Patients and study design
A review of the medical records of individuals who underwent immediate placement of dental implants following injuries to their teeth was performed. During the period spanning from January 2014 to December 2021, patients who participated in this research were treated at the Department of Periodontology and Oral Implantology, Stomatological Hospital, Southern Medical University (Guangzhou, China). The patients were selected according to specific inclusion and exclusion criteria.
The established criteria were as follows:
1.
Presence of a maxillary anterior tooth (canine or incisor) that has been damaged due to trauma in the past two weeks;
2.
Underwent immediate dental implant placement;
3.
The surrounding teeth have probing depths no deeper than 4 mm;
4.
Good oral hygiene
The exclusion criteria are outlined below:
1.
Factors such as a complex medical history including alcohol consumption, smoking habits, or overall poor health that could impact the study results were considered.
2.
Having a dental history involving bruxism, abnormal habits, and/or an unstable posterior occlusion;
3.
Noncompliance.
All study participants underwent immediate dental implant placement in the esthetic zone, with a portion of them receiving immediate temporary restorations. Following a healing period of 6 months or more, the final restorations were carried out. All patients provided detailed informed consent before treatment
Clinical procedure
During the initial visit, a cranial cone beam computed tomography (CBCT) scan was conducted to assess the injured teeth and rule out any potential bone fractures. The subsequent evaluation of the injured tooth involved consultation with an oral surgeon, prosthodontist, and endodontist to determine its preservation feasibility.
If the wounded tooth could not be kept and the patient Chose to have an oral implant, the patient received standard treatment planning and consented to the treatment. In the case of a damaged tooth where the buccal bone wall remains intact and there is sufficient residual bone, minimally traumatic extraction was carefully carried out, and the implant was immediately inserted into the fresh extraction socket in a flapless manner. All implants were placed 1–2 mm below the edge of the socket, to compensate the potential resorption of the buccal wall. The specific implant system utilized in this study was the Zimmer Biomet TSV (Warsaw, Indiana, U.S.). The diameter of the implant was 3.7 mm in all patients. Bone particles (Bio-oss, Geistlich Pharma AG, Wolhusen, Switzerland) were used to fill the space between the implant and the buccal wall.
Patients were instructed to use the broad-spectrum antibiotics cefuroxime (0.25 g, twice per day for 3 days) or roxithromycin (0.15 g, twice per day for 3 days) in the case of cefaclor allergy. 0.5% chlorhexidine was utilized for mouthwash three times daily during the first 2 weeks. The patient received one dose of dexamethasone (5 mg) orally post-surgery. The ice packs were used in the first 48 h after surgery. Patients were advised to consider nonsteroidal anti-inflammatory drugs in cases of pain. Sutures were removed after one week.
For some of the patients with an insertion torque greater than 35 N×cm, a temporary restoration was prepared and placed immediately after surgery. Some temporary restorations were prepared with the fractured crown of the patient before surgery (see Fig. 1). In cases where immediate provisionalization was not performed, prefabricated healing abutments were placed on the implants. The clinical outcomes were subsequently analyzed and compared between patients who received immediate provisionalization and those who did not. A minimum of four months after the surgery date, the final implant impression was taken using polyether silicone rubber (Minnesota Mining and Manufacturing Company, 3 M, Maplewood, Minnesota, U.S.). A definitive customized crown with gingival emergence established by the provisional restoration was fabricated via Hex-Lock Contour Abutments (Zimmer Biomet). The definitive abutment was torqued to 30 N/cm (manufacturer’s recommendation, Zimmer Biomet). The zirconia coping and zirconia crown, which are highly esthetic and natural-looking, were cemented (RelyX U200, 3 M).
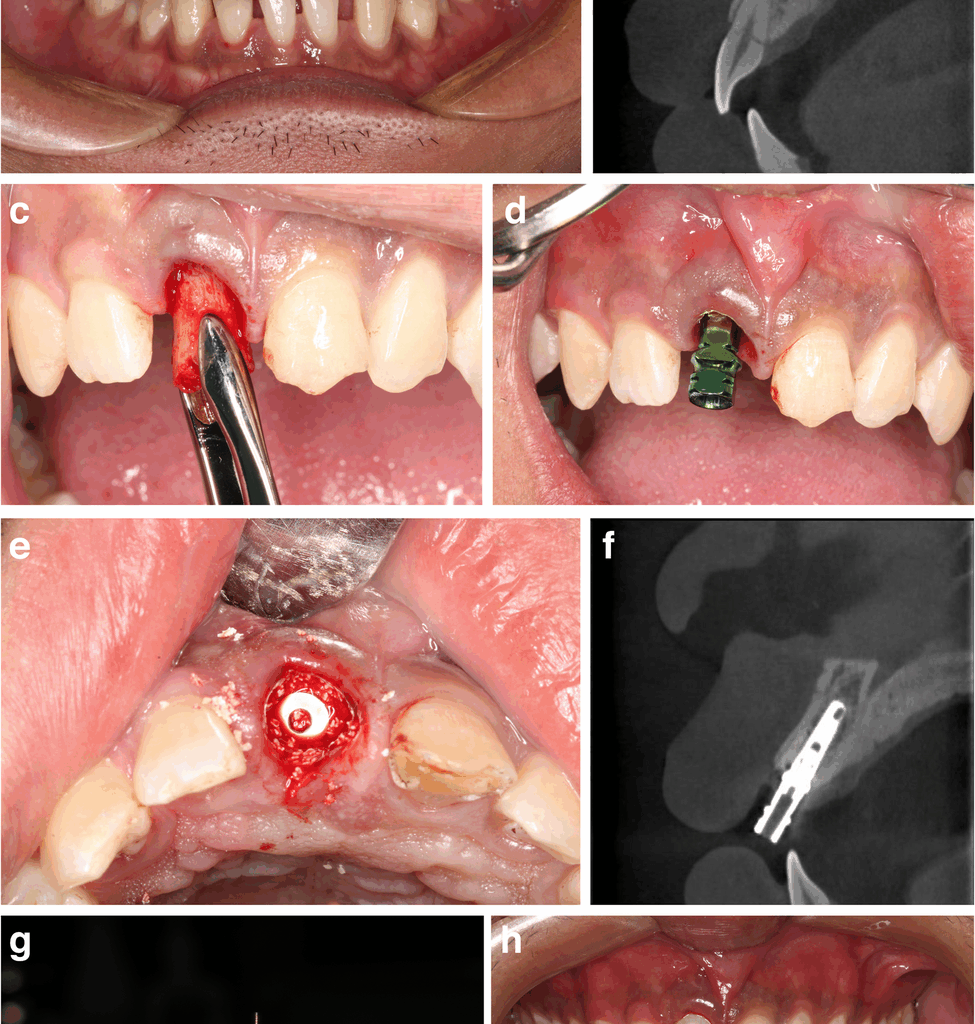
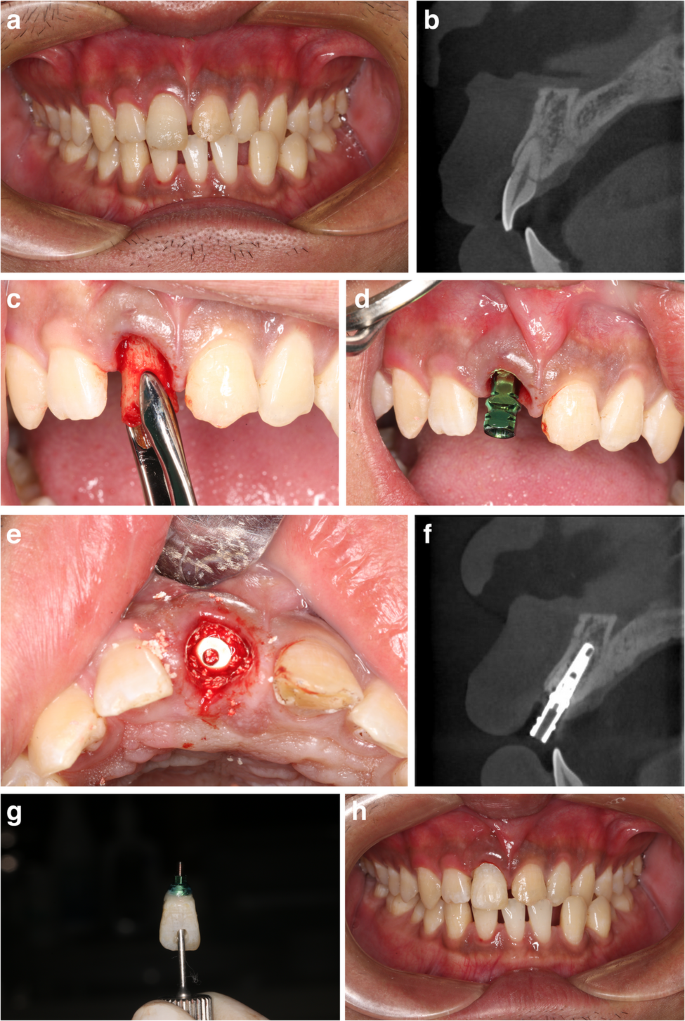
The patient fell off the bicycle and broke his right upper incisor two days prior. CBCT examination revealed that the tooth was fractured in the neck. The treatment plan was to extract tooth 11, immediately insert an implant (Zimmer TSV, 3.7 mm in diameter, 13 mm in length), and perform immediate restoration with the extracted crown. Front view (a) and parasagittal CBCT slice of 11 before implant surgery b. Surgical process: (c) tooth extraction; (d) implant placement; (e) filling of the jumping gap with bone particles (Bio-oss). f parasagittal CBCT slice of 11 after implant surgery. g the temporary crown. h front view after immediate restoration. One year after the final restoration, the front view (i) and parasagittal CBCT slice of 11 (j) are shown
Data collection
All examinations and data collection were performed by the same examiner. Assessments were conducted at the time of implant insertion (T0), upon completion of the final restoration (T1), and twelve months after final restoration (T2). The recorded variables included the success or failure of the implant, the marginal bone level, pink/white esthetic scores (PES/WES), and the satisfaction of patients with esthetics. The buccal bone wall thickness and jumping gap distance were measured at the level of implant shoulder through CBCT images at T0.
Marginal bone change
Sequential periapical radiographs and the long cone parallel technique were utilized to assess the changes in the marginal bone. To achieve standardization in angulation and film position to the X-ray beam, an occlusal jig was employed. Marginal bone levels of the implants were measured on the mesial and distal aspects at T1 and T2 under 10x magnification, with accuracy to the nearest 1 mm. The reference point for measurement was established at the apical corner of the implant shoulder, and subsequently, the alterations were calculated. A positive value is denoted when there is more coronal implant–bone contact in comparison to the reference point; conversely, a negative value is assigned when implant–bone contact is more apical than the reference point.
Esthetic assessment
The esthetic scores were objectively evaluated by two blinded prosthodontists who were not involved in the treatment.
Pink esthetic score
The pink esthetic score [10] was used to assess all patients, and consisted of seven variables: the mesial papilla, distal papilla, soft tissue level, soft tissue contour, alveolar process deficiency, soft tissue color, and soft tissue texture. The scoring system assigned a value of 0, 1, or 2 to each factor. The scale ranged from 0, representing the least favorable outcome, to 2, indicating the most favorable outcome for every variable; hence, achieving a total of 14 would signify optimal peri-implant soft tissues. The threshold for clinically acceptable soft tissues was set at 8. A score of 12 or higher was considered to indicate almost perfect peri-implant soft tissues, as previously described.
White esthetic score
The White Esthetic Score [11] was utilized to evaluate all patients, encompassing five different variables: the general shape of the teeth, the contour of the teeth, the color of the teeth (including hue and value), the texture of the tooth surface, and the level of translucence. A scoring system of 0, 1, or 2 was applied to each parameter. The scores ranged from the least favorable outcome, represented by 0, to the most favorable outcome, represented by 2, for every variable. The esthetics of the implant-supported tooth were compared with those of the contralateral reference tooth. When the closest resemblance to the contralateral tooth was achieved, a maximum score of 10 was awarded. The thresholds for a clinically acceptable or an almost perfect implant crown were set at 6 and 9, respectively.
Patient esthetic satisfaction
During the one-year follow-up evaluation, an evaluation was conducted to assess the satisfaction of each patient with the overall implant treatment through a subjective outcome questionnaire. The questionnaire comprised five inquiries and a visual analogue scale (VAS) spanning 10 centimeters, ranging from 0 (representing the least favorable outcome) to 10 (representing the most favorable outcome) for evaluating patient content. Each patient’s response to the listed inquiries was used to compute an average VAS score.
1.
How do you evaluate the shape of your dental implant tooth?
2.
How do you evaluate the color of your dental implant tooth?
3.
How do you evaluate the shape of the gum around your dental implant tooth?
4.
How do you evaluate the color of the gum around your dental implant tooth?
5.
What are your overall feelings towards your dental implant tooth?
Data analysis
Means and standard deviations were computed for each clinical parameter during each specific timeframe. GraphPad Prism (version 10, GraphPad Software, Boston, MA) was utilized to analyze the data. The Wilcoxon signed-rank test was adopted to measure the marginal bone changes in the first year. Two-tailed t tests for independent samples were used to define the relationships between potentially relevant factors (i.e., age, sex, gingival biotype, buccal bone wall thickness, jumping gap and immediate provisionalization) and esthetic scores. The Spearman correlation coefficient was used to assess the association between objective esthetic scores and patient esthetic satisfaction (VAS). The Mann‒Whitney test was used to compare the VAS scores of patients in different groups according to their potentially relevant factors. Statistical significance was denoted when P < 0.05.