Roberts, A. G., Younge, N. & Greenberg, R. G. Neonatal Necrotizing Enterocolitis: An Update on Pathophysiology, Treatment, and Prevention. Paediatr. Drugs 26, 259–275 (2024).
Alsaied, A., Islam, N. & Thalib, L. Global incidence of Necrotizing Enterocolitis: a systematic review and Meta-analysis. BMC Pediatr. 20, 344 (2020).
Meister, A. L., Doheny, K. K. & Travagli, R. A. Necrotizing enterocolitis: It’s not all in the gut. Exp. Biol. Med (Maywood) 245, 85–95 (2020).
Stey, A. et al. Outcomes and costs of surgical treatments of necrotizing enterocolitis. Pediatrics 135, e1190–e1197 (2015).
Mara, M. A., Good, M. & Weitkamp, J. H. Innate and adaptive immunity in necrotizing enterocolitis. Semin Fetal Neonatal Med 23, 394–399 (2018).
Duess, J. W. et al. Necrotizing enterocolitis, gut microbes, and sepsis. Gut Microbes 15, 2221470 (2023).
Krautkramer, K. A., Fan, J. & Bäckhed, F. Gut microbial metabolites as multi-kingdom intermediates. Nat. Rev. Microbiol 19, 77–94 (2021).
Chen, Z. et al. Bacteroides fragilis alleviates necrotizing enterocolitis through restoring bile acid metabolism balance using bile salt hydrolase and inhibiting FXR-NLRP3 signaling pathway. Gut Microbes 16, 2379566 (2024).
Pan, L. L. et al. Infant feces-derived Lactobacillus gasseri FWJL-4 mitigates experimental necrotizing enterocolitis via acetate production. Gut Microbes 16, 2430541 (2024).
Omenetti, S. & Pizarro, T. T. The Treg/Th17 Axis: A Dynamic Balance Regulated by the Gut Microbiome. Front Immunol. 6, 639 (2015).
Chang, Y. et al. Phytochemicals as regulators of Th17/Treg balance in inflammatory bowel diseases. Biomed. Pharmacother. 141, 111931 (2021).
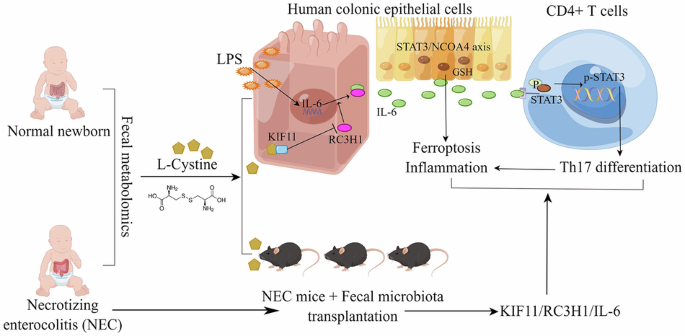
Ma, F. et al. Melatonin ameliorates necrotizing enterocolitis by preventing Th17/Treg imbalance through activation of the AMPK/SIRT1 pathway. Theranostics 10, 7730–7746 (2020).
Yarci, E. et al. Inhibition of Interleukin-6 signaling: A novel therapeutic approach to necrotizing enterocolitis. Int Immunopharmacol. 101, 108358 (2021).
Ma, Z. et al. Fecal microbiota transplantation improves chicken growth performance by balancing jejunal Th17/Treg cells. Microbiome 11, 137 (2023).
Dang, D. et al. Integrative analysis links ferroptosis to necrotizing enterocolitis and reveals the role of ACSL4 in immune disorders. iScience 25, 105406 (2022).
Ho, T., Sarkar, A., Szalacha, L. & Groer, M. W. Intestinal Microbiome in Preterm Infants Influenced by Enteral Iron Dosing. J. Pediatr. Gastroenterol. Nutr. 72, e132–e138 (2021).
Zhang, X., Ma, Y., Lv, G. & Wang, H. Ferroptosis as a therapeutic target for inflammation-related intestinal diseases. Front Pharm. 14, 1095366 (2023).
Gao, C. et al. N-Acetylcysteine Alleviates Necrotizing Enterocolitis by Depressing SESN2 Expression to Inhibit Ferroptosis in Intestinal Epithelial Cells. Inflammation 48, 464–482 (2025).
Dang, D. et al. Heme induces intestinal epithelial cell ferroptosis via mitochondrial dysfunction in transfusion-associated necrotizing enterocolitis. Faseb J. 36, e22649 (2022).
Zhang, Z. et al. Elabela alleviates ferroptosis, myocardial remodeling, fibrosis and heart dysfunction in hypertensive mice by modulating the IL-6/STAT3/GPX4 signaling. Free Radic. Biol. Med 181, 130–142 (2022).
Zhang, H. et al. Quercetin alleviates LPS/iE-DAP-induced liver injury by suppressing ferroptosis via regulating ferritinophagy and intracellular iron efflux. Redox Biol. 81, 103557 (2025).
Chen, H. et al. Butyrate ameliorated ferroptosis in ulcerative colitis through modulating Nrf2/GPX4 signal pathway and improving intestinal barrier. Biochim Biophys. Acta Mol. Basis Dis. 1870, 166984 (2024).
Zheng, Z. J. et al. Sleep Deprivation Induces Gut Damage via Ferroptosis. J. Pineal Res 76, e12987 (2024).
Wei, X. & Feng, X. DS0384 Alleviates Necrotizing Enterocolitis: Secretes N-carbamyl glutamic Acid and Participates in Lipid Metabolism and Lipid Peroxidation Processes. J. Microbiol Biotechnol. 35, e2410040 (2025).
Xiao, S. et al. Vitamin A and Retinoic Acid Exhibit Protective Effects on Necrotizing Enterocolitis by Regulating Intestinal Flora and Enhancing the Intestinal Epithelial Barrier. Arch. Med Res 49, 1–9 (2018).
Horas, H. N. S. et al. Adrenic acid as an inflammation enhancer in non-alcoholic fatty liver disease. Arch. Biochem Biophys. 623-624, 64–75 (2017).
Zhao, J. et al. Adrenic acid induces oxidative stress in hepatocytes. Biochem Biophys. Res Commun. 532, 620–625 (2020).
Chen, X., Li, J., Kang, R., Klionsky, D. J. & Tang, D. Ferroptosis: machinery and regulation. Autophagy 17, 2054–2081 (2021).
Tao, W. et al. Advances in molecular mechanisms and therapeutic strategies for central nervous system diseases based on gut microbiota imbalance. J. Adv. Res 69, 261–278 (2025).
Aziz, M., Prince, J. M. & Wang, P. Gut microbiome and necrotizing enterocolitis: Understanding the connection to find a cure. Cell Host Microbe 30, 612–616 (2022).
Zhang, X., Han, Y., Huang, W., Jin, M. & Gao, Z. The influence of the gut microbiota on the bioavailability of oral drugs. Acta Pharm. Sin. B 11, 1789–1812 (2021).
Tian, B. et al. Epigenetic Insights Into Necrotizing Enterocolitis: Unraveling Methylation-Regulated Biomarkers. Inflammation 48, 236–253 (2025).
Liu, J. et al. Fecal microbiota transplantation by enema reduces intestinal injury in experimental necrotizing enterocolitis. J. Pediatr. Surg. 55, 1094–1098 (2020).
Liu, X. C. et al. Gut microbiota and short-chain fatty acids may be new biomarkers for predicting neonatal necrotizing enterocolitis: A pilot study. Front Microbiol 13, 969656 (2022).
Clemente Plaza, N., Reig García-Galbis, M. & Martínez-Espinosa, R. M. Effects of the Usage of l-Cysteine (l-Cys) on Human Health. Molecules 23, https://doi.org/10.3390/molecules23030575 (2018).
He, Y. et al. SP2509 functions as a novel ferroptosis inhibitor by reducing intracellular iron level in vascular smooth muscle cells. Free Radic. Biol. Med 219, 49–63 (2024).
Xi, C. et al. Simvastatin-Mediated Nrf2 Activation Induces Fetal Hemoglobin and Antioxidant Enzyme Expression to Ameliorate the Phenotype of Sickle Cell Disease. Antioxidants (Basel) 13, https://doi.org/10.3390/antiox13030337 (2024).
Okamoto, H. et al. Perioperative Administration of Cystine and Theanine Suppresses Inflammation and Facilitates Early Rehabilitation and Recovery after Esophagectomy: A Randomized, Double-Blind, Controlled Clinical Trial. Nutrients 14, https://doi.org/10.3390/nu14112319 (2022).
Hasegawa, T., Mizugaki, A., Inoue, Y., Kato, H. & Murakami, H. Cystine reduces tight junction permeability and intestinal inflammation induced by oxidative stress in Caco-2 cells. Amino Acids 53, 1021–1032 (2021).
Zaccherini, G. et al. Assessing the role of amino acids in systemic inflammation and organ failure in patients with ACLF. J. Hepatol. 74, 1117–1131 (2021).
Long, D., Mao, C., Huang, Y., Xu, Y. & Zhu, Y. Ferroptosis in ulcerative colitis: Potential mechanisms and promising therapeutic targets. Biomed. Pharmacother. 175, 116722 (2024).
Chen, Y. et al. Human breast milk-derived phospholipid DOPE ameliorates intestinal injury associated with NEC by inhibiting ferroptosis. Food Funct. 15, 10811–10822 (2024).
Egan, C. E. et al. Toll-like receptor 4-mediated lymphocyte influx induces neonatal necrotizing enterocolitis. J. Clin. Invest 126, 495–508 (2016).
Zhu, C. et al. Roseburia intestinalis inhibits interleukin‑17 excretion and promotes regulatory T cells differentiation in colitis. Mol. Med Rep. 17, 7567-7574 https://doi.org/10.3892/mmr.2018.8833 (2018).
Guo, Y. et al. Biological characteristics of IL-6 and related intestinal diseases. Int J. Biol. Sci. 17, 204–219 (2021).
Ma, F. et al. Interleukin-6-mediated CCR9(+) interleukin-17-producing regulatory T cells polarization increases the severity of necrotizing enterocolitis. EBioMedicine 44, 71–85 (2019).
Tanaka, K. A., Kurihara, S., Shibakusa, T., Chiba, Y. & Mikami, T. Cystine improves survival rates in a LPS-induced sepsis mouse model. Clin. Nutr. 34, 1159–1165 (2015).
Schaefer, J. S. & Klein, J. R. Roquin-a multifunctional regulator of immune homeostasis. Genes Immun. 17, 79–84 (2016).
Wang, J. et al. Deciphering the role of the MALT1-RC3H1 axis in regulating GPX4 protein stability. Proc. Natl. Acad. Sci. USA 122, e2419625121 (2025).
Wu, Y. K., Liu, C. D., Liu, C., Wu, J. & Xie, Z. G. Machine learning and weighted gene co-expression network analysis identify a three-gene signature to diagnose rheumatoid arthritis. Front Immunol. 15, 1387311 (2024).
Hunter, C. E. et al. Hydrogen Sulfide Improves Outcomes in a Murine Model of Necrotizing Enterocolitis via the Cys440 Residue on Endothelial Nitric Oxide Synthase. J. Pediatr. Surg. 58, 2391–2398 (2023).
Drucker, N. A., Jensen, A. R., Ferkowicz, M. & Markel, T. A. Hydrogen sulfide provides intestinal protection during a murine model of experimental necrotizing enterocolitis. J. Pediatr. Surg. 53, 1692–1698 (2018).
Pickard, J. M. et al. Rapid fucosylation of intestinal epithelium sustains host-commensal symbiosis in sickness. Nature 514, 638–641 (2014).
Tran, L. et al. Necrotizing enterocolitis and cytomegalovirus infection in a premature infant. Pediatrics 131, e318–e322 (2013).
Prado, C. et al. The protective effects of fecal microbiota transplantation in an experimental model of necrotizing enterocolitis. J. Pediatr. Surg. 54, 1578–1583 (2019).
Goto, Y. et al. Innate lymphoid cells regulate intestinal epithelial cell glycosylation. Science 345, 1254009 (2014).
Bauché, D. et al. IL-23 and IL-2 activation of STAT5 is required for optimal IL-22 production in ILC3s during colitis. Sci Immunol 5, https://doi.org/10.1126/sciimmunol.aav1080 (2020).
Seo, G. Y. et al. LIGHT-HVEM Signaling in Innate Lymphoid Cell Subsets Protects Against Enteric Bacterial Infection. Cell Host Microbe 24, 249–260.e244 (2018).
Kurihara, S., Shibahara, S., Arisaka, H. & Akiyama, Y. Enhancement of antigen-specific immunoglobulin G production in mice by co-administration of L-cystine and L-theanine. J. Vet. Med Sci. 69, 1263–1270 (2007).
Lin, L. et al. The STAT3 inhibitor NSC 74859 is effective in hepatocellular cancers with disrupted TGF-beta signaling. Oncogene 28, 961–972 (2009).
Bian, Y. et al. Protective Effect of Kaempferol on LPS-Induced Inflammation and Barrier Dysfunction in a Coculture Model of Intestinal Epithelial Cells and Intestinal Microvascular Endothelial Cells. J. Agric Food Chem. 68, 160–167 (2020).
Dai, W. & Chen, Q. M. Fresh Medium or L-Cystine as an Effective Nrf2 Inducer for Cytoprotection in Cell Culture. Cells 12, https://doi.org/10.3390/cells12020291 (2023).
Zhang, Y., Du, W., Chen, Z. & Xiang, C. Upregulation of PD-L1 by SPP1 mediates macrophage polarization and facilitates immune escape in lung adenocarcinoma. Exp. Cell Res 359, 449–457 (2017).
Wei, Y. Y. et al. Interleukin-6 neutralizing antibody attenuates the hypersecretion of airway mucus via inducing the nuclear translocation of Nrf2 in chronic obstructive pulmonary disease. Biomed. Pharmacother. 152, 113244 (2022).
Nishiwaki, N. et al. Overcoming cancer-associated fibroblast-induced immunosuppression by anti-interleukin-6 receptor antibody. Cancer Immunol. Immunother. 72, 2029–2044 (2023).
Betts, B. C. et al. CD4+ T cell STAT3 phosphorylation precedes acute GVHD, and subsequent Th17 tissue invasion correlates with GVHD severity and therapeutic response. J. Leukoc. Biol. 97, 807–819 (2015).
Zhang, X. et al. β-glucan protects against necrotizing enterocolitis in mice by inhibiting intestinal inflammation, improving the gut barrier, and modulating gut microbiota. J. Transl. Med 21, 14 (2023).
Qiu, L. et al. Morin alleviates DSS-induced ulcerative colitis in mice via inhibition of inflammation and modulation of intestinal microbiota. Int Immunopharmacol. 140, 112846 (2024).