GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet Neurol. 2021;20(10):795–820.
Cushing H. Concerning a definite regulatory mechanism of vasomotor centre which controls blood pressure during cerebral compression. Bull Johns Hopkins Hosp. 1901;12:290–2.
Cushing H. Peptic ulcers and the interbrain. Surg Gynecol Obstet. 1932;55:1–34.
Ziaka M, Exadaktylos A. The heart is at risk: understanding stroke-heart-brain interactions with focus on neurogenic stress cardiomyopathy-a review. J Stroke. 2023;25(1):39–54.
Busl KM, Bleck TP. Neurogenic pulmonary edema. Crit Care Med. 2015;43(8):1710–5.
Meyfroidt G, Baguley IJ, Menon DK. Paroxysmal sympathetic hyperactivity: the storm after acute brain injury. Lancet Neurol. 2017;16(9):721–9.
Podell JE, Miller SS, Jaffa MN, Pajoumand M, Armahizer M, Chen H, et al. Admission features associated with paroxysmal sympathetic hyperactivity after traumatic brain injury: a case-control study. Crit Care Med. 2021;49(10):e989–1000.
Jafari AA, Shah M, Mirmoeeni S, Hassani MS, Nazari S, Fielder T, et al. Paroxysmal sympathetic hyperactivity during traumatic brain injury. Clin Neurol Neurosurg. 2022;212:107081.
Maesaka JK, Imbriano LJ. Cerebral salt wasting is a real cause of hyponatremia: pro. Kidney360. 2023;4(4):e437–40.
Wijdicks EFM. Duck or rabbit? Cerebral salt wasting and SIADH in acute brain injury. Neurocrit Care. 2023;39(1):260–3.
Adrogué HJ, Madias NE. The syndrome of inappropriate antidiuresis. N Engl J Med. 2023;389(16):1499–509.
Wilson JE, Mart MF, Cunningham C, Shehabi Y, Girard TD, MacLullich AMJ, et al. Delirium. Nat Rev Dis Primers. 2020;6(1):90.
Aita SL, Schuler KR, Isaak SL, Borgogna NC, Moncrief GG, Hollis SD, et al. Posttraumatic stress disorder complicated by traumatic brain injury: a narrative review. SN Compr Clin Med. 2023;5(1):92.
Ressler KJ, Berretta S, Bolshakov VY, Rosso IM, Meloni EG, Rauch SL, et al. Post-traumatic stress disorder: clinical and translational neuroscience from cells to circuits. Nat Rev Neurol. 2022;18(5):273–88.
Smith DH, Johnson VE, Trojanowski JQ, Stewart W. Chronic traumatic encephalopathy – confusion and controversies. Nat Rev Neurol. 2019;15(3):179–83.
Izzy S, Chen PM, Tahir Z, Grashow R, Radmanesh F, Cote DJ, et al. Association of traumatic brain injury with the risk of developing chronic cardiovascular, endocrine, neurological, and psychiatric disorders. JAMA Netw Open. 2022;5(4):e229478.
Asim M, Amin F, El-Menyar A. Multiple organ dysfunction syndrome: contemporary insights on the clinicopathological spectrum. Qatar Med J. 2020;2020(1):22.
Barea-Mendoza JA, Chico-Fernández M, Serviá-Goixart L, Quintana-Díaz M, García-Sáez I, Ballesteros-Sanz M, et al. Associated risk factors and impact in clinical outcomes of multiorgan failure in patients with TBI. Neurocrit Care. 2023;39(2):411–8.
Åkerlund CAI, Holst A, Stocchetti N, Steyerberg EW, Menon DK, Ercole A, et al. Clustering identifies endotypes of traumatic brain injury in an intensive care cohort: a CENTER-TBI study. Crit Care. 2022;26(1):228.
Krishnamoorthy V, Temkin N, Barber J, Foreman B, Komisarow J, Korley FK, et al. Association of early multiple organ dysfunction with clinical and functional outcomes over the year following traumatic brain injury: a transforming research and clinical knowledge in traumatic brain injury study. Crit Care Med. 2021;49(10):1769–78.
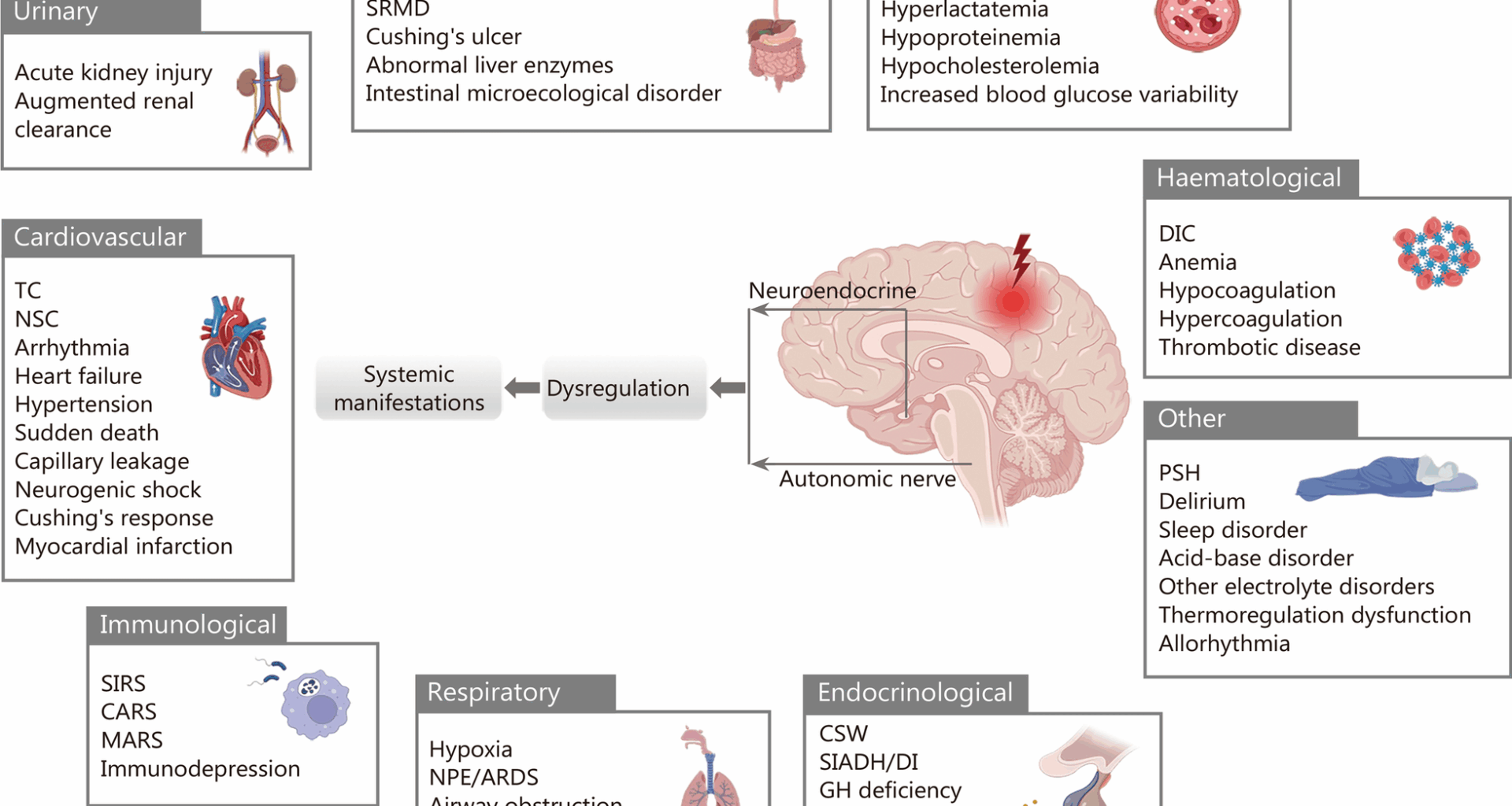
Battaglini D, De Rosa S, Godoy DA. Crosstalk between the nervous system and systemic organs in acute brain injury. Neurocrit Care. 2024;40(1):337–48.
Wongsripuemtet P, Ohnuma T, Minic Z, Vavilala MS, Miller JB, Laskowitz DT, et al. Early autonomic dysfunction in traumatic brain injury: an article review on the impact on multiple organ dysfunction. J Clin Med. 2025. https://doi.org/10.3390/jcm14020557.
Del Negro CA, Funk GD, Feldman JL. Breathing matters. Nat Rev Neurosci. 2018;19(6):351–67.
Manuel J, Färber N, Gerlach DA, Heusser K, Jordan J, Tank J, et al. Deciphering the neural signature of human cardiovascular regulation. Elife. 2020;9:e55316.
Morrison SF, Nakamura K. Central mechanisms for thermoregulation. Annu Rev Physiol. 2019;81:285–308.
Ramirez JM, Severs LJ, Ramirez SC, Agosto-Marlin IM. Advances in cellular and integrative control of oxygen homeostasis within the central nervous system. J Physiol. 2018;596(15):3043–65.
Ichiki T, Augustine V, Oka Y. Neural populations for maintaining body fluid balance. Curr Opin Neurobiol. 2019;57:134–40.
Bernal A, Zafra MA, Simón MJ, Mahía J. Sodium homeostasis, a balance necessary for life. Nutrients. 2023;15(2):395.
Barabási DL, Bianconi G, Bullmore E, Burgess M, Chung S, Eliassi-Rad T, et al. Neuroscience needs network science. J Neurosci. 2023;43(34):5989–95.
Bullmore E, Sporns O. Complex brain networks: graph theoretical analysis of structural and functional systems. Nat Rev Neurosci. 2009;10(3):186–98.
Girvan M, Newman MEJ. Community structure in social and biological networks. Proc Natl Acad Sci U S A. 2002;99(12):7821–6.
Sporns O, Honey CJ, Kötter R. Identification and classification of hubs in brain networks. PLoS ONE. 2007;2(10):e1049.
Stam CJ, van Straaten ECW. The organization of physiological brain networks. Clin Neurophysiol. 2012;123(6):1067–87.
Ravasz E, Barabási AL. Hierarchical organization in complex networks. Phys Rev E Stat Nonlin Soft Matter Phys. 2003;67(2 Pt 2):026112.
Cannon WB. The wisdom of the body. New York, W.W. Norton, 1939.
Goldstein DS. How does homeostasis happen? Integrative physiological, systems biological, and evolutionary perspectives. Am J Physiol Regul Integr Comp Physiol. 2019;316(4):R301–17.
Sennesh E, Theriault J, Brooks D, van de Meent JW, Barrett LF, Quigley KS. Interoception as modeling, allostasis as control. Biol Psychol. 2022;167:108242.
Pereira A Jr. Developing the concepts of homeostasis, homeorhesis, allostasis, elasticity, flexibility and plasticity of brain function. NeuroSci. 2021;2(4):372–82.
Bobba-Alves N, Juster RP, Picard M. The energetic cost of allostasis and allostatic load. Psychoneuroendocrinology. 2022;146:105951.
Wang S, Qin L. Homeostatic medicine: a strategy for exploring health and disease. Curr Med. 2022;1(1):16.
Schulkin J, Sterling P. Allostasis: a brain-centered, predictive mode of physiological regulation. Trends Neurosci. 2019;42(10):740–52.
Billman GE. Homeostasis: the underappreciated and far too often ignored central organizing principle of physiology. Front Physiol. 2020;11:200.
Kleckner IR, Zhang J, Touroutoglou A, Chanes L, Xia C, Simmons WK, et al. Evidence for a large-scale brain system supporting allostasis and interoception in humans. Nat Hum Behav. 2017;1:0069.
Benarroch EE. The central autonomic network: functional organization, dysfunction, and perspective. Mayo Clin Proc. 1993;68(10):988–1001.
Sklerov M, Dayan E, Browner N. Functional neuroimaging of the central autonomic network: recent developments and clinical implications. Clin Auton Res. 2019;29(6):555–66.
Thayer JF, Lane RD. A model of neurovisceral integration in emotion regulation and dysregulation. J Affect Disord. 2000;61(3):201–16.
Thayer JF, Hansen AL, Saus-Rose E, Johnsen BH. Heart rate variability, prefrontal neural function, and cognitive performance: the neurovisceral integration perspective on self-regulation, adaptation, and health. Ann Behav Med. 2009;37(2):141–53.
Porges SW. The polyvagal theory: new insights into adaptive reactions of the autonomic nervous system. Cleve Clin J Med. 2009;76(Suppl 2):S86-90.
Edlow BL, McNab JA, Witzel T, Kinney HC. The structural connectome of the human central homeostatic network. Brain Connect. 2016;6(3):187–200.
Al-Khazraji BK, Shoemaker JK. The human cortical autonomic network and volitional exercise in health and disease. Appl Physiol Nutr Metab. 2018;43(11):1122–30.
Reisert M, Weiller C, Hosp JA. Displaying the autonomic processing network in humans – a global tractography approach. Neuroimage. 2021;231:117852.
Benarroch EE. Insular cortex: functional complexity and clinical correlations. Neurology. 2019;93(21):932–8.
Tadross JA, Steuernagel L, Dowsett GKC, Kentistou KA, Lundh S, Porniece M, et al. A comprehensive spatio-cellular map of the human hypothalamus. Nature. 2025;639(8055):708–16.
Eguíluz VM, Chialvo DR, Cecchi GA, Baliki M, Apkarian AV. Scale-free brain functional networks. Phys Rev Lett. 2005;94(1):018102.
Beissner F, Meissner K, Bär KJ, Napadow V. The autonomic brain: an activation likelihood estimation meta-analysis for central processing of autonomic function. J Neurosci. 2013;33(25):10503–11.
Valenza G, Duggento A, Passamonti L, Toschi N, Barbieri R. Resting state neural correlates of cardiac sympathetic dynamics in healthy subjects. IEEE EMBC. 2019;2019(2019):4330–3.
Valenza G, Passamonti L, Duggento A, Toschi N, Barbieri R. Uncovering complex central autonomic networks at rest: a functional magnetic resonance imaging study on complex cardiovascular oscillations. J R Soc Interface. 2020;17(164):20190878.
Quadt L, Critchley H, Nagai Y. Cognition, emotion, and the central autonomic network. Auton Neurosci. 2022;238:102948.
Goldstein DS. Stress and the “extended” autonomic system. Auton Neurosci. 2021;236:102889.
Fink G. Eighty years of stress. Nature. 2016;539(7628):175–6.
Goldstein DS. Linking the extended autonomic system with the homeostat theory: new perspectives about dysautonomias. J Pers Med. 2024;14(1):123.
Schiller M, Ben-Shaanan TL, Rolls A. Neuronal regulation of immunity: why, how and where? Nat Rev Immunol. 2021;21(1):20–36.
Chan KL, Poller WC, Swirski FK, Russo SJ. Central regulation of stress-evoked peripheral immune responses. Nat Rev Neurosci. 2023;24(10):591–604.
Zhou C, Zemanová L, Zamora G, Hilgetag CC, Kurths J. Hierarchical organization unveiled by functional connectivity in complex brain networks. Phys Rev Lett. 2006;97(23):238103.
Fornito A, Zalesky A, Breakspear M. The connectomics of brain disorders. Nat Rev Neurosci. 2015;16(3):159–72.
Ge M, Ni X, Qi X, Chen S, Huang J, Kang Y, et al. Synthesizing brain-network-inspired interconnections for large-scale network-on-chips. ACM Trans Des Autom Electron Syst. 2021;27(1):1–30.
Liao X, Vasilakos AV, He Y. Small-world human brain networks: perspectives and challenges. Neurosci Biobehav Rev. 2017;77:286–300.
Newman MEJ, Girvan M. Finding and evaluating community structure in networks. Phys Rev E Stat Nonlin Soft Matter Phys. 2004;69(2 Pt 2):026113.
Gallen CL, D’Esposito M. Brain modularity: a biomarker of intervention-related plasticity. Trends Cogn Sci. 2019;23(4):293–304.
Pan RK, Sinha S. Modular networks emerge from multiconstraint optimization. Phys Rev E Stat Nonlin Soft Matter Phys. 2007;76(4 Pt 2):045103.
Sporns O, Betzel RF. Modular brain networks. Annu Rev Psychol. 2016;67:613–40.
Stam CJ. Modern network science of neurological disorders. Nat Rev Neurosci. 2014;15(10):683–95.
Ahn YY, Bagrow JP, Lehmann S. Link communities reveal multiscale complexity in networks. Nature. 2010;466(7307):761–4.
Wig GS. Segregated systems of human brain networks. Trends Cogn Sci. 2017;21(12):981–96.
Godoy LD, Rossignoli MT, Delfino-Pereira P, Garcia-Cairasco N, de Lima Umeoka EH. A comprehensive overview on stress neurobiology: basic concepts and clinical implications. Front Behav Neurosci. 2018;12:127.
Ulrich-Lai YM, Herman JP. Neural regulation of endocrine and autonomic stress responses. Nat Rev Neurosci. 2009;10(6):397–409.
Guyenet PG, Stornetta RL, Bochorishvili G, Depuy SD, Burke PG, Abbott SB. C1 neurons: The body’s EMTs. Am J Physiol Regul Integr Comp Physiol. 2013;305(3):R187-204.
Krohn F, Novello M, van der Giessen RS, De Zeeuw CI, Pel JJM, Bosman LWJ. The integrated brain network that controls respiration. Elife. 2023;12:e83654.
Benarroch EE. Brainstem integration of arousal, sleep, cardiovascular, and respiratory control. Neurology. 2018;91(21):958–66.
Ruud J, Steculorum SM, Brüning JC. Neuronal control of peripheral insulin sensitivity and glucose metabolism. Nat Commun. 2017;8:15259.
Tracey KJ. Reflex control of immunity. Nat Rev Immunol. 2009;9(6):418–28.
Lowell BB. New neuroscience of homeostasis and drives for food, water, and salt. N Engl J Med. 2019;380(5):459–71.
van den Heuvel MP, Sporns O. Network hubs in the human brain. Trends Cogn Sci. 2013;17(12):683–96.
Loewy AD. Descending pathways to sympathetic and parasympathetic preganglionic neurons. J Auton Nerv Syst. 1981;3(2–4):265–75.
Ondicova K, Mravec B. Multilevel interactions between the sympathetic and parasympathetic nervous systems: a minireview. Endocr Regul. 2010;44(2):69–75.
Elfaki LA, Sharma B, Meusel LC, So I, Colella B, Wheeler AL, et al. Examining anterior prefrontal cortex resting-state functional connectivity patterns associated with depressive symptoms in chronic moderate-to-severe traumatic brain injury. Front Neurol. 2025;16:1541520.
Stern JE. Neuroendocrine-autonomic integration in the paraventricular nucleus: novel roles for dendritically released neuropeptides. J Neuroendocrinol. 2015;27(6):487–97.
Simmons S, Langlois LD, Oyola MG, Gouty S, Wu TJ, Nugent FS. Blast-induced mild traumatic brain injury alterations of corticotropin-releasing factor neuronal activity in the mouse hypothalamic paraventricular nucleus. Front Synaptic Neurosci. 2021;13:804898.
Watts DJ, Strogatz SH. Collective dynamics of “small-world” networks. Nature. 1998;393(6684):440–2.
Bassett DS, Bullmore E. Small-world brain networks. Neuroscientist. 2006;12(6):512–23.
Bassett DS, Bullmore ET. Small-world brain networks revisited. Neuroscientist. 2017;23(5):499–516.
Chen Y, Wang S, Hilgetag CC, Zhou C. Trade-off between multiple constraints enables simultaneous formation of modules and hubs in neural systems. PLoS Comput Biol. 2013;9(3):e1002937.
Bertolero MA, Thomas Yeo BT, D’Esposito M. The modular and integrative functional architecture of the human brain. Proc Natl Acad Sci U S A. 2015;112(49):E6798–807.
Seguin C, Sporns O, Zalesky A. Brain network communication: concepts, models and applications. Nat Rev Neurosci. 2023;24(9):557–74.
Bullmore E, Sporns O. The economy of brain network organization. Nat Rev Neurosci. 2012;13(5):336–49.
Chen Y, Wang S, Hilgetag CC, Zhou C. Features of spatial and functional segregation and integration of the primate connectome revealed by trade-off between wiring cost and efficiency. PLoS Comput Biol. 2017;13(9):e1005776.
Deco G, Tononi G, Boly M, Kringelbach ML. Rethinking segregation and integration: contributions of whole-brain modelling. Nat Rev Neurosci. 2015;16(7):430–9.
Lynn CW, Bassett DS. The physics of brain network structure, function and control. Nat Rev Phys. 2019;1(5):318–32.
van den Heuvel MP, Sporns O. A cross-disorder connectome landscape of brain dysconnectivity. Nat Rev Neurosci. 2019;20(7):435–46.
Lyon AR, Citro R, Schneider B, Morel O, Ghadri JR, Templin C, et al. Pathophysiology of takotsubo syndrome: JACC state-of-the-art review. J Am Coll Cardiol. 2021;77(7):902–21.
Ancona F, Bertoldi LF, Ruggieri F, Cerri M, Magnoni M, Beretta L, et al. Takotsubo cardiomyopathy and neurogenic stunned myocardium: similar albeit different. Eur Heart J. 2016;37(37):2830–2.
Tavazzi G, Zanierato M, Via G, Iotti GA, Procaccio F. Are neurogenic stress cardiomyopathy and takotsubo different syndromes with common pathways?: etiopathological insights on dysfunctional hearts. JACC Heart Fail. 2017;5(12):940–2.
Brame AL, Singer M. Stressing the obvious? An allostatic look at critical illness. Crit Care Med. 2010;38(Suppl 10):S600–7.
Cuesta JM, Singer M. The stress response and critical illness: a review. Crit Care Med. 2012;40(12):3283–9.
Fisher JP, Young CN, Fadel PJ. Central sympathetic overactivity: maladies and mechanisms. Auton Neurosci. 2009;148(1–2):5–15.
Schmidt JM, Crimmins M, Lantigua H, Fernandez A, Zammit C, Falo C, et al. Prolonged elevated heart rate is a risk factor for adverse cardiac events and poor outcome after subarachnoid hemorrhage. Neurocrit Care. 2014;20(3):390–8.
Rachfalska N, Putowski Z, Krzych ŁJ. Distant organ damage in acute brain injury. Brain Sci. 2020;10(12):1019.
Hasegawa Y, Uchikawa H, Kajiwara S, Morioka M. Central sympathetic nerve activation in subarachnoid hemorrhage. J Neurochem. 2022;160(1):34–50.
Baguley IJ, Heriseanu RE, Felmingham KL, Cameron ID. Dysautonomia and heart rate variability following severe traumatic brain injury. Brain Inj. 2006;20(4):437–44.
Prasad Hrishi A, Ruby Lionel K, Prathapadas U. Head rules over the heart: cardiac manifestations of cerebral disorders. Indian J Crit Care Med. 2019;23(7):329–35.
Stam CJ. Hub overload and failure as a final common pathway in neurological brain network disorders. Netw Neurosci. 2024;8(1):1–23.
Achard S, Delon-Martin C, Vértes PE, Renard F, Schenck M, Schneider F, et al. Hubs of brain functional networks are radically reorganized in comatose patients. Proc Natl Acad Sci U S A. 2012;109(50):20608–13.
Lv LQ, Hou LJ, Yu MK, Qi XQ, Chen HR, Chen JX, et al. Prognostic influence and magnetic resonance imaging findings in paroxysmal sympathetic hyperactivity after severe traumatic brain injury. J Neurotrauma. 2010;27(11):1945–50.
Podell JE, Moffet EW, Bodanapally UK, Pajoumand M, Silva LM, Hu P, et al. Magnetic resonance imaging lesions associated with paroxysmal sympathetic hyperactivity after traumatic brain injury. Neurotrauma Rep. 2024;5(1):317–29.
Brown HW, Plum F. The neurologic basis of cheyne-stokes respiration. Am J Med. 1961;30(6):849–60.
Mador MJ, Tobin MJ. Apneustic breathing. A characteristic feature of brainstem compression in achondroplasia? Chest. 1990;97(4):877–83.
Summ O, Hassanpour N, Mathys C, Groß M. Disordered breathing in severe cerebral illness – towards a conceptual framework. Respir Physiol Neurobiol. 2022;300:103869.
Dobson GP, Morris JL, Letson HL. Traumatic brain injury: symptoms to systems in the 21st century. Brain Res. 2024;1845:149271.
Robba C, Wahlster S, Newcombe V. Update on acute brain injury. Intensive Care Med. 2025;51(10):1924–6.
Hill CS, Coleman MP, Menon DK. Traumatic axonal injury: mechanisms and translational opportunities. Trends Neurosci. 2016;39(5):311–24.
Jarrahi A, Braun M, Ahluwalia M, Gupta RV, Wilson M, Munie S, et al. Revisiting traumatic brain injury: from molecular mechanisms to therapeutic interventions. Biomedicines. 2020;8(10):389.
Shi K, Tian DC, Li ZG, Ducruet AF, Lawton MT, Shi FD. Global brain inflammation in stroke. Lancet Neurol. 2019;18(11):1058–66.
Sabet N, Soltani Z, Khaksari M. Multipotential and systemic effects of traumatic brain injury. J Neuroimmunol. 2021;357:577619.
Sammons M, Popescu MC, Chi J, Liberles SD, Gogolla N, Rolls A. Brain-body physiology: local, reflex, and central communication. Cell. 2024;187(21):5877–90.
Busl KM, Bogossian EG, Claassen J, Helbok R, Provencio JJ, Robba C, et al. Beyond the bleed: complications after aneurysmal subarachnoid hemorrhage. Pathophysiology, clinical implications, and management strategies: a review. Crit Care. 2025;29(1):414.
Zygun DA, Doig CJ, Gupta AK, Whiting G, Nicholas C, Shepherd E, et al. Non-neurological organ dysfunction in neurocritical care. J Crit Care. 2003;18(4):238–44.
Zygun DA, Kortbeek JB, Fick GH, Laupland KB, Doig CJ. Non-neurologic organ dysfunction in severe traumatic brain injury. Crit Care Med. 2005;33(3):654–60.
Astarabadi M, Khurrum M, Asmar S, Bible L, Chehab M, Castanon L, et al. The impact of non-neurological organ dysfunction on outcomes in severe isolated traumatic brain injury. J Trauma Acute Care Surg. 2020;89(2):405–10.
Piek J, Chesnut RM, Marshall LF, van Berkum-Clark M, Klauber MR, Blunt BA, et al. Extracranial complications of severe head injury. J Neurosurg. 1992;77(6):901–7.
Mascia L, Sakr Y, Pasero D, Payen D, Reinhart K, Vincent JL. Extracranial complications in patients with acute brain injury: a post-hoc analysis of the SOAP study. Intensive Care Med. 2008;34(4):720–7.
Alberti A, Agnelli G, Caso V, Venti M, Acciarresi M, D’Amore C, et al. Non-neurological complications of acute stroke: frequency and influence on clinical outcome. Intern Emerg Med. 2011;6(Suppl 1):119–23.
Corral L, Javierre CF, Ventura JL, Marcos P, Herrero JI, Mañez R. Impact of non-neurological complications in severe traumatic brain injury outcome. Crit Care. 2012;16(2):R44.
Goyal K, Hazarika A, Khandelwal A, Sokhal N, Bindra A, Kumar N, et al. Non- neurological complications after traumatic brain injury: a prospective observational study. Indian J Crit Care Med. 2018;22(9):632–8.
Kumaria A, Kirkman MA, Scott RA, Dow GR, Leggate AJ, Macarthur DC, et al. A reappraisal of the pathophysiology of cushing ulcer: a narrative review. J Neurosurg Anesthesiol. 2024;36(3):211–7.
Šedý J, Kuneš J, Zicha J. Pathogenetic mechanisms of neurogenic pulmonary edema. J Neurotrauma. 2015;32(15):1135–45.
Tuzi S, Kranawetter B, Moerer O, Rohde V, Mielke D, Malinova V. Logistic organ dysfunction system as an early risk stratification tool after aneurysmal subarachnoid hemorrhage. Sci Rep. 2024;14(1):27639.
Brown EN, Lydic R, Schiff ND. General anesthesia, sleep, and coma. N Engl J Med. 2010;363(27):2638–50.
Hu Y, Wang Y, Zhang L, Luo M, Wang Y. Neural network mechanisms underlying general anesthesia: cortical and subcortical nuclei. Neurosci Bull. 2024;40(12):1995–2011.
Hawryluk GWJ, Aguilera S, Buki A, Bulger E, Citerio G, Cooper DJ, et al. A management algorithm for patients with intracranial pressure monitoring: the Seattle International Severe Traumatic Brain Injury Consensus Conference (SISBICC). Intensive Care Med. 2019;45(12):1783–94.
Varley TF, Sporns O, Puce A, Beggs J. Differential effects of propofol and ketamine on critical brain dynamics. PLoS Comput Biol. 2020;16(12):e1008418.
Varley TF, Denny V, Sporns O, Patania A. Topological analysis of differential effects of ketamine and propofol anaesthesia on brain dynamics. R Soc Open Sci. 2021;8(6):201971.
Grände PO. The “lund concept” for the treatment of severe head trauma–physiological principles and clinical application. Intensive Care Med. 2006;32(10):1475–84.
Réen L, Cederberg D, Radman A, Marklund N, Visse E, Siesjö P. Low morbidity and mortality in children with severe traumatic brain injury treated according to the lund concept: a population-based study. J Neurotrauma. 2023;40(7–8):720–9.
Khalili H, Ahl R, Paydar S, Sjolin G, Cao Y, Abdolrahimzadeh Fard H, et al. Beta-blocker therapy in severe traumatic brain injury: a prospective randomized controlled trial. World J Surg. 2020;44(6):1844–53.
Nordness MF, Maiga AW, Wilson LD, Koyama T, Rivera EL, Rakhit S, et al. Effect of propranolol and clonidine after severe traumatic brain injury: a pilot randomized clinical trial. Crit Care. 2023;27(1):228.
Alshaya AI, Aldhaeefi M, Alodhaiyan N, Alqahtani M, Althewaibi S, Alshahrani W, et al. Clonidine safety and effectiveness in the management of suspected paroxysmal sympathetic hyperactivity post-traumatic brain injury: A retrospective cohort study. Sci Prog. 2023;106(4):368504231201298.
Mansour MS, Seidy NSE, Fathey YI. Evaluation of beta-blocker effects on patients with traumatic brain injury: interventional double-blinded randomized controlled trial. Ain Shams J Anesthesiol. 2023;15(1):65.
Hart S, Lannon M, Chen A, Martyniuk A, Sharma S, Engels PT. Beta blockers in traumatic brain injury: a systematic review and meta-analysis. Trauma Surg Acute Care Open. 2023;8(1):e001051.
Borgmann D, Rigoux L, Kuzmanovic B, Edwin Thanarajah S, Münte TF, Fenselau H, et al. Technical note: modulation of fMRI brainstem responses by transcutaneous vagus nerve stimulation. Neuroimage. 2021;244:118566.
Lee MC, Bartuska A, Chen J, Kim RK, Jaradeh S, Mihm F. Stellate ganglion block catheter for paroxysmal sympathetic hyperactivity: calming the “neuro-storm.” Reg Anesth Pain Med. 2023;48(10):522–5.
Sharp DJ, Scott G, Leech R. Network dysfunction after traumatic brain injury. Nat Rev Neurol. 2014;10(3):156–66.
Petrella JR. Use of graph theory to evaluate brain networks: a clinical tool for a small world? Radiology. 2011;259(2):317–20.
Filippi M, van den Heuvel MP, Fornito A, He Y, Hulshoff Pol HE, Agosta F, et al. Assessment of system dysfunction in the brain through MRI-based connectomics. Lancet Neurol. 2013;12(12):1189–99.
Pandit AS, Expert P, Lambiotte R, Bonnelle V, Leech R, Turkheimer FE, et al. Traumatic brain injury impairs small-world topology. Neurology. 2013;80(20):1826–33.
Swanson LW, Hahn JD, Sporns O. Neural network architecture of a mammalian brain. Proc Natl Acad Sci U S A. 2024;121(39):e2413422121.
Swanson LW, Hahn JD, Sporns O. The intrinsic neuronal network of the central nervous system and its modular (subsystem) architecture in a mammal. Proc Natl Acad Sci U S A. 2025;122(40):e2519768122.
Fukushima M, Betzel RF, He Y, van den Heuvel MP, Zuo XN, Sporns O. Structure-function relationships during segregated and integrated network states of human brain functional connectivity. Brain Struct Funct. 2018;223(3):1091–106.
Thayer JF, Lane RD. Claude Bernard and the heart-brain connection: further elaboration of a model of neurovisceral integration. Neurosci Biobehav Rev. 2009;33(2):81–8.
De Raedt S, De Vos A, De Keyser J. Autonomic dysfunction in acute ischemic stroke: an underexplored therapeutic area? J Neurol Sci. 2015;348(1–2):24–34.