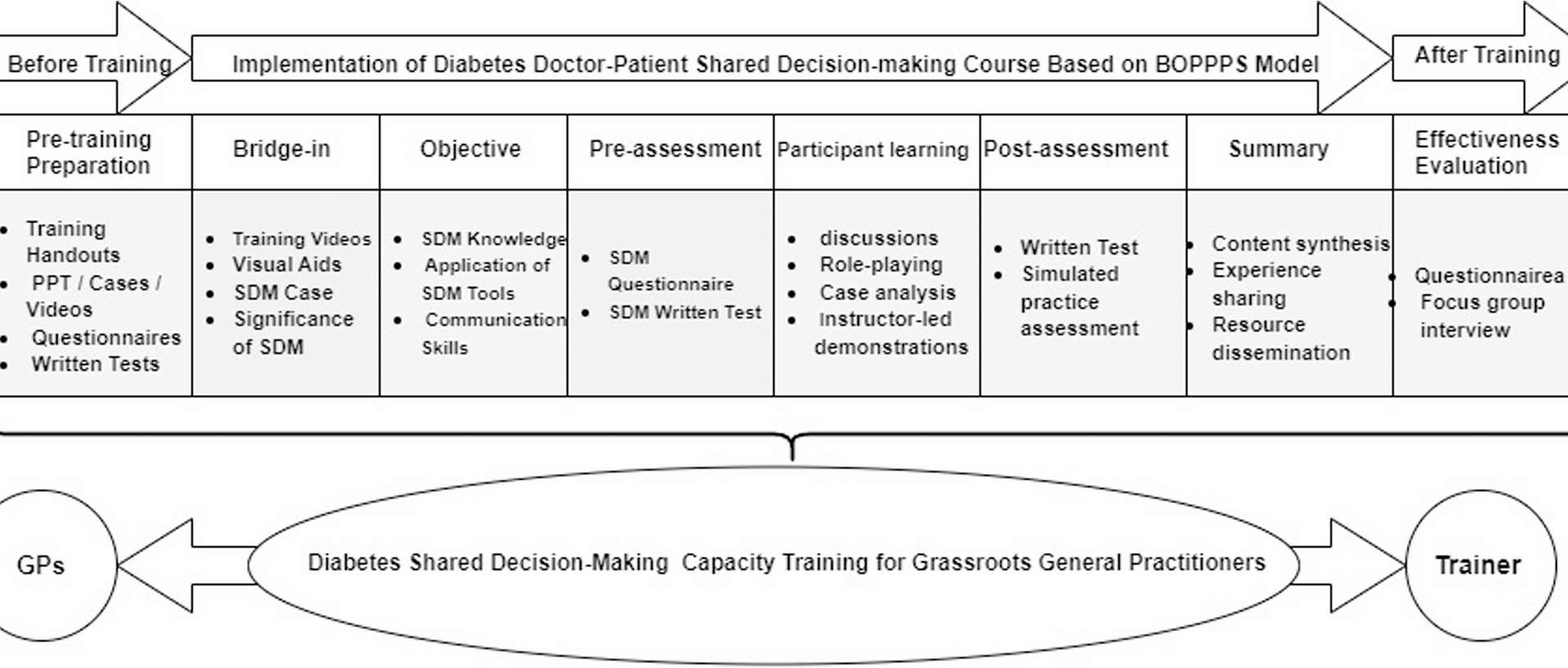
Chen L, Tang XJ, Chen XK, Ke N, Liu Q. Effect of the BOPPPS model combined with case-based learning versus lecture-based learning on ophthalmology education for five-year paediatric undergraduates in Southwest China. BMC Med Educ. 2022;22(1): 437.
Xu Z, Che X, Yang X, Wang X. Application of the hybrid BOPPPS teaching model in clinical internships in gynecology. BMC Med Educ. 2023;23(1):465.
Shen B, Chen Y, Wu Y, Lan Y, He X, Wang N, Liu J, Yu Y. Development and effectiveness of a BOPPPS teaching model-based workshop for community pharmacists training. BMC Med Educ. 2024;24(1):293.
Manzoor I, Mukhtar F, Hashmi NR. Medical students’ perspective about role-plays as a teaching strategy in community medicine. J Coll Physicians Surgeons–Pakistan: JCPSP. 2012;22(4):222–5.
Health Xicheng. The district health commission collaborates with Peking University Hospital and the Peking University Health Science Center to innovate training methods and enhance the capacity building of community general practitioners. 2024.https://www.sohu.com/a/762105051121106842. Accessed 02 Dec.2024.
Xicheng District People’s Government of Beijing Municipality. 2023 Statistical Yearbook (Permanent Population for the Year 2022). 2023. https://www.bjxch.gov.cn/xcsj/tjnj/2023tjnj.html. Accessed 02 Dec.2024.
Mukhalalati BA, Taylor A. Adult learning theories in context: a quick guide for healthcare professional educators. J Med Educ Curric Dev. 2019;6:2382120519840332.
NICE: Type 2 diabetes: agreeing my blood glucose (HbA1c) target patient decision aid. ©NICE2022.Last updated February 2022. https://www.nice.org.uk/Guidance/ng28/resources/patient-decision-aid-pdf-2187281198
Branda ME, LeBlanc A, Shah ND, Tiedje K, Ruud K, Van Houten H, Pencille L, Kurland M, Yawn B, Montori VM. Shared decision making for patients with type 2 diabetes: a randomized trial in primary care. BMC Health Serv Res. 2013;13:301.
NICE: Statin decision aid: Should I take a statin? Retrieved fromhttps://www.nice.org.uk/guidance/ng238/resources/patientdecisionaidonshouldItakeastatinpdf-243780159.
Kriston L, Scholl I, Hölzel L, Simon D, Loh A, Härter M. The 9-item shared decision making questionnaire (SDM-Q-9). Development and psychometric properties in a primary care sample. Patient Educ Couns. 2010;80(1):94–9.
Luo B, Xiao S. Reliability and validity for Chinese version of the 9-item shared decision making questionnaire. Zhong Nan Da Xue Xue Bao Yi Xue ban = J Cent South Univ Med Sci. 2019;44(7):823–9.
Scholl I, Kriston L, Dirmaier J, Buchholz A, Härter M. Development and psychometric properties of the shared decision making questionnaire–physician version (SDM-Q-Doc). Patient Educ Couns. 2012;88(2):284–90.
Luo B, Xiao S. Reliability and validity of Chinese version of shared decision making questionnaire-physician version. Chin J Clin Psychol. 2019;27(1):59–62.
Byrne D. A worked example of Braun and Clarke’s approach to reflexive thematic analysis. Qual Quant. 2022;56(3):1391–412. https://doi.org/10.1007/s11135-021-01182-y.
Nestel D, Tierney T. Role-play for medical students learning about communication: guidelines for maximising benefits. BMC Med Educ. 2007;7:3.
Nair BT. Role play – an effective tool to teach communication skills in pediatrics to medical undergraduates. J Educ Health Promot. 2019;8:18.
Chan PG, Schaheen LW, Chan EG, Cook CC, Luketich JD, D’Cunha J. Technology-enhanced simulation improves trainee readiness transitioning to cardiothoracic training. J Surg Educ. 2018;75(5):1395–402.
Lavanya SH, Kalpana L, Veena RM, Bharath Kumar VD. Role-play as an educational tool in medication communication skills: students’ perspectives. Indian J Pharmacol. 2016;48(Suppl 1):S33–6.
Ziv A, Ben-David S, Ziv M. Simulation based medical education: an opportunity to learn from errors. Med Teach. 2005;27(3):193–9.
Rhondali W, Nguyen LM, Peck M, Vallet F, Daneault S, Filbet M. Description of a teaching method for research education for palliative care healthcare professionals. Palliat Support Care. 2015;13(2):249–54.
Khan M, Kamal AK, Pasha O, Islam M, Azam I, Virk A, Nasir A, Andani A, Jan M, Akhtar A, et al. Study protocol: validation and adaptation of community-worker-administered stroke symptom questionnaire in a Periurban Pakistani community to determine disease burden. J Vasc Interv Neurol. 2015;8(1):1–10.
AlKahtani RN, Alnufaiy BM, Albaijan RS, Alnafaiy SM, Elfakhri FM, Aljudaibi SM. Comparing the efficacy of live vs. video instructional demonstrations in dental education: a systematic review and meta-analysis. BMC Med Educ. 2025;25(1):108.
Abu Arqub S, Al-Shehri NA, Meyer S, Asefi S, Al-Moghrabi D. The effectiveness of technology-enhanced learning in prosthodontic education: a systematic review. Eur J Dent Education: Official J Association Dent Educ Europe. 2024;28(4):995–1015.
Atwal PK, Kwatra G, Jain R, Dua KK, Khanna S, Gupta VV. To develop and implement a preclinical operative dentistry module to enhance class-II cavity preparation training. Int J Appl Basic Med Res. 2024;14(4):273–7.
Dash S, Kamath U, Rao G, Prakash J, Mishra S. Audio-visual aid in teaching “fatty liver”. Biochem Mol Biology Education: Bimon Publication Int Union Biochem Mol Biology. 2016;44(3):241–5.
Taslibeyaz E, Aydemir M, Karaman S. An analysis of research trends in articles on video usage in medical education. Educ Inf Technol. 2017;22(3):873–81.
O’Connor AM, Stacey D, Entwistle V, Llewellyn-Thomas H, Rovner D, Holmes-Rovner M, Tait V, Tetroe J, Fiset V, Barry M et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2003;(2):Cd001431.
Breslin M, Mullan RJ, Montori VM. The design of a decision aid about diabetes medications for use during the consultation with patients with type 2 diabetes. Patient Educ Couns. 2008;73(3):465–72.
Weymiller AJ, Montori VM, Jones LA, Gafni A, Guyatt GH, Bryant SC, Christianson TJ, Mullan RJ, Smith SA. Helping patients with type 2 diabetes mellitus make treatment decisions: statin choice randomized trial. Arch Intern Med. 2007;167(10):1076–82.
Mullan RJ, Montori VM, Shah ND, Christianson TJ, Bryant SC, Guyatt GH, Perestelo-Perez LI, Stroebel RJ, Yawn BP, Yapuncich V, et al. The diabetes mellitus medication choice decision aid: a randomized trial. Arch Intern Med. 2009;169(17):1560–8.
Légaré F, Moumjid-Ferdjaoui N, Drolet R, Stacey D, Härter M, Bastian H, et al. Core competencies for shared decision making training programs: insights from an international, interdisciplinary working group. J Contin Educ Health Prof. 2013;33(4):267–73.
Körner M, Ehrhardt H, Steger AK, Bengel J. Interprofessional SDM train-the-trainer program “Fit for SDM “: provider satisfaction and impact on participation. Patient Educ Couns. 2012;89(1):122–8.