Bärnighausen T, Røttingen JA, Rockers P, Shemilt I, Tugwell P. Quasi-experimental study designs series—paper 1: introduction: two historical lineages. J Clin Epidemiol. 2017;89:4–11.
Ogilvie D, Adams J, Bauman A, et al. Using natural experimental studies to guide public health action: turning the evidence-based medicine paradigm on its head. J Epidemiol Community Health. 2019. https://doi.org/10.1136/jech-2019-213085.
Reeves BC, Wells GA, Waddington H. Quasi-experimental study designs series—paper 5: a checklist for classifying studies evaluating the effects on health interventions—a taxonomy without labels. J Clin Epidemiol. 2017;89:30–42.
Glanville J, Eyers J, Jones AM, et al. Quasi-experimental study designs series—paper 8: identifying quasi-experimental studies to inform systematic reviews. J Clin Epidemiol. 2017;89:67–76.
Basu S, Meghani A, Siddiqi A. Evaluating the health impact of large-scale public policy changes: classical and novel approaches. Annu Rev Public Health. 2017;38:351–70.
Abreu D, Pinto F, Matias-Dias C, Sousa P. Trends of case-fatality rate by acute coronary syndrome in Portugal: impact of a fast track to the coronary unit. JRSM Cardiovasc Dis. 2019;8:204800401985195.
Kislaya I, Rodrigues AP, Sousa-Uva M, et al. Indirect effect of 7-valent and 13-valent Pneumococcal conjugated vaccines on Pneumococcal pneumonia hospitalizations in elderly. PLoS ONE. 2019;14(1):65–74.
Torres AR, Rodrigues AP, Sousa-Uva M, et al. Impact of stringent non-pharmaceutical interventions applied during the second and third COVID-19 epidemic waves in Portugal, 9 November 2020 to 10 February 2021: an ecological study. Eurosurveillance. 2022;27(3):1–12.
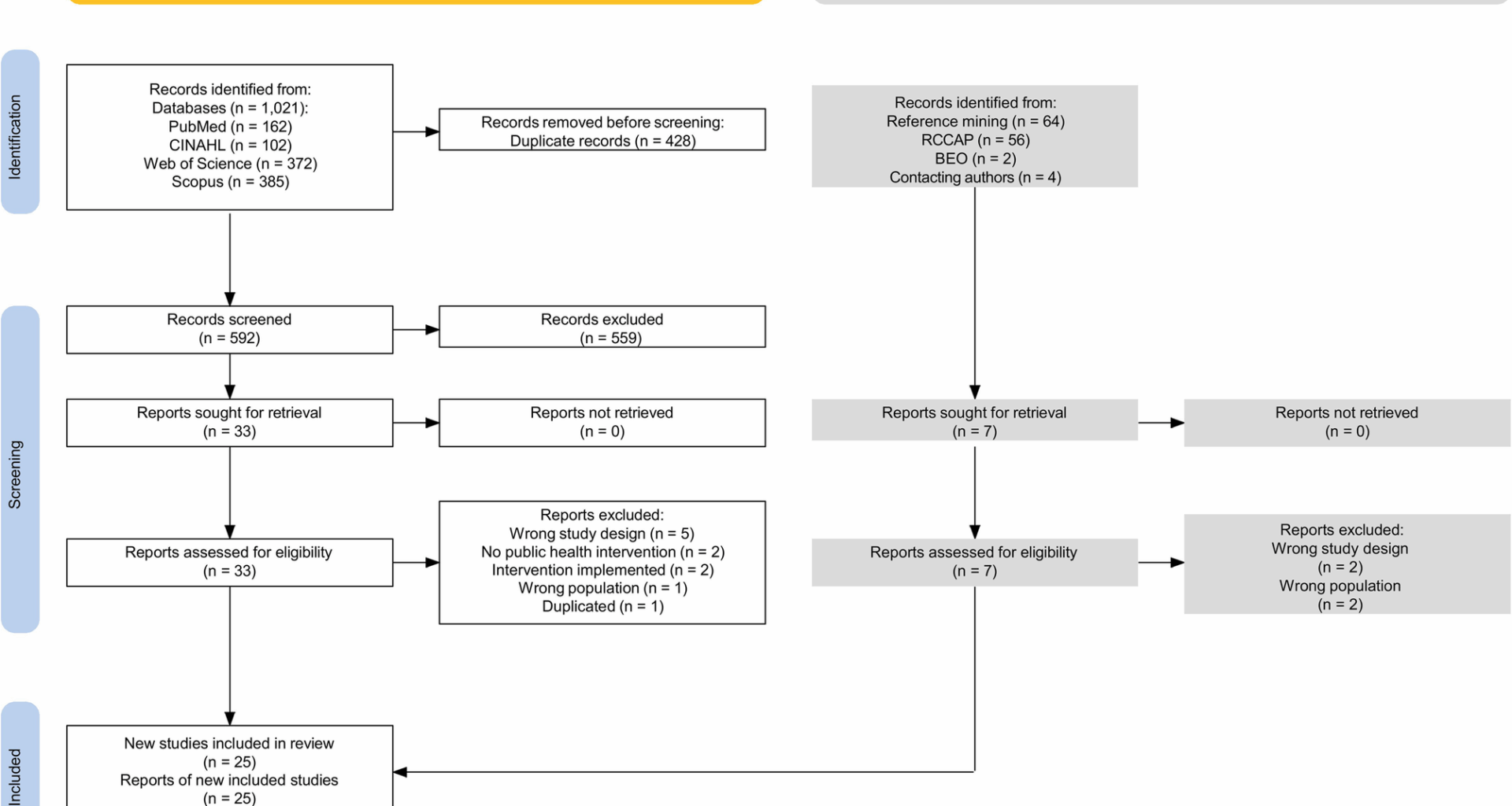
Tricco AC, Lillie E, Zarin W, et al. Preferred reporting items for systematic reviews and Meta-Analyses extension for scoping reviews (PRISMA-ScR) checklist SECTION. Ann Intern Med. 2018;169(7):11–2.
Leite A, Kislaya I, Machado A, Aguiar P, Nunes B, Matias Dias C. Use of quasi-experimental studies to evaluate causal effects of public health interventions in portugal: a scoping review protocol. 2022. Available from: osf.io/zex3v. Cited 2022 Sep 26.
Open Science Framework (OSF). Available from: https://doi.org/10.17605/OSF.IO/G9KVE. cited 2022 Sep 26.
Instituto Nacional de Saúde Doutor Ricardo Jorge. Boletim Epidemiológico Observações [Internet]. [cited 2022 Sep 26]. Available from: https://www.insa.min-saude.pt/category/informacao-e-cultura-cientifica/publicacoes/boletim-epidemiologico-observacoes/
Bond, University. Institute for evidence-based healthcare. SR-Accelerator. Available from: https://sr-accelerator.com/#/. Cited 2024 Mar 21.
Rayyan. – Intelligent Systematic Review – Rayyan. Available from: https://www.rayyan.ai/. Cited 2022 Sep 26.
Waddington H, Aloe AM, Becker BJ, et al. Quasi-experimental study designs series—paper 6: risk of bias assessment. J Clin Epidemiol. 2017;89:43–52.
de Vocht F, Katikireddi SV, McQuire C, Tilling K, Hickman M, Craig P. Conceptualising natural and quasi experiments in public health. BMC Med Res Methodol. 2021;21(1):1–8.
Haddaway NR, Page MJ, Pritchard CC, McGuinness LA. PRISMA2020: an R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and open synthesis. Campbell Syst Rev. 2022;18(2):1–12.
Abreu D, Sousa P, Matias-Dias C, Pinto FJ. Longitudinal impact of the smoking ban legislation in acute coronary syndrome admissions. BioMed Res Int. 2017. https://doi.org/10.1155/2017/6956941.
Abreu D, Sousa P, Matias-Dias C, Pinto FJ. Cardiovascular disease and high blood pressure trend analyses from 2002 to 2016: after the implementation of a salt reduction strategy. BMC Public Health. 2018;18(1):722.
Abreu D, Sousa P, Matias-Dias C, Pinto F. Impact of public health initiatives on acute coronary syndrome fatality rates in Portugal. Rev Port Cardiol. 2020;39(1):27–34.
Adam C, Raschzok A. Cannabis policy and the uptake of treatment for cannabis-related problems. Drug Alcohol Rev. 2017;36(2):171–7.
Aiken ARA, Starling JE, Gomperts R, Scott JG, Aiken CE. Demand for self-managed online telemedicine abortion in eight European countries during the COVID-19 pandemic: a regression discontinuity analysis. BMJ Sex Reprod Health. 2021;47(4):238–45.
Bellerba F, Bardeck N, Boehm M, et al. SARS-CoV-2 trends in Italy, Germany and Portugal and school opening during the period of Omicron variant dominance: a quasi experimental study in the EuCARE project. Int J Infect Dis. 2024. https://doi.org/10.1016/j.ijid.2023.11.002.
Benedetti E, Resce G, Brunori P, Molinaro S. Cannabis policy changes and adolescent cannabis use: evidence from Europe. Int J Environ Res Public Health. 2021. https://doi.org/10.3390/ijerph18105174.
Dimitrovová K, Perelman J, Serrano-Alarcón M. Effect of a national primary care reform on avoidable hospital admissions (2000–2015): a difference-in-difference analysis. Soc Sci Med. 2020;252:112908.
Fernandes OB, Lopes S, Marques AP, Moita B, Sarmento J, Santana R. Local health units in Portugal: the influence of chronic conditions on inpatient readmissions. Port J Public Heal. 2020;37(2–3):91–9.
Gonçalves J, Pereira Dos Santos J. Brown sugar, how come you taste so good? The impact of a soda tax on prices and consumption. Soc Sci Med. 2020;264:113332.
Hoffman SJ, Poirier MJP, Van Rogers S, Baral P, Sritharan L. Impact of the WHO framework convention on tobacco control on global cigarette consumption: Quasi-experimental evaluations using interrupted time series analysis and in-sample forecast event modelling. BMJ. 2019;365.
Leitão C, Silva S, Roquette R, Uva M, Baltazar N. Será Que Os Planos de contingência Para Ondas de Calor reduzem a Mortalidade associada Ao Calor ? Um Estudo Da diferença-das-diferenças Em Portugal (Do heat contingency plans reduce heat related deaths? A difference-in-difference study in Portugal). Obs Bol Epidemiológico – Inst Nac Saúde Dr Ricardo Jorge. 2020;26:4–8.
Lopes S, Fernandes ÓB, Marques AP, Moita B, Sarmento J, Santana R. Can vertical integration reduce hospital readmissions? A difference-in-differences approach. Med Care. 2017;55(5):506–13.
Pereira AM, Pereira RM, Dos Santos JP. For whom the bell tolls: road safety effects of tolls ouncongested SCUT highways in Portugal. J Infrastructure Policy Dev. 2020;4(2):287–305.
Pinto D, Silva A, Heleno B, Rodrigues DS, Santos I, Caetano PA. Effect of European medicines agency’s regulatory measures on nimesulide utilization in Portugal. Pharmacoepidemiol Drug Saf. 2018;27(6):630–7.
Pinto D, Silva A, Heleno B, Rodrigues DS, Santos I, Caetano PA. Effect of European medicines agency’s restrictions on Trimetazidine utilization in Portugal. Pharmacoepidemiol Drug Saf. 2018;27(9):962–8.
Ramos P, Almeida A. The impact of an increase in user costs on the demand for emergency services: the case of Portuguese hospitals. Health Econ. 2016;25(11):1372–88.
Ricoca Peixoto V, Vieira A, Aguiar P, Carvalho C, Rhys Thomas D, Abrantes A. Initial assessment of the impact of the emergency state lockdown measures on the 1st wave of the COVID-19 epidemic in Portugal. Acta Med Port. 2020;33(11):733–41.
Sánchez R. Does a mandatory reduction of standard working hours improve employees’. health status? Ind Relat. 2017;56(1):3–39.
Sassano M, Mariani M, Pastorino R, Ricciardi W, La Vecchia C, Boccia S. Association of national smoke-free policies with per-capita cigarette consumption and acute myocardial infarction mortality in Europe. J Epidemiol Community Health. 2024. https://doi.org/10.1136/jech-2023-220746.
Torres AR, Rodrigues AP, Sousa-Uva M et al. Impact of stringent non-pharmaceutical interventions applied during the second and third COVID-19 epidemic waves in Portugal, 9 November 2020 to 10 February 2021: an ecological study. Euro Surveill. 2022;27(23).
Torres AR, Silva S, Kislaya I, et al. Impact of lifting mask mandates on COVID-19 incidence and mortality in portugal: an ecological study. Acta Med Port. 2023;36(10):661–9.
Vaz S, Ramos P. Where did civil servants go? The effect of an increase in public co-payments on double insured patients. Health Econ Rev. 2016;6(1):16.
Matthay EC, Glymour MM. Causal inference challenges and new directions for epidemiologic research on the health effects of social policies. Curr Epidemiol Rep. 2022;9(1):22–37.
Jandoc R, Burden AM, Mamdani M, Lévesque LE, Cadarette SM. Interrupted time series analysis in drug utilization research is increasing: systematic review and recommendations. J Clin Epidemiol. 2015;68(8):950–6.
Hilton Boon M, Craig P, Thomson H, Campbell M, Moore L. Regres Discontinuity Designs Health: Syst Rev Epidemiol. 2021;32(1):87–93.
Kennedy-Shaffer L. Quasi-experimental methods for pharmacoepidemiology: difference-in-differences and synthetic control methods with case studies for vaccine evaluation. Am J Epidemiol. 2024;193(7):1050–8.
Hategeka C, Ruton H, Karamouzian M, Lynd LD, Law MR. Use of interrupted time series methods in the evaluation of health system quality improvement interventions: A methodological systematic review. BMJ Glob Heal. 2020;5(10):1–13.
Ewusie JE, Soobiah C, Blondal E, Beyene J, Thabane L, Hamid JS. Methods, applications and challenges in the analysis of interrupted time series data: A scoping review. J Multidiscip Healthc. 2020;13:411–23.
Albers PN, Rinaldi C, Brown H, et al. Natural experiments for the evaluation of place-based public health interventions: a methodology scoping review. Front Public Health. 2023. https://doi.org/10.3389/fpubh.2023.1192055.
Akter S, Islam MR, Rahman MM, et al. Evaluation of population-level tobacco control interventions and health outcomes: a systematic review and meta-analysis. JAMA Netw Open. 2023;6(7):E2322341.
Moscoe E, Bor J, Bärnighausen T. Regression discontinuity designs are underutilized in medicine, epidemiology, and public health: a review of current and best practice. J Clin Epidemiol. 2015;68(2):132–43.
Wang G, Hamad R, White JS. Advances in difference-in-differences methods for policy evaluation research. Epidemiology. 2024;35(5):628–37.
Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46(1):348–55.
Rothbard S, Etheridge JC, Murray EJ. A tutorial on applying the difference-in-differences method to health data. Curr Epidemiol Rep. 2023;11(2):85–95.
Turner SL, Karahalios A, Forbes AB, et al. Design characteristics and statistical methods used in interrupted time series studies evaluating public health interventions: a review. J Clin Epidemiol. 2020;122:1–11.
Korevaar E, Karahalios A, Turner SL, et al. Methodological systematic review recommends improvements to conduct and reporting when meta-analyzing interrupted time series studies. J Clin Epidemiol. 2022;145:55–69.
Hudson J, Fielding S, Ramsay CR. Methodology and reporting characteristics of studies using interrupted time series design in healthcare. BMC Med Res Methodol. 2019;19(1):1–7.
Leonard SA, Panelli DM. Quasi-experimental study designs can inform pandemic effects on nutrition and weight gain in pregnancy. Am J Clin Nutr. 2023;117(2):216–7.
Lopes S, Soares P, Santos Sousa J, Rocha JV, Boto P, Santana R. Effect of the COVID-19 pandemic on the frequency of emergency department visits in Portugal: an interrupted time series analysis until July 2021. JACEP Open. 2023;4(1):e12864.
Domingues M, Torre C, Guerreiro JP, et al. COVID-19 pandemic and the quality of antibiotic use in primary care: an interrupted time-series study. Int J Qual Health Care. 2023;35(2):mzad014.
Almeida D, Rodrigues AT, Guerreiro JP, et al. COVID-19 pandemic and the consumption of self-care products for pediculosis capitis in Portugal: an interrupted time-series analysis. Parasitol Res. 2024;123(6):235.
Hanquet G, Valenciano M, Simondon F, Moren A. Vaccine effects and impact of vaccination programmes in post-licensure studies. Vaccine. 2013;31(48):5634–42.
Su SY. Nationwide mammographic screening and breast cancer mortality in Taiwan: an interrupted time-series analysis. Breast Cancer. 2022;29(2):336–42.