This systematic review and meta-analysis synthesized evidence from randomized controlled trials comparing short-duration (< 8 h/day) and long-duration (≥ 8 h/day) KMC with conventional care in LBW infants. Across all pooled analyses, KMC significantly improved neonatal growth outcomes and exclusive breastfeeding rates, regardless of daily duration. Daily weight gain increased by an average of 4.52 g/day overall, with both short-duration (3.71 g/day) and long-duration (5.04 g/day) KMC showing benefit compared to control. Weekly length gain improved similarly in both subgroups (0.09 cm/week), while weekly head circumference gain was greater in the short-duration group (0.07 cm/week) than in the long-duration group (0.04 cm/week). Exclusive breastfeeding rates increased by 2.09-fold overall, with a stronger association in short-duration KMC (OR 2.42) than in long-duration KMC (OR 1.81). These results suggest that meaningful growth and feeding improvements can be achieved with as little as several hours of daily KMC.
The core mechanisms underlying these benefits remain consistent with prior literature—thermoregulation, reduced energy expenditure, and enhanced maternal-infant bonding redirect metabolic resources toward growth [8]. Shorter, repeated KMC sessions may minimize fatigue and optimize feeding frequency, which could explain why short-duration KMC performed comparably or better in some outcomes despite lower daily exposure. This hypothesis is supported by Mazumder et al., whose community-based randomized trial showed that intermittent KMC (≥ 8 h/day) significantly reduces infant mortality and improves growth outcomes [11]. The association between head circumference growth and continuous KMC may reflect long-term neurodevelopmental benefits. Prolonged skin-to-skin contact and maternal interaction in continuous KMC could stimulate vagal nerve activity and growth hormone secretion, influencing cranial development. Similarly, Zhang et al. [24] reported that head circumference growth in preterm infants correlates with neurodevelopmental outcomes, and sustained care interventions optimize brain volume development. However, the robustness of this finding is limited by the small number of studies on continuous KMC (n = 1).
The enhancement of exclusive breastfeeding rates is another notable advantage of KMC. Joshi et al. [7] proposed that KMC strengthens maternal-infant bonding and tactile stimulation, directly promoting prolactin and oxytocin release to increase milk production.
Our reclassification of KMC into short (< 8 h/day) and long (≥ 8 h/day) daily durations addresses a major methodological gap in prior reviews that compared “intermittent” and “continuous” KMC. These earlier definitions were inconsistent, with some “intermittent” protocols lasting over 12 h/day, overlapping with what other studies termed “continuous.” By adopting a reproducible, time-based cut-off, we reduced misclassification bias and included trials with ambiguous terminology, thereby providing a more objective framework for comparison and clinical recommendations. Beyond daily duration, the timing of KMC initiation may also influence outcomes. For example, Arya et al.’s multicenter trial [9] demonstrated that immediate initiation after birth significantly improved exclusive breastfeeding rates (78% vs. 52% with conventional care). Thus, our classification not only clarifies previous inconsistencies but also complements existing reviews by offering a practical, standardized approach to evaluating KMC effectiveness.
In resource-limited settings, KMC is a low-cost, scalable intervention with substantial public health value. This study found that even intermittent KMC (a few hours daily) significantly improves growth outcomes, offering a feasible solution for families unable to provide 24-hour continuous care. For instance, in sub-Saharan Africa, Mazumder et al.’s [11] community trial demonstrated that training community health workers to promote KMC increased 6-month survival rates of LBW infants to 89% (vs. 76% in controls). Moreover, KMC’s breastfeeding benefits reduce reliance on formula, mitigating infection and malnutrition risks—particularly crucial in under-resourced regions [25]. However, mode selection should be context-specific: intermittent KMC may suit hospital settings or high-risk infants, whereas continuous KMC could be more effective in community or home-based care. Studies suggest that ≥ 6 h/day of maternal KMC achieves outcomes comparable to hospital-based continuous care, with higher family engagement [26]. Mode selection for KMC should be context-specific, taking into account factors such as the setting (hospital vs. community/home-based), the health status of the infant, and available resources [27]. In hospital settings, where neonates may be at higher risk or require more intensive monitoring, intermittent KMC (e.g., 3–4 h a day) can offer a balance between the benefits of skin-to-skin contact and medical interventions [28]. This form of care might also be more practical in settings where resources such as trained personnel or space are limited [29]. On the other hand, continuous KMC is often more beneficial for term or stable low-birth-weight infants, particularly in community-based or home settings, where caregivers can provide extended skin-to-skin contact without the constraints of hospital infrastructure [30].
Studies consistently suggest that ≥ 6 h of daily maternal KMC can achieve outcomes comparable to those seen in hospital-based continuous KMC [31, 32]. Importantly, this level of care not only improves neonatal outcomes such as weight gain, temperature regulation, and reduced mortality, but also fosters a higher level of family engagement [33]. This engagement is crucial, as it empowers mothers and other caregivers, encourages bonding, and facilitates the development of a nurturing caregiving environment, all of which play a key role in the infant’s emotional and physiological development [34]. The flexibility of KMC models allows it to be adapted to various contexts, thereby ensuring that more families can benefit from this life-saving intervention [35]. Yet, Sivanandan et al.’s meta-analysis indicated that ≥ 8 h/day is required for significant mortality reduction [13]. Thus, future clinical guidelines should refine KMC protocols, tailoring recommendations to resource availability and family circumstances.
The enhancement in exclusive breastfeeding rates aligns with established evidence that skin-to-skin contact stimulates oxytocin and prolactin release, increasing milk production and facilitating early initiation [13, 34]. Our finding that short-duration KMC achieved a higher odds ratio for breastfeeding success may be related to its flexibility, allowing mothers to integrate KMC into daily routines more sustainably. In contrast, long-duration KMC, while beneficial, may be harder to maintain in hospital or working contexts.
From a public health perspective, the observation that both short and long KMC durations improve growth and feeding outcomes is critical for resource-limited settings. Even partial daily implementation may be sufficient to achieve clinically relevant benefits where continuous care is impractical. Evidence from community trials shows that integrating KMC promotion into maternal and child health programs can substantially improve survival, feeding, and growth outcomes without heavy infrastructure investment [11]. However, heterogeneity across studies was substantial. This variability likely stems from differences in baseline infant health, gestational age, maternal nutritional status, KMC initiation timing, and hospital vs. community settings. Such heterogeneity may also have contributed to the asymmetry observed in some funnel plots, alongside potential small-study effects. Although Egger’s test did not indicate statistically significant publication bias, the limited number of studies per outcome reduces confidence in this finding.
Strengths and limitations
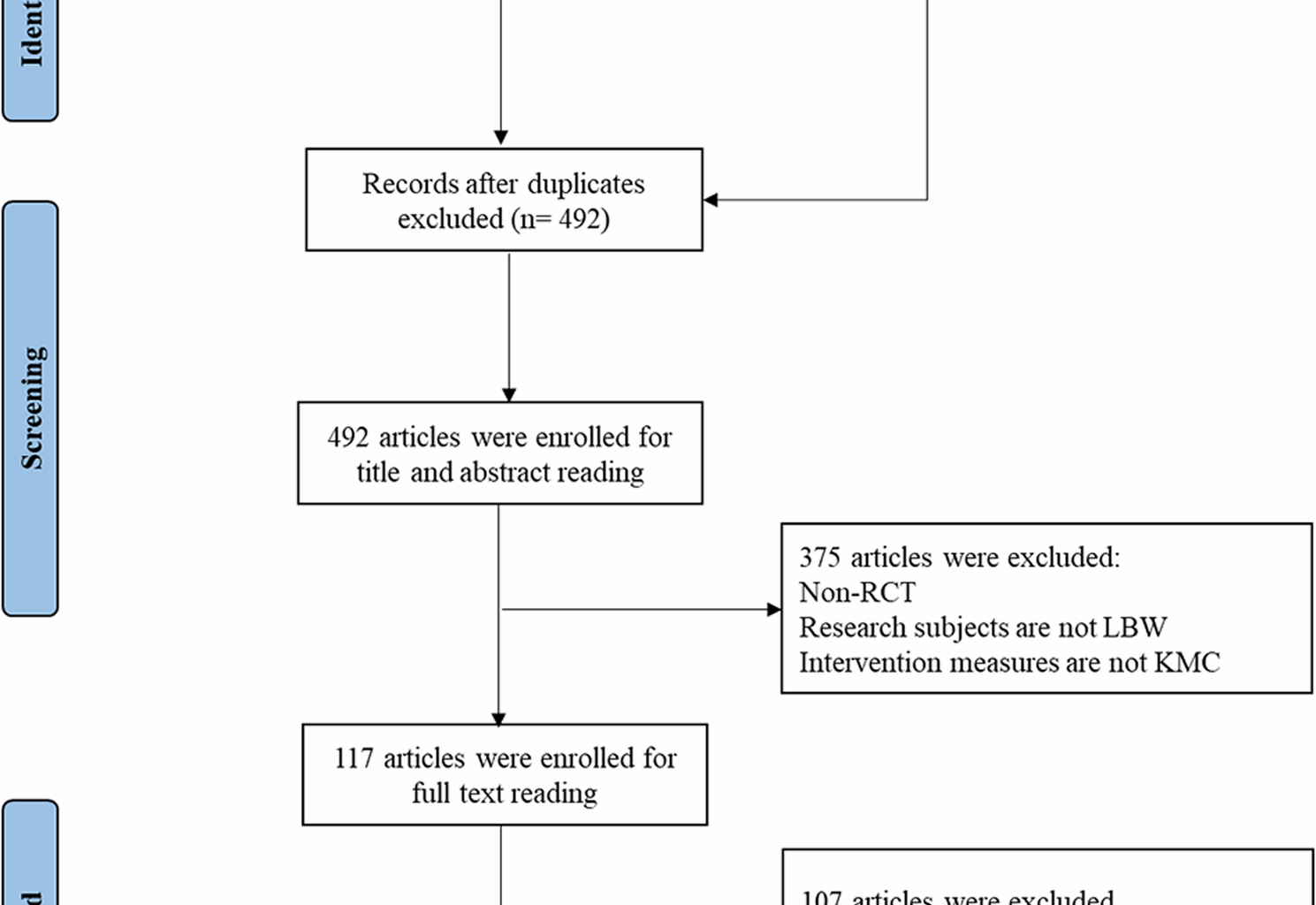
A key strength of this review is the standardized time-based classification of KMC duration, enabling a clearer evaluation of dose-response effects. The inclusion of exclusively randomized trials strengthens causal inference. Limitations include possible residual confounding from unmeasured factors such as feeding supplementation, lack of data on adherence, and the relatively small number of trials in each subgroup, particularly for long-duration KMC in some outcomes.
Implications for practice and research
Given that both short- and long-duration KMC confer measurable benefits, clinical guidelines should emphasize feasibility and sustainability rather than adherence to rigid daily hour thresholds. Future trials should adopt standardized KMC duration reporting and explore threshold effects for specific outcomes. Additionally, more granular measurement of feeding practices and neurodevelopmental outcomes would help clarify whether certain durations preferentially benefit different domains of infant health.