Cho GJ, Kim J, Kim JY, Han SW, Lee SB, Oh M-J, et al. Adverse pregnancy outcomes and maternal chronic diseases in the future: a cross-sectional study using KoGES-HEXA data. J Clin Med. 2022;11(5):1457.
World Health Organization. Maternal health [Internet]. Who.int. World Health Organization; 2019 [cited 2024 Sep 16]. Available from: https://www.who.int/health-topics/maternal-health#tab=tab_1
Centers for Disease Control and Prevention. Percentage of mothers with gestational diabetes, by maternal age—National vital statistics System, united States, 2016 and 2021. Morbidity Mortal Wkly Rep. 2023;71(1):16.
Garovic VD, White WM, Vaughan L, Saiki M, Parashuram S, Garcia-Valencia O, Weissgerber TL, Milic N, Weaver A, Mielke MM. Incidence and long-term outcomes of hypertensive disorders of pregnancy. J Am Coll Cardiol. 2020;75(18):2323–34.
World Health Organization. Anaemia [Internet]. www.who.int 2023 [cited 2024 Sep 16]. Available from: https://www.who.int/news-room/fact-sheets/detail/anaemia#:~:text=Globally%2C%20it%20is%20estimated%20tha
Mestman JH. Hyperthyroidism in pregnancy. Best Pract Res Clin Endocrinol Metab. 2004;18(2):267–88.
Wang W, Teng W, Shan Z, Wang S, Li J, Zhu L, et al. The prevalence of thyroid disorders during early pregnancy in China: the benefits of universal screening in the first trimester of pregnancy. Eur J Endocrinol. 2011;164(2):263–8.
Mumtaz H, Danish R, Yousaf T, Sehgal S, Jawad A, Haider SM. Frequency and outcome of pregnant females presenting with thrombocytopenia at a tertiary care hospital. Cureus. 2023;15(11).
Sindiani A, Awadallah E, Alshdaifat E, Melhem S, Kheirallah K. The relationship between maternal health and neonatal low birth weight in Amman, Jordan: a case-control study. J Med Life. 2023;16(2):290.
Benton M, Bird J, Pawlby S, Ismail K. The impact of gestational diabetes mellitus on perceived mother-infant bonding: a qualitative study. J Reproductive Infant Psychol 2023 Jul 28:1–4.
World Health Organisation. Preterm birth [Internet]. www.who.int.
. 2023 [cited 2024 Sep 16]. Available from: https://www.who.int/news-room/fact-sheets/detail/preterm-birth#:~:text=Preterm%20is%20defined%20as%20babies
Teune MJ, Bakhuizen S, Gyamfi Bannerman C, Opmeer BC, van Kaam AH, van Wassenaer AG, et al. A systematic review of severe morbidity in infants born late preterm. Am J Obstet Gynecol. 2011;205(4):e3741–9.
Saigal S, Doyle LW. An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet. 2008;371(9608):261–9.
Chawanpaiboon S, Vogel JP, Moller AB, Lumbiganon P, Petzold M, Hogan D, et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob Health. 2019;7(1):e37-46.
Pierrat V, Marchand-Martin L, Marret S, Arnaud C, Benhammou V, Cambonie G, Debillon T, Dufourg MN, Gire C, Goffinet F, Kaminski M. Neurodevelopmental outcomes at age 5 among children born preterm: EPIPAGE-2 cohort study. BMJ. 2021;373.
Sarda SP, Sarri G, Siffel C. Global prevalence of long-term neurodevelopmental impairment following extremely preterm birth: a systematic literature review. J Int Med Res. 2021;49(7):03000605211028026.
Meis PJ, Goldenberg RL, Mercer BM, Iams JD, Moawad AH, Miodovnik M, Menard MK, Caritis SN, Thurnau GR, Bottoms SF, Das A. The preterm prediction study: risk factors for indicated preterm births. Am J Obstet Gynecol. 1998;178(3):562–7.
Behrman RE, Butler Adrienne Stith, Institute Of Medicine (U.S.). Committee on Understanding premature birth and assuring healthy Outcomes. Preterm birth: causes, consequences, and prevention. Washington, D.C.: National Academies; 2007.
Reiss JD, Peterson LS, Nesamoney SN, Chang AL, Pasca AM, Marić I, et al. Perinatal infection, inflammation, preterm birth, and brain injury: a review with proposals for future investigations. Exp Neurol. 2022;351:113988.
Romero R, Espinoza J, Gonçalves LF, Kusanovic JP, Friel L, Hassan S. The role of inflammation and infection in preterm birth. Semin Reprod Med. 2007;25(1):21–39.
Chappell LC, Brocklehurst P, Green ME, Hunter R, Hardy P, Juszczak E, et al. Planned early delivery or expectant management for late preterm pre-eclampsia (PHOENIX): a randomised controlled trial. Lancet. 2019;394(10204):1181–90.
Maxey AP, Wheeler SJ, Travis JM, McCain ML. Contractile responses of engineered human µmyometrium to prostaglandins and inflammatory cytokines. APL Bioeng. 2024;8(4):046115.
Crump C. An overview of adult health outcomes after preterm birth. Early Hum Dev. 2020;150:105187.
Strand KM, Heimstad R, Iversen AC, Austgulen R, Lydersen S, Andersen GL, et al. Mediators of the association between pre-eclampsia and cerebral palsy: population based cohort study. BMJ. 2013;347:f4089.
Zen M, Schneuer F, Alahakoon TI, Nassar N, Lee VW. Perinatal and child factors mediate the association between preeclampsia and offspring school performance. J Pediatr. 2021;238:153–e1604.
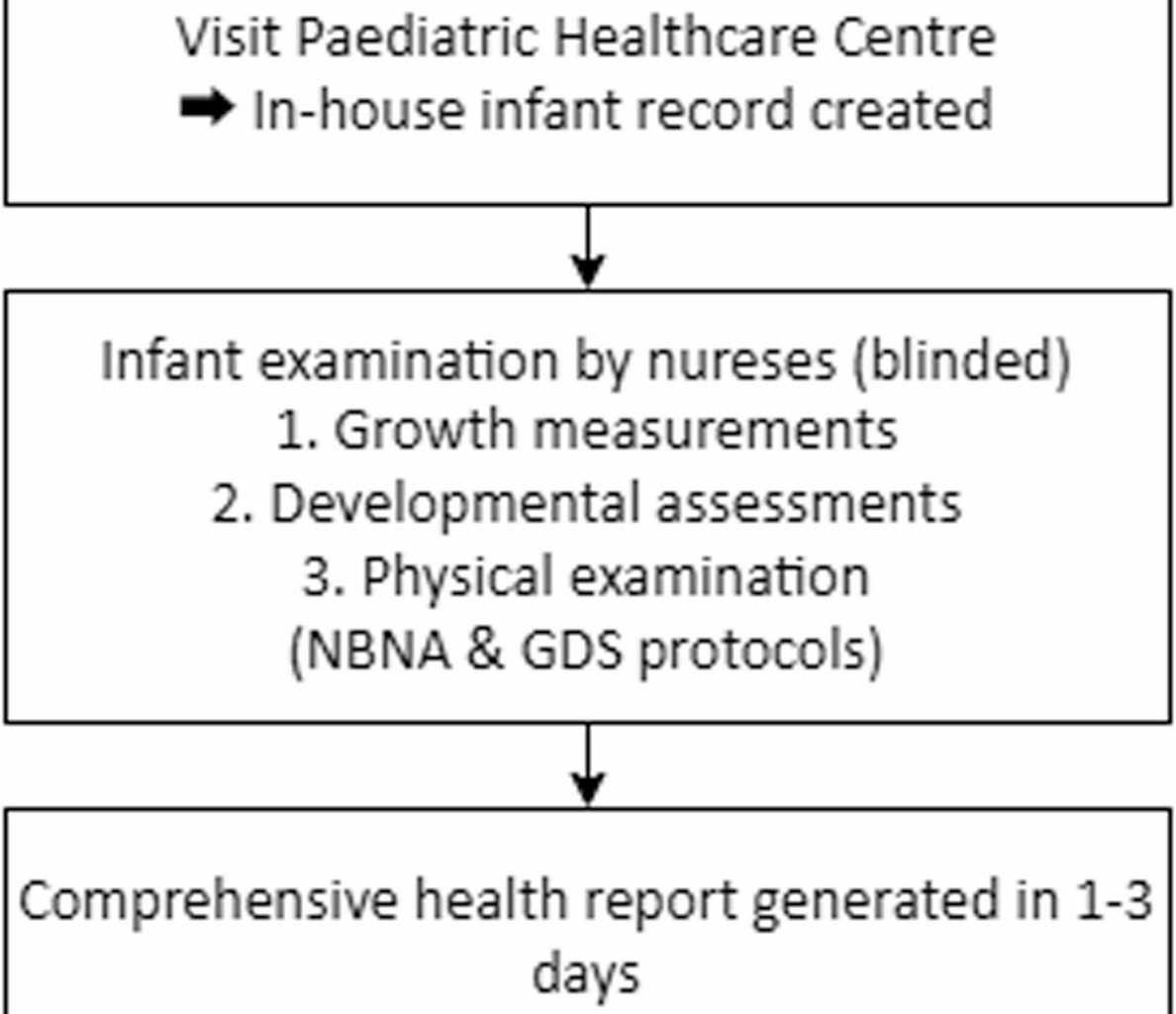
Bao X, Liu W. Application of neonatal behavioral neurological assessment and observation to the assessment of brain development and early intervention in preterm and young infants. Chin J Pract Pediatr. 2017;32:820–2.
Yang J, Hu L, Zhang Y, Shi Y, Jiang W, Song C. Gesell developmental schedules scores and the relevant factors in children with Down syndrome. J Pediatr Endocrinol Metab. 2020;33(4):539–46.
American Psychological Association. Age. APA Dictionary of Psychology. 2023 Nov 15. Available from: https://dictionary.apa.org/age
American Psychological Association. Gestational age. APA Dictionary of Psychology. 2018 Apr 19. Available from: https://dictionary.apa.org/gestational-age
Evelyn AH, Christian SG, Thorsten F, Monya Todesco B, Martina K, Mirjam K, et al. Sensitivity, specificity, and diagnostic accuracy of WHO 2013 criteria for diagnosis of gestational diabetes mellitus in low risk early pregnancies: international, prospective, multicentre cohort study. BMJ Med. 2023;2(1):e000330.
Khedagi AM, Bello NA. Hypertensive disorders of pregnancy. Cardiol Clin. 2021;39(1):77–90.
Soldin OP. Thyroid function testing in pregnancy and thyroid disease: trimester-specific reference intervals. Ther Drug Monit. 2006;28(1):8–11.
Pavord S, Daru J, Prasannan N, Robinson S, Stanworth S, Girling J, et al. UK guidelines on the management of iron deficiency in pregnancy. Br J Haematol. 2020;188(6):819–30.
Nandy A, Guha A, Datta D, Mondal R. Evolution of clinical method for new-born infant maturity assessment. J Maternal-Fetal Neonatal Med. 2020;33(16):2852–9.
Zhou BF, Cooperative Meta-Analysis Group of the Working Group on Obesity in China. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults–study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci BES. 2002;15(1):83–96.
Kong L, Nilsson IAK, Gissler M, Lavebratt C. Associations of maternal diabetes and body mass index with offspring birth weight and prematurity. JAMA Pediatr. 2019;173(4):371.
Chen S, Wang X, Lee BK, Gardner RM. Associations between maternal metabolic conditions and neurodevelopmental conditions in offspring: the mediating effects of obstetric and neonatal complications. BMC Med. 2023;21(1):422.
Qi Y, Lin Z, Lu H, Zhao P, Hou Y, Mao J. The association between pregnancy-induced hypertension and neonatal cerebral metabolism, hemodynamics, and brain injury as determined by physiological imaging. Front Physiol. 2022;13:756386.
Drommelschmidt K, Mayrhofer T, Hüning B, Stein A, Foldyna B, Schweiger B, et al. Incidence of brain injuries in a large cohort of very preterm and extremely preterm infants at term-equivalent age: results of a single tertiary neonatal care center over 10 years. Eur Radiol. 2024;34(8):5239–49.
Molloy EJ, El-Dib M, Soul J, Juul S, Gunn AJ, Bender M, et al. Neuroprotective therapies in the NICU in preterm infants: present and future (Neonatal neurocritical care Series). Pediatr Res. 2024;95(5):1224–36.
Brown HK, Speechley KN, Macnab J, Natale R, Campbell MK. Neonatal morbidity associated with late preterm and early term birth: the roles of gestational age and biological determinants of preterm birth. Int J Epidemiol. 2014;43(3):802–14.
Malhotra A, Allison BJ, Castillo-Melendez M, Jenkin G, Polglase GR, Miller SL. Neonatal morbidities of fetal growth restriction: pathophysiology and impact. Front Endocrinol (Lausanne). 2019;10:55.
Burton GJ, Jauniaux E. Pathophysiology of placental-derived fetal growth restriction. Am J Obstet Gynecol. 2018;218(2S):S745–61.
Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–82. https://doi.org/10.1037/0022-3514.51.6.1173.
Hee Chung E, Chou J, Brown KA. Neurodevelopmental outcomes of preterm infants: a recent literature review. Transl Pediatr. 2020;9(Suppl 1):S3–8.
Hufnagel A, Dearden L, Fernandez-Twinn DS, Ozanne SE. Programming of cardiometabolic health: the role of maternal and fetal hyperinsulinaemia. J Endocrinol. 2022;253(2):R47–63. https://doi.org/10.1530/JOE-21-0332.
Hu XQ, Zhang L. Hypoxia and mitochondrial dysfunction in pregnancy complications. Antioxidants. 2021;10(3):405.
Counsell SJ, Maalouf EF, Fletcher AM, Duggan P, Battin M, Lewis HJ, et al. MR imaging assessment of myelination in the very preterm brain. AJNR Am J Neuroradiol. 2002;23(5):872–81.
González-Rojas A, Valencia-Narbona M. Neurodevelopmental disruptions in children of preeclamptic mothers: pathophysiological mechanisms and consequences. Int J Mol Sci. 2024;25(7):3632.
Growth Standard for Children Under 7 Years of Age. Biomed Environ Sci. 2023;36(7):663–4.
Sharma A, Davis A, Shekhawat PS. Hypoglycemia in the preterm neonate: etiopathogenesis, diagnosis, management and long-term outcomes. Transl Pediatr. 2017;6(4):335–48. https://doi.org/10.21037/tp.2017.10.06.