Swedo SE, Leckman JF, Rose NR. From research subgroup to clinical syndrome: modifying the PANDAS criteria to describe PANS (pediatric acute-onset neuropsychiatric syndrome). Pediatr Therapeut. 2012;2(2):113.
Frankovich J, Thienemann M, Pearlstein J, Crable A, Brown K, Chang K. Multidisciplinary clinic dedicated to treating youth with pediatric acute-onset neuropsychiatric syndrome: presenting characteristics of the first 47 consecutive patients. J Child Adolesc Psychopharmacol. 2015;25(1):38–47.
Gromark C, Hesselmark E, Djupedal IG, Silverberg M, Horne A, Harris RA, et al. A two-to-five year follow-up of a pediatric acute-onset neuropsychiatric syndrome cohort. Child Psychiatry Hum Dev. 2022;53(2):354–64.
Masterson EE, Miles K, Schlenk N, Manko C, Ma M, Farhadian B, Chang K, Silverman M, Thienemann M, Frankovich J. Defining clinical course of patients evaluated for pediatric acute-onset neuropsychiatric syndrome (PANS): phenotypic classification based on 10 years of clinical data. Dev Neurosci. 2025:1–33. https://doi.org/10.1159/000545598.
Chang K, Frankovich J, Cooperstock M, Cunningham MW, Latimer ME, Murphy TK, et al. Clinical evaluation of youth with pediatric acute-onset neuropsychiatric syndrome (PANS): recommendations from the 2013 PANS consensus conference. J Child Adolesc Psychopharmacol. 2015;25(1):3–13.
Vreeland A, Thienemann M, Cunningham M, Muscal E, Pittenger C, Frankovich J. Neuroinflammation in obsessive-compulsive disorder: Sydenham chorea, pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections, and pediatric acute onset neuropsychiatric syndrome. Psychiatr Clin North Am. 2023;46(1):69–88.
Gagliano A, Carta A, Tanca MG, Sotgiu S. Pediatric acute-onset neuropsychiatric syndrome: current perspectives. Neuropsychiatr Dis Treat. 2023. https://doi.org/10.2147/NDT.S362202.
Leonardi L, Perna C, Bernabei I, Fiore M, Ma M, Frankovich J, et al. Pediatric acute-onset neuropsychiatric syndrome (PANS) and pediatric autoimmune neuropsychiatric disorders associated with Streptococcal infections (PANDAS): immunological features underpinning controversial entities. Children (Basel). 2024;11(9):1043.
Murphy TK, Patel PD, McGuire JF, Kennel A, Mutch PJ, Parker-Athill EC, et al. Characterization of the pediatric acute-onset neuropsychiatric syndrome phenotype. J Child Adolesc Psychopharmacol. 2015;25(1):14–25.
Gromark C, Harris RA, Wickström R, Horne A, Silverberg-Mörse M, Serlachius E, et al. Establishing a pediatric Acute-Onset neuropsychiatric syndrome clinic: baseline clinical features of the pediatric Acute-Onset neuropsychiatric syndrome cohort at Karolinska Institutet. J Child Adolesc Psychopharmacol. 2019;29(8):625–33.
Johnson M, Fernell E, Preda I, Wallin L, Fasth A, Gillberg C, et al. Paediatric acute-onset neuropsychiatric syndrome in children and adolescents: an observational cohort study. The Lancet Child & Adolescent Health. 2019;3(3):175–80.
Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunol. 2016;16(10):626–38.
Masterson EE, Gavin JM. Baseline characteristics of children in the international PANS registry (IPR) epidemiology study. BMJ Open. 2024;14(1):e072743.
Gao J, Chan A, Willett T, Farhadian B, Silverman M, Tran P, et al. Sex and aggression characteristics in a cohort of patients with pediatric acute-onset neuropsychiatric syndrome. J Child Adolesc Psychopharmacol. 2022;32(8):444–52.
Calaprice D, Tona J, Parker-Athill EC, Murphy TK. A survey of pediatric acute-onset neuropsychiatric syndrome characteristics and course. J Child Adolesc Psychopharmacol. 2017;27(7):607–18.
Ma M, Masterson EE, Gao J, Karpel H, Chan A, Pooni R, et al. Development of autoimmune diseases among children with pediatric acute-onset neuropsychiatric syndrome. JAMA Netw Open. 2024;7(7):e2421688-2421688.
Zheng J, Frankovich J, McKenna ES, Rowe NC, MacEachern SJ, Ng NN, et al. Association of pediatric acute-onset neuropsychiatric syndrome with microstructural differences in brain regions detected via diffusion-weighted magnetic resonance imaging. JAMA Netw Open. 2020;3(5):e204063-204063.
Kumar A, Williams MT, Chugani HT. Evaluation of basal ganglia and thalamic inflammation in children with pediatric autoimmune neuropsychiatric disorders associated with Streptococcal infection and tourette syndrome: a positron emission tomographic (PET) study using 11 C-[R]-PK11195. J Child Neurol. 2015;30(6):749–56.
Giedd JN, Rapoport JL, Garvey MA, Perlmutter S, Swedo SE. MRI assessment of children with obsessive-compulsive disorder or tics associated with streptococcal infection. Am J Psychiatry. 2000;157(2):281–3.
Cabrera B, Romero-Rebollar C, Jiménez-Ángeles L, Genis-Mendoza AD, Flores J, Lanzagorta N, Arroyo M, de la Fuente-Sandoval C, Santana D, Medina-Bañuelos V, et al. Neuroanatomical features and its usefulness in classification of patients with PANDAS. CNS Spectr. 2019;24(5):533–43.
Gaughan T, Buckley A, Hommer R, Grant P, Williams K, Leckman JF, et al. Rapid eye movement sleep abnormalities in children with pediatric acute-onset neuropsychiatric syndrome (PANS). J Clin Sleep Med. 2016;12(7):1027–32.
Santoro JD, Frankovich J, Bhargava S. Continued presence of period limb movements during REM sleep in patients with chronic static pediatric acute-onset neuropsychiatric syndrome (PANS). J Clin Sleep Med. 2018;14(7):1187–92.
Gagliano A, Puligheddu M, Ronzano N, Congiu P, Tanca MG, Cursio I, et al. Artificial neural networks analysis of polysomnographic and clinical features in pediatric Acute-Onset neuropsychiatric syndrome (PANS): from sleep alteration to brain fog. Nat Sci Sleep. 2021;13:1209–24.
Congiu P, Gagliano A, Carucci S, Lanza G, Ferri R, Puligheddu M. REM sleep Atonia in patients with pediatric acute-onset neuropsychiatric syndrome (PANS): implications for pathophysiology. J Clin Sleep Med. 2024. https://doi.org/10.5664/jcsm.11544.
Zebrack JE, Gao J, Verhey B, Tian L, Stave C, Farhadian B, et al. Neurological soft signs at presentation in patients with pediatric acute-onset neuropsychiatric syndrome. JAMA Netw Open. 2025;8(3):e250314.
Xu J, Frankovich J, Liu RJ, Thienemann M, Silverman M, Farhadian B, et al. Elevated antibody binding to striatal cholinergic interneurons in patients with pediatric acute-onset neuropsychiatric syndrome. Brain Behav Immun. 2024;122:241–55.
Xu J, Liu RJ, Fahey S, Frick L, Leckman J, Vaccarino F, Duman RS, Williams K, Swedo S, Pittenger C. Antibodies from children with PANDAS bind specifically to striatal cholinergic interneurons and alter their activity. Am J Psychiatry. 2021;178(1):48–64.
Frick LR, Rapanelli M, Jindachomthong K, Grant P, Leckman JF, Swedo S, et al. Differential binding of antibodies in PANDAS patients to cholinergic interneurons in the striatum. Brain Behav Immun. 2018;69:304–11.
Chain JL, Alvarez K, Mascaro-Blanco A, Reim S, Bentley R, Hommer R, Grant P, Leckman JF, Kawikova I, Williams K, et al. Autoantibody biomarkers for basal ganglia encephalitis in Sydenham chorea and pediatric autoimmune neuropsychiatric disorder associated with Streptococcal infections. Front Psychiatry. 2020;11:564.
Brimberg L, Benhar I, Mascaro-Blanco A, Alvarez K, Lotan D, Winter C, et al. Behavioral, pharmacological, and immunological abnormalities after streptococcal exposure: a novel rat model of Sydenham chorea and related neuropsychiatric disorders. Neuropsychopharmacology. 2012;37(9):2076–87.
Yaddanapudi K, Hornig M, Serge R, De Miranda J, Baghban A, Villar G, et al. Passive transfer of streptococcus-induced antibodies reproduces behavioral disturbances in a mouse model of pediatric autoimmune neuropsychiatric disorders associated with streptococcal infection. Mol Psychiatry. 2010;15(7):712–26.
Kirvan CA, Swedo SE, Snider LA, Cunningham MW. Antibody-mediated neuronal cell signaling in behavior and movement disorders. J Neuroimmunol. 2006;179(1–2):173–9.
Cox CJ, Zuccolo AJ, Edwards EV, Mascaro-Blanco A, Alvarez K, Stoner J, Chang K, Cunningham MW. Antineuronal antibodies in a heterogeneous group of youth and young adults with tics and obsessive-compulsive disorder. J Child Adolesc Psychopharmacol. 2015;25(1):76–85.
Cox CJ, Sharma M, Leckman JF, Zuccolo J, Zuccolo A, Kovoor A, et al. Brain human monoclonal autoantibody from Sydenham chorea targets dopaminergic neurons in transgenic mice and signals dopamine D2 receptor: implications in human disease. J Immunol. 2013;191(11):5524–41.
Menendez CM, Zuccolo J, Swedo SE, Reim S, Richmand B, Ben-Pazi H, Kovoor A, Cunningham MW. Dopamine receptor autoantibody signaling in infectious sequelae differentiates movement versus neuropsychiatric disorders. JCI Insight. 2024;9(21):e164762.
Ben-Pazi H, Stoner JA, Cunningham MW. Dopamine receptor autoantibodies correlate with symptoms in Sydenham’s chorea. PLoS ONE. 2013;8(9):e73516.
Rodríguez N, Lázaro L, Ortiz AE, Morer A, Martínez-Pinteño A, Segura AG, et al. Gene expression study in monocytes: evidence of inflammatory dysregulation in early-onset obsessive-compulsive disorder. Transl Psychiatry. 2022;12(1):1–10.
Rodríguez N, Morer A, González-Navarro EA, Serra-Pages C, Boloc D, Torres T, et al. Inflammatory dysregulation of monocytes in pediatric patients with obsessive-compulsive disorder. J Neuroinflammation. 2017;14(1):261.
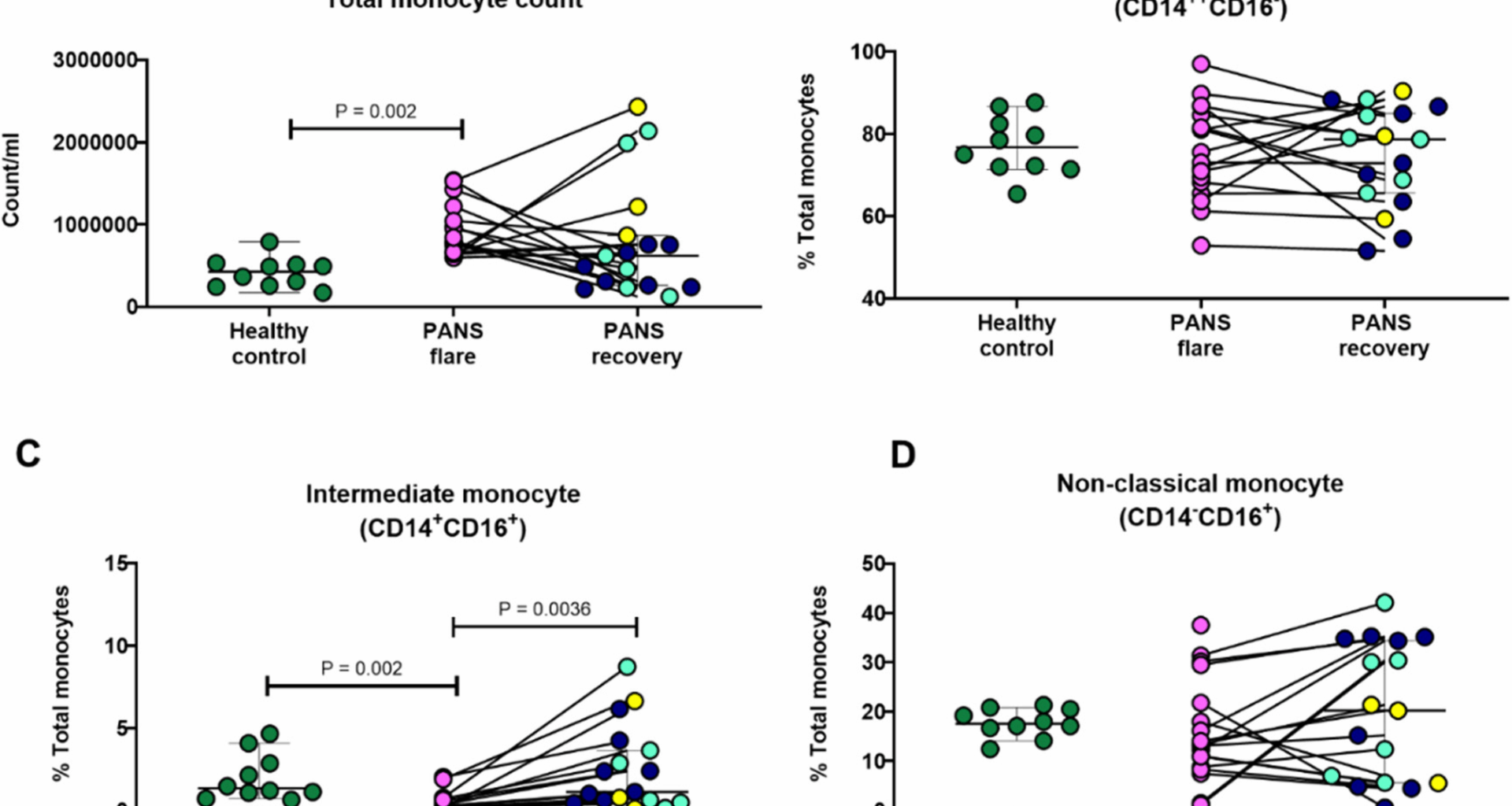
Melamed I, Rahman S, Pein H, Heffron M, Frankovich J, Kreuwel H, Mellins ED. IVIG response in pediatric acute-onset neuropsychiatric syndrome correlates with reduction in pro-inflammatory monocytes and neuropsychiatric measures. Front Immunol. 2024;15:1383973.
Swirski FK, Nahrendorf M, Etzrodt M, Wildgruber M, Cortez-Retamozo V, Panizzi P, et al. Identification of splenic reservoir monocytes and their deployment to inflammatory sites. Science. 2009;325(5940):612–6.
Gaudillière B, Fragiadakis GK, Bruggner RV, Nicolau M, Finck R, Tingle M, et al. Clinical recovery from surgery correlates with single-cell immune signatures. Sci Transl Med. 2014;6(255):ra255131-255131.
Patel AA, Zhang Y, Fullerton JN, Boelen L, Rongvaux A, Maini AA, et al. The fate and lifespan of human monocyte subsets in steady state and systemic inflammation. J Exp Med. 2017;214(7):1913–23.
Cormican S, Griffin MD. Human monocyte subset distinctions and function: insights from gene expression analysis. Front Immunol. 2020;11:1070.
Atri C, Guerfali FZ, Laouini D. Role of human macrophage polarization in inflammation during infectious diseases. Int J Mol Sci. 2018. https://doi.org/10.3390/ijms19061801.
Palframan RT, Jung S, Cheng G, Weninger W, Luo Y, Dorf M, et al. Inflammatory chemokine transport and presentation in HEV: a remote control mechanism for monocyte recruitment to lymph nodes in inflamed tissues. J Exp Med. 2001;194(9):1361–74.
Ranjbar M, Rahimi A, Baghernejadan Z, Ghorbani A, Khorramdelazad H. Role of CCL2/CCR2 axis in the pathogenesis of COVID-19 and possible treatments: all options on the table. Int Immunopharmacol. 2022;113(Pt A):109325.
Panek CA, Ramos MV, Mejias MP, Abrey-Recalde MJ, Fernandez-Brando RJ, Gori MS, Salamone GV, Palermo MS. Differential expression of the fractalkine chemokine receptor (CX 3 CR1) in human monocytes during differentiation. Cell Mol Immunol. 2015;12(6):669–80.
Yang J, Zhang L, Yu C, Yang X-F, Wang H. Monocyte and macrophage differentiation: circulation inflammatory monocyte as biomarker for inflammatory diseases. Biomark Res. 2014;2(1):1.
Reader BF, Jarrett BL, McKim DB, Wohleb ES, Godbout JP, Sheridan JF. Peripheral and central effects of repeated social defeat stress: monocyte trafficking, microglial activation, and anxiety. Neuroscience. 2015;289:429–42.
Takeshita Y, Ransohoff RM. Inflammatory cell trafficking across the blood–brain barrier: chemokine regulation and in vitro models. Immunol Rev. 2012;248(1):228–39.
Mareckova H, Havrdova E, Krasulova E, Vankova Z, Koberova M, Šterzl I. Natalizumab in the treatment of patients with multiple sclerosis: first experience. Ann N Y Acad Sci. 2007;1110(1):465–73.
Stüve O, Marra CM, Jerome KR, Cook L, Cravens PD, Cepok S, et al. Immune surveillance in multiple sclerosis patients treated with natalizumab. Ann Neurol. 2006;59(5):743–7.
Levesque MC, Heinly CS, Whichard LP, Patel DD. Cytokine‐regulated expression of activated leukocyte cell adhesion molecule (CD166) on monocyte‐lineage cells and in rheumatoid arthritis synovium. Arthritis Rheum. 1998;41(12):2221–9.
Williams DW, Eugenin EA, Calderon TM, Berman JW. Monocyte maturation, HIV susceptibility, and transmigration across the blood brain barrier are critical in HIV neuropathogenesis. J Leukoc Biol. 2012;91(3):401–15.
Cayrol R, Wosik K, Berard JL, Dodelet-Devillers A, Ifergan I, Kebir H, Haqqani AS, Kreymborg K, Krug S, Moumdjian R. Activated leukocyte cell adhesion molecule promotes leukocyte trafficking into the central nervous system. Nat Immunol. 2008;9(2):137.
Macaubas C, Nguyen K, Deshpande C, Phillips C, Peck A, Lee T, et al. Distribution of circulating cells in systemic juvenile idiopathic arthritis across disease activity states. Clin Immunol. 2010;134(2):206–16.
Rustenhoven J, Drieu A, Mamuladze T, de Lima KA, Dykstra T, Wall M, Papadopoulos Z, Kanamori M, Salvador AF, Baker W, et al. Functional characterization of the dural sinuses as a neuroimmune interface. Cell. 2021;184(4):1000–e10161027.
Lun ATL, Riesenfeld S, Andrews T, Dao TP, Gomes T, Marioni JC. Participants in the 1st human cell atlas J: emptydrops: distinguishing cells from empty droplets in droplet-based single-cell RNA sequencing data. Genome Biol. 2019;20(1):63.
Griffiths JA, Richard AC, Bach K, Lun ATL, Marioni JC. Detection and removal of barcode swapping in single-cell RNA-seq data. Nat Commun. 2018;9(1):2667.
Galfrè SG, Morandin F, Pietrosanto M, Cremisi F, Helmer-Citterich M. COTAN: scRNA-seq data analysis based on gene co-expression. NAR Genomics Bioinform. 2021;3(3):lqab072.
McGinnis CS, Murrow LM, Gartner ZJ. Doubletfinder: doublet detection in single-cell RNA sequencing data using artificial nearest neighbors. Cell Syst. 2019;8(4):329-e337324.
Hao Y, Stuart T, Kowalski MH, Choudhary S, Hoffman P, Hartman A, Srivastava A, Molla G, Madad S, Fernandez-Granda C, et al. Dictionary learning for integrative, multimodal and scalable single-cell analysis. Nat Biotechnol. 2024;42(2):293–304.
Butler A, Hoffman P, Smibert P, Papalexi E, Satija R. Integrating single-cell transcriptomic data across different conditions, technologies, and species. Nat Biotechnol. 2018;36(5):411–20.
Bongen E, Lucian H, Khatri A, Fragiadakis GK, Bjornson ZB, Nolan GP, Utz PJ, Khatri P. Sex differences in the blood transcriptome identify robust changes in immune cell proportions with aging and influenza infection. Cell Rep. 2019;29(7):1961–73. e1964.
Martinez FO, Gordon S. The M1 and M2 paradigm of macrophage activation: time for reassessment. F1000prime reports. 2014;6. https://doi.org/10.12703/P6-13.
Bernardo D, Marin A, Fernández-Tomé S, Montalban-Arques A, Carrasco A, Tristán E, Ortega-Moreno L, Mora-Gutiérrez I, Díaz-Guerra A, Caminero-Fernández R. Human intestinal pro-inflammatory CD11c high CCR2 + CX3CR1 + macrophages, but not their tolerogenic CD11c – CCR2 – CX3CR1 – counterparts, are expanded in inflammatory bowel disease. Mucosal Immunol. 2018;11(4):1114.
Sallusto F, Lanzavecchia A. Efficient presentation of soluble antigen by cultured human dendritic cells is maintained by granulocyte/macrophage colony-stimulating factor plus interleukin 4 and downregulated by tumor necrosis factor alpha. J Exp Med. 1994;179(4):1109–18.
Lee JS, Jeong S-J, Kim S, Chalifour L, Yun TJ, Miah MA, et al. Conventional dendritic cells impair recovery after myocardial infarction. J Immunol. 2018;201(6):1784–98.
Alcántara-Hernández M, Leylek R, Wagar LE, Engleman EG, Keler T, Marinkovich MP, Davis MM, Nolan GP, Idoyaga J. High-dimensional phenotypic mapping of human dendritic cells reveals interindividual variation and tissue specialization. Immunity. 2017;47(6):1037–50. e1036.
van Beek JJ, Gorris MA, Sköld AE, Hatipoglu I, Van Acker HH, Smits EL, de Vries IJM, Bakdash G. Human blood myeloid and plasmacytoid dendritic cells cross activate each other and synergize in inducing NK cell cytotoxicity. Oncoimmunology. 2016;5(10):e1227902.
Minoda Y, Virshup I, Leal Rojas I, Haigh O, Wong Y, Miles JJ, Wells CA, Radford KJ. Human CD141 + dendritic cell and CD1c + dendritic cell undergo concordant early genetic programming after activation in humanized mice in vivo. Front Immunol. 2017;8:1419.
Cai G, Du M, Bossé Y, Albrecht H, Qin F, Luo X, et al. SARS-CoV-2 impairs dendritic cells and regulates DC-SIGN gene expression in tissues. Int J Mol Sci. 2021;22(17):9228.
Dileepan T, Smith ED, Knowland D, Hsu M, Platt M, Bittner-Eddy P, et al. Group A Streptococcus intranasal infection promotes CNS infiltration by streptococcal-specific Th17 cells. J Clin Invest. 2016;126(1):303–17.
Platt MP, Agalliu D, Cutforth T. Hello from the other side: how autoantibodies circumvent the Blood-Brain barrier in autoimmune encephalitis. Front Immunol. 2017;8:442.
Platt MP, Bolding KA, Wayne CR, Chaudhry S, Cutforth T, Franks KM, et al. Th17 lymphocytes drive vascular and neuronal deficits in a mouse model of postinfectious autoimmune encephalitis. Proc Natl Acad Sci U S A. 2020;117(12):6708–16.
Dale RC, Merheb V, Pillai S, Wang D, Cantrill L, Murphy TK, et al. Antibodies to surface dopamine-2 receptor in autoimmune movement and psychiatric disorders. Brain. 2012;135(Pt 11):3453–68.
Kim W-K, Alvarez X, Fisher J, Bronfin B, Westmoreland S, McLaurin J, et al. CD163 identifies perivascular macrophages in normal and viral encephalitic brains and potential precursors to perivascular macrophages in blood. Am J Pathol. 2006;168(3):822–34.
Caldwell BA, Li L. Epigenetic regulation of innate immune dynamics during inflammation. J Leukoc Biol. 2024;115(4):589–606.
Cugurra A, Mamuladze T, Rustenhoven J, Dykstra T, Beroshvili G, Greenberg ZJ, Baker W, Papadopoulos Z, Drieu A, Blackburn S. Skull and vertebral bone marrow are myeloid cell reservoirs for the meninges and CNS parenchyma. Science. 2021;373(6553):eabf7844.
Mastorakos P, McGavern D. The anatomy and immunology of vasculature in the central nervous system. Sci Immunol. 2019. https://doi.org/10.1126/sciimmunol.aav0492.
Chuluundorj D, Harding SA, Abernethy D, La Flamme AC. Expansion and preferential activation of the CD14(+)CD16(+) monocyte subset during multiple sclerosis. Immunol Cell Biol. 2014;92(6):509–17.
Di Pardo A, Alberti S, Maglione V, Amico E, Cortes EP, Elifani F, Battaglia G, Busceti CL, Nicoletti F, Vonsattel JG, et al. Changes of peripheral TGF-β1 depend on monocytes-derived macrophages in huntington disease. Mol Brain. 2013;6(1):55.
Vogel DY, Kooij G, Heijnen PD, Breur M, Peferoen LA, van der Valk P, et al. GM-CSF promotes migration of human monocytes across the blood brain barrier. Eur J Immunol. 2015;45(6):1808–19.
Janssens K, Slaets H, Hellings N. Immunomodulatory properties of the IL-6 cytokine family in multiple sclerosis. Ann N Y Acad Sci. 2015;1351:52–60.
Fiedler SE, George JD, Love HN, Kim E, Spain R, Bourdette D, Salinthone S. Analysis of IL-6, IL-1β and TNF-α production in monocytes isolated from multiple sclerosis patients treated with disease modifying drugs. J Syst Integr Neurosci. 2017;3(3). https://doi.org/10.15761/JSIN.1000166.
Roth J, Rummel C, Harré E-M, Voss T, Mütze J, Gerstberger R, et al. Is interleukin-6 the necessary pyrogenic cytokine? J Therm Biol. 2004;29(7):383–9.
Choi BR, Johnson KR, Maric D, McGavern DB. Monocyte-derived IL-6 programs microglia to rebuild damaged brain vasculature. Nat Immunol. 2023;24(7):1110–23.
Hatori K, Nagai A, Heisel R, Ryu JK, Kim SU. Fractalkine and fractalkine receptors in human neurons and glial cells. J Neurosci Res. 2002;69(3):418–26.
Vogel DY, Heijnen PD, Breur M, de Vries HE, Tool AT, Amor S, Dijkstra CD. Macrophages migrate in an activation-dependent manner to chemokines involved in neuroinflammation. J Neuroinflamm. 2014;11(1):1–11.
Mangaonkar AA, Tande AJ, Bekele DI. Differential diagnosis and workup of monocytosis: a systematic approach to a common hematologic finding. Curr Hematol Malig Rep. 2021;16(3):267–75.
Agrawal S, Salazar J, Tran TM, Agrawal A. Sex-related differences in innate and adaptive immune responses to SARS-CoV-2. Front Immunol. 2021;12:739757.
Chamekh M, Deny M, Romano M, Lefèvre N, Corazza F, Duchateau J, Casimir G. Differential susceptibility to infectious respiratory diseases between males and females linked to sex-specific innate immune inflammatory response. Front Immunol. 2017;8:1806.
Jaillon S, Berthenet K, Garlanda C. Sexual dimorphism in innate immunity. Clin Rev Allergy Immunol. 2019;56:308–21.
Ferri SL, Abel T, Brodkin ES. Sex differences in autism spectrum disorder: a review. Curr Psychiatry Rep. 2018;20:1–17.
Flanagan EP, Geschwind MD, Lopez-Chiriboga AS, Blackburn KM, Turaga S, Binks S, Zitser J, Gelfand JM, Day GS, Dunham SR. Autoimmune encephalitis misdiagnosis in adults. JAMA Neurol. 2023;80(1):30–9.
Mirsafian H, Ripen AM, Leong W-M, Manaharan T, Mohamad SB, Merican AF. Transcriptome landscape of human primary monocytes at different sequencing depth. Genomics. 2017;109(5–6):463–70.
Kay E, Gomez-Garcia L, Woodfin A, Scotland RS, Whiteford JR. Sexual dimorphisms in leukocyte trafficking in a mouse peritonitis model. J Leukoc Biol. 2015;98(5):805–17.
Marzaioli V, Canavan M, Floudas A, Wade SC, Low C, Veale DJ, Fearon U. Monocyte-derived dendritic cell differentiation in inflammatory arthritis is regulated by the JAK/STAT axis via NADPH oxidase regulation. Front Immunol. 2020;11:1406.
Perdiguero EG, Klapproth K, Schulz C, Busch K, Azzoni E, Crozet L, Garner H, Trouillet C, De Bruijn MF, Geissmann F. Tissue-resident macrophages originate from yolk-sac-derived erythro-myeloid progenitors. Nature. 2015;518(7540):547–51.
Frankovich J, Leibold CM, Farmer C, Sainani K, Kamalani G, Farhadian B, Willett T, Park JM, Sidell D, Ahmed S et al. The burden of caring for a child or adolescent with pediatric Acute-Onset neuropsychiatric syndrome (PANS): an observational longitudinal study. J Clin Psychiatry. 2018;80(1). https://doi.org/10.4088/JCP.17m12091.
Kapellos TS, Bonaguro L, Gemünd I, Reusch N, Saglam A, Hinkley ER, Schultze JL. Human monocyte subsets and phenotypes in major chronic inflammatory diseases. Front Immunol. 2019;10:2035.
Zhang G, Yao Q, Long C, Yi P, Song J, Wu L, et al. Infiltration by monocytes of the central nervous system and its role in multiple sclerosis: reflections on therapeutic strategies. Neural Regen Res. 2025;20(3):779–93.