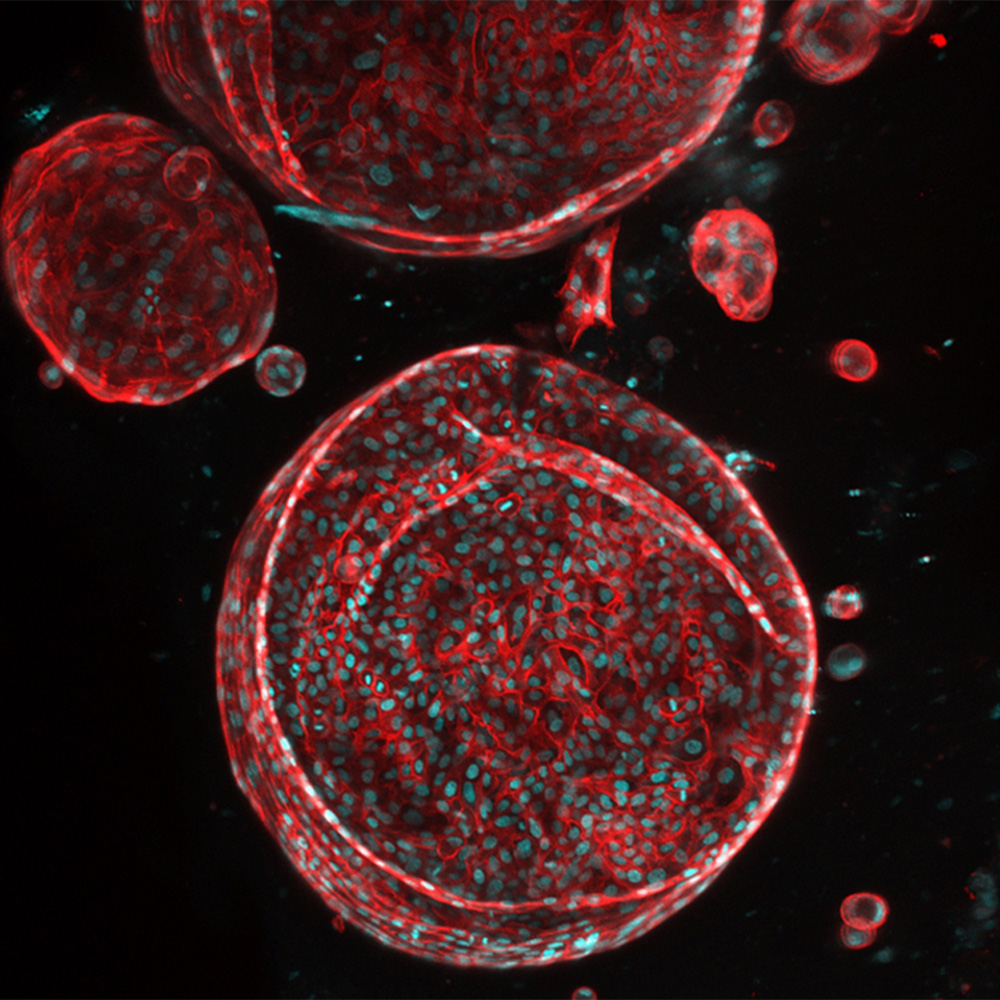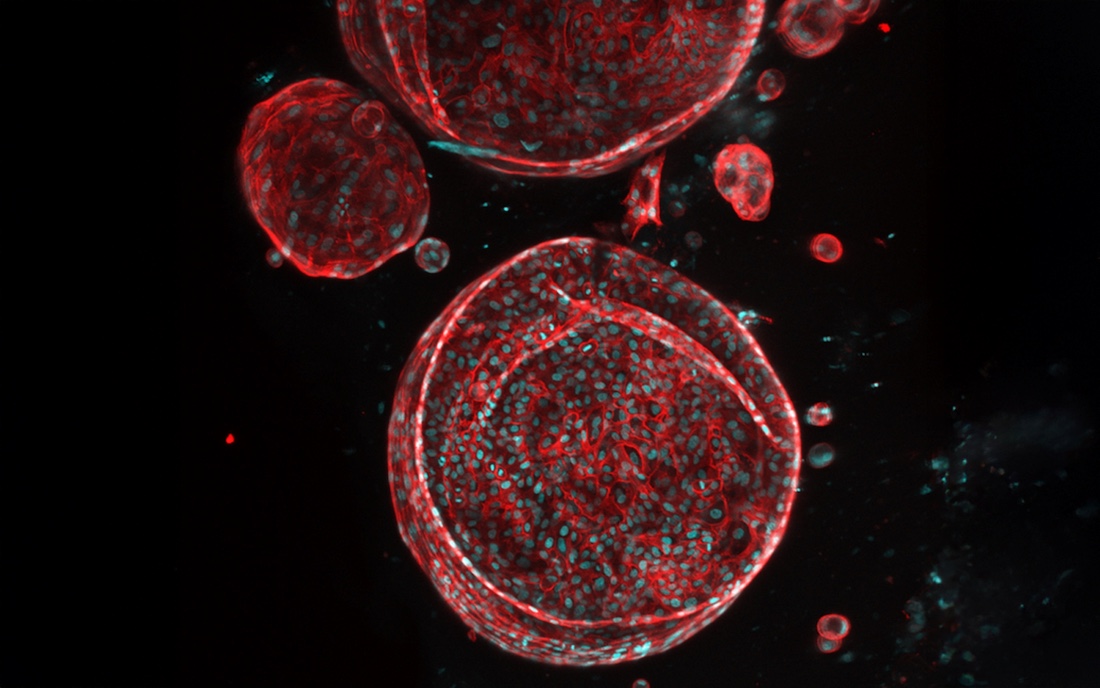
Patient biopsy-derived liver organoids can serve as building blocks for biofabrication of a personalized, patient-specific whole liver. This image shows liver organoids generated from a patient liver biopsy with alcoholic liver disease. CD44 is shown in red marking liver organoids, and cell nuclei are shown in blue. (Photo credit: Sunil Shrestha, Ph.D., postdoctoral fellow, Rizwan Lab)
DALLAS – Jan. 12, 2026 – UT Southwestern Medical Center has received an award from the Advanced Research Projects Agency for Health (ARPA-H) to develop livers using patients’ own cells and an innovative three-dimensional (3D) printing approach. If successful, this project – known as Vascularized Immunocompetent Tissue as an Alternative Liver (VITAL) – could significantly reduce the gap between supply and demand for donor livers, negate the necessity of lifelong immunosuppression for liver transplant patients, and create artificial livers for in vitro drug testing and research. The project is under ARPA-H’s Personalized Regenerative Immunocompetent Nanotechnology Tissue (PRINT) program, which is led by ARPA-H Program Manager Ryan Spitler, Ph.D.

Muhammad Rizwan, Ph.D., Assistant Professor of Biomedical Engineering and Ophthalmology at UT Southwestern, is the project’s principal investigator.
“Over the last two decades, researchers have made remarkable progress toward the goal of creating lab-made organs, including innovations in biomaterials, stem cell differentiation, and bioprinting. UT Southwestern is an ideal environment to bring together the recent advances that have never been combined before,” said the project’s principal investigator, Muhammad Rizwan, Ph.D., Assistant Professor of Biomedical Engineering and Ophthalmology at UT Southwestern.
Each year, liver cirrhosis and chronic liver diseases cause about 50,000 deaths in the U.S. As of September 2024, nearly 10,000 people were on the waiting list for a donor liver, with wait times averaging about seven months, according to the Health Resources & Services Administration. Statistics show that up to 31% of patients die while waiting for a donor liver.
Researchers have attempted to narrow the gap between donor liver supply and demand in many ways, such as pursuing living donors or improving technology that keeps cadaver donor livers healthy for a longer time before transplant, said Madhukar Patel, M.D., M.B.A., Sc.M., Assistant Professor of Surgery at UTSW, Surgical Director of the Liver Transplantation Program, and a Dedman Family Scholar in Clinical Care. However, none of these approaches has significantly resolved the lack of sufficient donor livers. Finding a way to generate artificial livers that function as well as natural ones could offer a solution, he explained. Artificial livers may also address other issues inherent to organ transplants, such as the need for lifelong immunosuppression and the high cost of liver transplantation, which averages nearly $1 million.
Madhukar Patel, M.D., M.B.A., Sc.M., is Assistant Professor of Surgery at UT Southwestern, Surgical Director of the Liver Transplantation Program, and a Dedman Family Scholar in Clinical Care.
Toward that goal, ARPA-H recently awarded UTSW up to $25 million for VITAL. In this project, researchers across UTSW, including Drs. Rizwan and Patel, will work together to harvest cells from liver disease patients and facilitate their conversion into induced pluripotent stem cells (iPSCs), which can become any cell type in the body. Jun Wu, Ph.D., Associate Professor of Molecular Biology, whose lab specializes in working with iPSCs, will lead research to reprogram the patient cells into iPSCs and convert these cells into the various cell types that make up livers. The team will then combine these cells with a hydrogel “bioink” that can be used for 3D printing of functioning livers. These bioprinted livers will first be tested in small and large animal models and potentially within humans in about five years, Dr. Rizwan said. Collaborators from Pennsylvania State University, led by Ibrahim T. Ozbolat, and the University of California, Davis, will assist with improving the 3D printing technology and GMP cell manufacturing.
Researchers at UTSW and elsewhere have successfully created liver tissue by converting iPSCs to liver cells. However, Dr. Rizwan said, a major roadblock to scaling this tissue into an artificial liver is the lack of blood vessels and bile ducts, tubes that remove bile acids that build up from normal liver function. He and his colleagues have discovered a novel approach for growing both blood vessels and bile ducts within generated liver tissue, making it possible to create a fully functional artificial liver. Moreover, Dr. Rizwan is establishing a scalable organoid manufacturing facility at UT Southwestern.
Because the resulting organ will be custom-made from a patient’s own cells, he added, transplanted livers won’t require immunosuppression. In addition, he estimates a bioprinted liver could be generated in 10-13 weeks. These artificial organs won’t just be useful for transplantation, Dr. Rizwan explained. The process of developing livers from scratch is expected to lend insight into how natural livers function, helping researchers solve long-standing mysteries about this organ. Artificial livers will also be used to evaluate the safety and efficacy of pharmaceuticals in development.

Samuel Achilefu, Ph.D., is inaugural Chair of Biomedical Engineering and Professor in the Harold C. Simmons Comprehensive Cancer Center and of Radiology at UT Southwestern and a co-investigator on this project.
The wealth of expertise and collaboration available at UTSW makes it an ideal location for developing artificial livers, said Samuel Achilefu, Ph.D., inaugural Chair of Biomedical Engineering and Professor in the Harold C. Simmons Comprehensive Cancer Center and of Radiology at UTSW. A co-investigator on this project, he will use his expertise in noninvasive imaging to evaluate the performance of the bioprinted livers.
UTSW has a robust solid organ transplant program that recently celebrated its 1,000th liver transplant and houses experts across the spectrum needed for developing artificial livers. In addition, the seven UTSW researchers leading portions of this project, the 11 core facilities they will use, and UTSW’s hepatology clinics are all within walking distance, facilitating teamwork.
“This project represents a bold step toward advancing patient care through biomedical innovation,” Dr. Achilefu said. “It unites engineers, clinicians, and scientists to transform discovery into real-world solutions, shaping a future where functional organ printing becomes reality.”
Other UTSW co-investigators involved in the project are Hao Zhu, M.D., Professor of Children’s Medical Center Research Institute at UT Southwestern; Walter Akers, Ph.D., D.V.M., Associate Professor of Biomedical Engineering; and Yasin Dhaher, Ph.D., Professor of Physical Medicine & Rehabilitation.
Dr. Wu is a Virginia Murchison Linthicum Scholar in Medical Research. Dr. Achilefu holds the Lyda Hill Distinguished University Chair in Biomedical Engineering. Dr. Zhu holds the Nancy B. and Jake L. Hamon Distinguished Chair in Therapeutic Oncology Research. Drs. Achilefu, Akers, Rizwan, Wu, and Zhu are members of the Simmons Cancer Center.
This publication was supported by the Advanced Research Projects Agency for Health (ARPA-H) under Award Number D25AC000239-00, providing up to $24,939,120 for a 60-month period. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Advanced Research Projects Agency for Health.
About UT Southwestern Medical Center
UT Southwestern, one of the nation’s premier academic medical centers, integrates pioneering biomedical research with exceptional clinical care and education. The institution’s faculty members have received six Nobel Prizes and include 24 members of the National Academy of Sciences, 25 members of the National Academy of Medicine, and 13 Howard Hughes Medical Institute Investigators. The full-time faculty of more than 3,200 is responsible for groundbreaking medical advances and is committed to translating science-driven research quickly to new clinical treatments. UT Southwestern physicians provide care in more than 80 specialties to more than 140,000 hospitalized patients, more than 360,000 emergency room cases, and oversee nearly 5.1 million outpatient visits a year.
Related Stories