QFD-based investigation and analysis of elderly care needs
Prior to developing the multifunctional care wheelchair, the research team conducted a systematic needs assessment targeting both caregivers and elderly individuals with disabilities. By integrating semi-structured interviews, standardized questionnaires, and field observations, two predominant challenges were identified: biomechanically demanding operations (e.g., patient transfers and posture adjustments) and insufficient functional support, particularly in privacy-sensitive activities such as toileting and bathing. Concurrently, the study systematically evaluated improvement potentials in safety mechanisms (equipment stability and misuse prevention) and comfort features (pressure distribution and ergonomic adaptability) of existing assistive devices, thereby establishing a robust empirical foundation for subsequent engineering design.
Semi-structured interviews were conducted focusing on three dimensions: biomechanical loads during physical caregiving tasks (e.g., lifting and assisted standing), functional limitations of current devices in daily activity support (e.g., toileting and bathing), and specific user requirements for safety features (e.g., anti-tip mechanisms) and comfort enhancements (e.g., pressure-relieving seat cushions). A total of 48 participants were involved in the needs assessment phase, including 36 professional caregivers and 12 elderly individuals with moderate-to-severe physical disabilities who were regular wheelchair users.
Participants were recruited from three long-term care facilities in Shanghai. Caregivers had an average of 6.8 years of caregiving experience (range: 2–17 years), and their age ranged from 25 to 59 years old. The elderly participants were aged 68–88, most of whom required daily assistance with toileting and posture transitions. A majority of the elderly participants reported requiring daily assistance with activities such as toileting and posture adjustment, which was later confirmed as a high-frequency, high-burden category in the quantitative task analysis.
In parallel, a structured questionnaire was designed to systematically collect caregivers’ demographic data (e.g., age, caregiving tenure) and task load parameters (e.g., task types, execution frequency, and per-session duration), as summarized in Table 1. Post-task physiological fatigue was assessed via Visual Analog Scales (VAS), supplemented by open-ended questions to prioritize device improvement needs and solicit specific optimization suggestions. The questionnaire emphasized task-load correlation analysis to establish a data-driven foundation for subsequent functional prioritization. The questionnaire was distributed to the same 36 caregivers, and 33 valid responses were collected (response rate: 95.8%). The sample covered a broad age and experience spectrum, providing a representative cross-section of the professional care population in institutional settings.
Table 1 Care needs assessment questionnaire content
Based on the structured questionnaire described in Table 1, the collected data were quantified and summarized in Table 2. In this survey, three key parameters were assessed for each caregiving task: (i) Handling duration, defined as the average time required to complete a single activity, which is critical for evaluating caregiver workload and elderly user safety; (ii) Execution frequency, or how often the task is performed daily; and (iii) Caregiver fatigue level, rated on a five-point scale. Through systematic analysis, the operational characteristics were categorized into four major domains: daily living assistance, basic care, health management, and psychological support. For example, within the daily living assistance category, toileting support requires frequent interventions (five times per day) and induces moderate-to-high caregiver fatigue (rated 3/5), highlighting its high operational frequency and significant physical burden.
Table 2 Care demand operational metrics
Building upon quantified needs assessment results, this study employs Quality Function Deployment (QFD) methodology to construct a House of Quality (HOQ) model, systematically establishing traceability between clinical requirements and technical parameters. A multi-criteria decision analysis framework was developed to create requirement-characteristic correlation matrices, enabling quantitative evaluation of engineering parameters’ contributions to user needs. Within the HOQ model, calculation of requirement-feature relationship intensity integrates multidimensional factors including demand priority, technical feasibility, and cost constraints, for which we designed an Analytic Hierarchy Process (AHP)-based weighting algorithm.
$$\:\text{Weighted\:Relation\:}\text{Score}=\text{Effective\:Score}\cdot\:\text{Importance\:Weight}\cdot\:\text{Resource\:Weigh}{\text{t}}^{\text{-1}}$$
(1)
Within the established evaluation framework, the Effective Score (\(\:{E}_{i}\)) quantifies the fulfillment degree of design response \(\:i\:\)towards specific requirement \(\:j\), normalized to a 0–1 scale. The Importance Weight (\(\:{I}_{i}\)), derived through Analytic Hierarchy Process, reflects priority rankings among care requirements. The Resource Weight (\(\:{R}_{i}\)) measures material and human resource consumption, with its reciprocal form embodying the negative regulatory effect of resource constraints. The comprehensive priority score for each design response is calculated via the weighted summation formula:
$$\:\text{Total\:Score\:for\:Design\:}\text{Respons}{\text{e}}_{i}={\sum\:}_{j=1}^{n}({E}_{i}\times\:{I}_{i}\times\:{R}_{i}^{-1})$$
(2)
Where the summation spans all n associated care requirements. Higher scores indicate greater implementation priority when balancing requirement fulfillment and resource efficiency.
Within the House of Quality (HOQ) matrix, we systematically established a demand-response mapping framework. Taking user requirements (VOC) such as “toileting assistance” as inputs and corresponding technical descriptors (HOWs) like “bathroom aid mechanisms” as outputs, the relationship matrix employs a chromatic coding system to visualize interaction intensities (e.g., dark hues for strong correlations, light hues for weak) complemented by numerical annotations. This methodology enables identification of mission-critical technical parameters through structured decision-making processes, achieving Pareto-optimal resource allocation and iterative design refinement. The HOQ matrix visualization is presented in Fig. 1.
House of Quality (HOQ) Requirement Conversion Matrix
This prioritization framework enables precise alignment between core user needs and engineering parameters, strategically directing resources toward high-impact design improvements. Serving as the decision-making nucleus, the HOQ model prevents redundant investments in non-essential functions through its requirement-feature mapping mechanism, ensuring concentrated resource allocation towards critical-to-quality characteristics. The systematic methodology not only achieves iterative functional enhancement but also establishes a data-driven translation pipeline that converts user needs into quantifiable engineering specifications, thereby significantly improving market adaptability and clinical implementation success rates.
QFD-driven multimodal care wheelchair design
Derived from elderly individuals living with disability, this study proposes a cost-effective, user-friendly, and scenario-adaptive wheelchair design framework. Critical design requirements encompass:
1.
Intelligent posture transition mechanisms for seamless bed-wheelchair transfer through multi-DOF adjustment systems;
2.
Integrated standing-assist modules to facilitate lower limb rehabilitation while mitigating pressure ulcer risks and enhancing psychological well-being;
3.
Omnidirectional mobility chassis for enhanced maneuverability in confined spaces (e.g., bathrooms), reducing positional calibration needs during toileting/bathing;
4.
Innovative toilet-assist mechanisms enabling in-situ defecation functions to alleviate caregiver burden;
5.
Bathroom docking systems ensuring safe bathing posture maintenance.
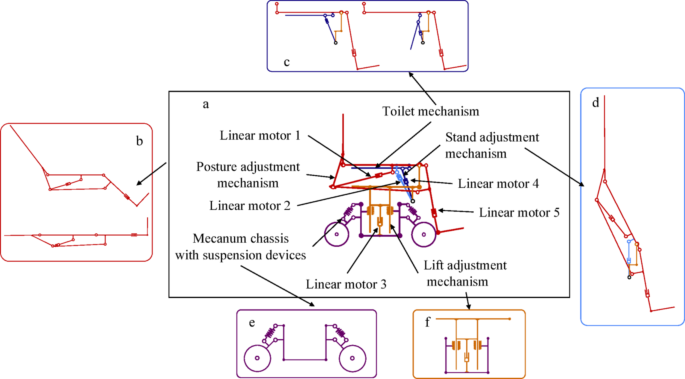
The finalized design integrates five core subsystems: smart posture transition system, toilet-assist mechanism, standing rehabilitation module, omnidirectional drive chassis, and height adjustment unit, with system architecture illustrated in Fig. 2.
Linkage Model of the Multifunctional Integrated Care Wheelchair, (a) Design solution of multifunctional integrated wheelchair, (b) Multi-posture transition mechanism, (c) Toileting assistance mechanism, (d) Standing assistance mechanism, f. Lifting adjustment mechanism, (e) Mecanum wheel mobile chassis
Structure Design
This subsection presents the 3D parametric modeling of the integrated wheelchair system, with comprehensive architecture shown in Fig. 3. Core functional modules include: a posture coordination mechanism enabling sitting-lying transitions, The lifting mechanism adapting to varied care scenarios, the toileting assistance device supporting in-situ defecation, and omnidirectional mobility chassis enhancing environmental adaptability. An integrated navigation system was specifically developed to enhance autonomous mobility through real-time environmental perception and path-planning algorithms. Subsequent sections provide systematic elucidation of each subsystem’s mechanical configuration and synergistic operation principles.
CAD Model of Multifunctional Integrated Care Wheelchair
Posture transition mechanism
The posture adjustment system adopts a three-linkage architecture (Fig. 4), where Link 1 (backrest), Link 2 (seat), and Link 3 (leg rest) achieve coordinated motion via an optimized four-bar linkage mechanism. To improve drive efficiency, a synchronized dual-degree-of-freedom control is implemented using a single linear actuator that simultaneously drives the backrest and leg rest. To meet ergonomic requirements, a telescopic compensation mechanism is integrated into the leg rest, which automatically adjusts the shank support length during sit-to-stand transitions to accommodate biomechanical variations caused by the shifting of joint centers. This not only ensures smooth limb support but also contributes to maintaining the user’s balance by stabilizing the center of gravity (CoG) throughout the posture transition [24].
Importantly, the full recline posture also enables horizontal transfers, allowing users to move safely and comfortably between the wheelchair and a bed or other surfaces [25, 26]. To enhance comfort and prevent limb strain during such transfers, the leg rest compensation mechanism dynamically adapts to changes in leg length that occur due to the relative motion of the knee joint during recline. The kinematic diagram (Fig. 4) illustrates the sit-to-recline transition, where the linear actuator adjusts the backrest inclination (θ₁) from 96° to 180° and the leg rest elevation (θ₂) from 90° to 180°, achieving a seamless and fully extended 180° semi-reclined posture suitable for resting or transfer scenarios.
Sit-to-Lie Postural Transition Mechanism
Standing assistance mechanism
Based on posture transition capabilities, dual linear actuators (L1/L2) are integrated to provide safe, progressive standing assistance. As shown in the motion sequence (Fig. 5), a phased center-of-gravity control strategy is adopted: Initially, actuator L1 increases the backrest inclination from 95° to 101°, transitioning users to a semi-reclined position (hip angle Φ₁=105°) with a 120 mm posterior shift of the center of gravity to prevent forward tipping. Subsequently, synchronized activation of L1 and L2 elevates the backrest-seat assembly (angular velocity ω = 2°/s), resulting in a 260 ± 10 mm vertical center-of-gravity lift to achieve a full standing posture (knee angle Φ₂ = 155°).
Sit-to-Stand Postural Conversion Mechanism
Toileting assistance device
Needs assessment indicated a high dependency on toileting assistance among moderately to severely elderly individuals living with disability, with significant fall risks during postural transitions. To mitigate transfer risks, a downward-flipping central seat panel is incorporated. As shown in Fig. 3, actuator L3 rotates the central seat panel downward while simultaneously elevating the waste diversion device to align with the toilet. Users can complete toileting without transfer when the wheelchair is positioned above the toilet. The system directs waste into the toilet, effectively preventing environmental contamination.
Omnidirectional chassis and detachable backrest
To enhance maneuverability in confined indoor environments, the chassis adopts four Mecanum wheels (Fig. 3), enabling forward/backward movement, lateral translation, and in-place rotation. This omnidirectional system enables flexible navigation through narrow corridors and tight turning spaces, significantly improving operational convenience.
For bathing scenarios, a detachable backrest system was developed (Fig. 3). By rotating the armrest, the locking mechanism is disengaged, allowing quick removal of the intelligent navigation-integrated backrest. The perforated support backrest improves cleaning efficiency, enabling direct bathing on the wheelchair and minimizing transfer-associated fall risks.