Acute respiratory failure (ARF) is characterized by a triad of clinical signs, radiographic findings, and gas exchange abnormalities. Most patients present with newly developing or worsening respiratory symptoms over a period of seven days. Severe acute respiratory failure is marked by respiratory distress, significant tachypnea, labored breathing, and the use of accessory respiratory muscles [11]. Various patterns of pulmonary infiltrates may be observed, with diffuse bilateral infiltrates being the most common [12].
The main causes of acute respiratory failure can be categorized into non-infectious and infectious factors. In 2020, Azoulay et al. noted that among infectious causes in immunocompromised patients, severe bacterial pneumonias are the most prevalent, followed by viral, fungal, and, less commonly, parasitic infections [13]. The three most significant causes of fungal pulmonary infections are Pneumocystis jirovecii, Aspergillus spp., and Cryptococcus spp [14]. Although T. marneffei has been reported to cause sepsis [15], there have been no documented cases of respiratory failure associated with this pathogen, highlighting the need for greater awareness of its potential impact.
Talaromycosis was once thought to affect only patients with human immunodeficiency virus (HIV), with disseminated disease linked to advanced HIV infection and localized disease occurring in non-HIV-infected individuals. However, the number of HIV-negative patients, particularly those who are immunocompromised, with talaromycosis is increasing [16]. Evidence is emerging that both localized respiratory and disseminated forms of the disease can develop in both HIV-positive and HIV-negative hosts, and the immune status of these individuals cannot be accurately inferred from clinical presentation [17, 18].
The exact route of transmission for pathogenic T. marneffei to humans remains unclear. Studies of wild bamboo rats have shown the highest burden of disease in the lungs (83.3%), followed by the liver (33.3%) and spleen (33.3%) [19]. It is commonly believed that human inhalation of airborne conidia from environmental sources, such as soil, leads to the infection, with subsequent dissemination to other body sites [20]. Consequently, lung infection is considered a critical initial step in the onset of the disease, with pulmonary talaromycosis serving as a key indicator of its immunopathogenesis [21]. Despite this, there are fewer reports of localized infections compared to disseminated infections, possibly due to the short duration of disease progression and the challenges in diagnosing pulmonary talaromycosis.
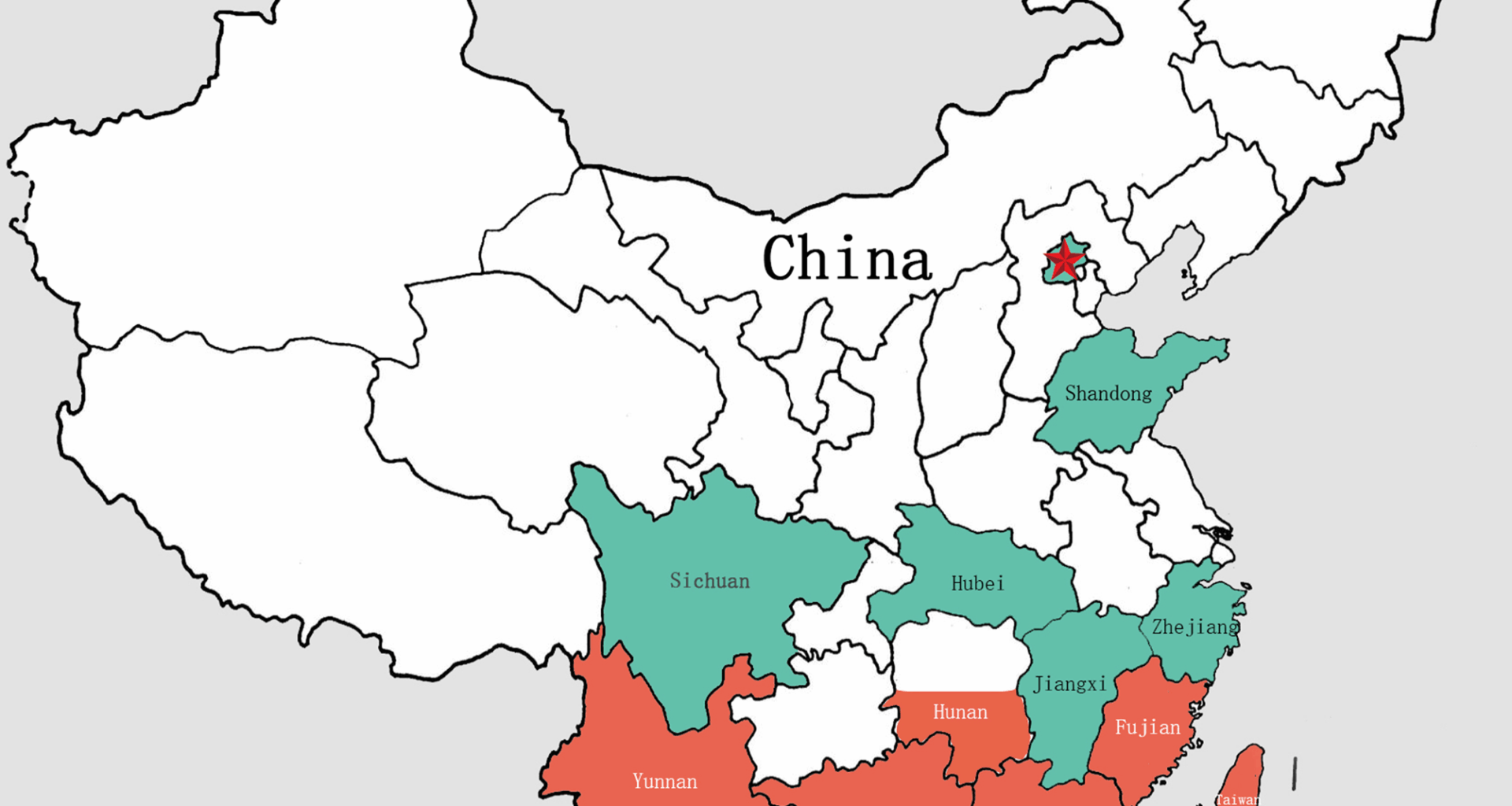
This patient, born in Shandong, had a brief history of living in an epidemic area prior to the onset of the disease, which played a key role in the diagnosis. The patient presents with a clinically rare localized form of the disease, complicated by severe respiratory failure. Pulmonary imaging in cases of T. marneffei typically reveals a range of findings, including patchy consolidation, nodular shadows, cavitary lesions, diffuse miliary nodules, ground-glass opacities, mediastinal and hilar lymphadenopathy, pleural thickening, and pleural effusion. These findings often coexist with multiple lesions, exhibiting diverse patterns without clear distinguishing characteristics. Various types of pulmonary infiltrates may be observed, with diffuse bilateral infiltrates being the most common in respiratory failure (RF) [12]. Failure to identify the underlying cause of acute respiratory failure (ARF) significantly increases the risk of mortality [22].
The possible reasons for the patient’s infection seem confined to the lungs: ① Immunosuppression was not evident in this patient. His HIV test was negative, and lymphocyte subset analysis was normal. We screened for potential immunosuppressive factors, including tumors, rheumatological conditions, and autoimmune diseases, but all results were negative. Another common cause of immune deficiency is anti-IFN-γ autoantibodies. The association between these antibodies and T. marneffei infection was first reported in 2010. In patients with anti-IFN-γ autoantibodies, T. marneffei infections typically manifest as fever of unknown origin, cervical lymphadenitis, and/or mild symptomatic infection, often with positive serology [23]. Reports of T. marneffei infections linked to anti-IFN-γ autoantibodies are increasing, but we did not assess the level of anti-IFN-γ autoantibodies in this case, as the patient’s symptoms did not align with the common clinical presentations. ② The patient’s diagnosis was made in a timely manner. It took 25 days from symptom onset to diagnosis, which may have prevented the pathogen from disseminating throughout the body.
Pulmonary talaromycosis shares many clinical features with tuberculosis, non-tuberculous mycobacterial infections, cancer, and pneumocystis pneumonia, which often leads to misdiagnosis, delays in treatment, further spread of the infection, and poor patient outcomes. As a result, histopathological examination or culture of T. marneffei is considered the gold standard for diagnosis. To confirm the diagnosis, we performed regular sputum culture, fungal culture, bronchoalveolar lavage (BAL) fluid culture, BAL fluid metagenomic next-generation sequencing (mNGS), and percutaneous lung biopsy.Unfortunately, we did not perform mNGS testing on the biopsy tissue and were unable to confirm the presence of penicillium marneffei infection in the patient through tissue analysis.
Recently, an HIV-negative patient diagnosed with mNGS through percutaneous lung biopsy was reported,this patient has no respiratory symptoms, with bone pain as the main clinical manifestation [2]. Interestingly, while an increasing number of reports suggest that mNGS may be an effective tool for early diagnosis of T. marneffei infection, in this case, the patient had a negative mNGS result but a positive sputum fungal culture. This finding was puzzling, as T. marneffei does not typically colonize the lungs. We examined the background microorganisms listed in the mNGS report, but T. marneffei was not detected. According to multiple previous studies, mNGS is generally more sensitive than sputum fungal culture. However, in this case, the mNGS result was negative.
We have reviewed the literature and found that there have been similar case reports in the past.Among the 32 T. marneffei infected patients studied by Chen Qiuhua [24], 7 were negative for mNGS detection and positive for culture. The reasons may be related to antifungal therapy, thick fungal cell walls, large genomes, and some fungi being engulfed by phagocytic cells. Bipolar fungi such as Nepenthes mirabilis are intracellular bacteria that can only be detected after a certain period of time in macrophages to release nucleic acids, which can easily lead to delayed mNGS positivity.At the same time, the article mentioned that 21 patients underwent pathological examination with PAS staining, and only 1 patient had lymph node pathology indicating T. marneffei infection.
Liang Tianwei [25] also discussed the limitations of NGS: in her study, a BALF sample confirmed to be T. marnefei after 30 days of cultivation had a negative mNGS report for parallel testing. It is speculated that the low T. marnefei loading in the sample may be the reason.
The possible reasons for this include:
① Technical issues with the mNGS detection process.The difficulty of mNGS detection of T. marneffei may be due to its intracellular fungal nature. Due to its intracellular growth characteristics, T. marneffei releases less extracellular nucleic acid, making it difficult to break through the cell wall during nucleic acid extraction.
② The samples had to be sent to Nanjing for testing. Although they were refrigerated throughout the process, the delay may have affected the detection of the pathogen.
T. marneffei* infection is rarely reported in patients without a history of travel to or residence in epidemic areas, though a recent case has been documented. This complicates the diagnosis and highlights the need for multi-channel and multi-sample testing as a priority in such cases.
Currently, there is no standardized treatment protocol for T. marneffei infection in HIV-negative patients, and optimal treatment for localized respiratory disease has not been clearly defined. Current treatment approaches are based on studies involving HIV-positive patients, which include two weeks of induction therapy with amphotericin B followed by long-term consolidation and maintenance treatment with itraconazole [26]. Voriconazole has also been used successfully in treating T. marneffei in HIV-negative patients, with confirmed safety and efficacy [27, 28]. In cases where T. marneffei involves the tracheobronchial tree, nebulized inhalation or intratracheal instillation of amphotericin B, similar to the treatment of invasive pulmonary aspergillosis, is recommended [29]. However, there is no unified standard for antifungal treatment in HIV-negative patients, and most treatment regimens involve long-term therapy.
Due to difficulties in obtaining amphotericin B and the patient’s rapid deterioration, we initially administered voriconazole as antifungal therapy, rather than the recommended amphotericin B induction therapy. However, according to the national guidelines of China, amphotericin B remains the first-line recommendation for the induction treatment of talaromycosis. The clinical treatment guidelines, which are often based on the treatment of HIV-positive talaromycosis patients, advise intravenous amphotericin B (0.6 mg/kg/day), followed by oral itraconazole (400 mg/day) for maintenance therapy [30].
Given the patient’s condition, we closely monitored liver and kidney function and adopted a strategy of gradually increasing the dosage of amphotericin B in combination with voriconazole. After nearly two weeks of voriconazole treatment, amphotericin B was added at a dose of 25 mg (0.3125 mg/kg) once daily for four days. At this point, we discontinued voriconazole.
Diagnosing T. marneffei in HIV-negative patients is challenging, and many are already experiencing systemic spread or organ failure by the time of diagnosis. Some patients cannot tolerate high doses of amphotericin B. Although the combination of antifungal drugs increases the risk of hepatorenal toxicity, the patient’s respiratory distress was worsening rapidly, and we were concerned about further deterioration while increasing the amphotericin B dose. Thus, we opted for combination therapy while closely monitoring liver and kidney function.
Unfortunately, the patient chose to discontinue the medication on their own after a follow-up visit and did not undergo the recommended chest CT scan. However, in a three-year follow-up by telephone, the patient reported that they are still engaged in physical labor and have not experienced a relapse.
Before starting antifungal treatment, the patient’s condition worsened significantly. At one point, we considered intubation, but the patient’s family declined the procedure. As a result, we focused on maintaining the patient’s oxygen levels to the best of our ability. Given the ongoing debate about the effectiveness of different oxygen therapies for acute respiratory failure, we employed various methods, including Venturi mask oxygen therapy, non-invasive ventilation, and high-flow nasal cannula therapy, while also ensuring adequate nutritional support.
Although respiratory failure can be caused by many common diseases, cases of respiratory failure due to this condition are rarely reported in northern China. The patient had a clear history of living in an endemic area, and the final diagnosis was confirmed through culture results. With increasing population movement and rising reports of T. marneffei infections in HIV-negative patients, it is important for physicians in non-endemic regions to remain vigilant and consider this diagnosis.