Yin X, Xie Q, Huang L, Liu L, Armstrong E, Zhen M, et al. Assessment of the psychological burden among family caregivers of people living with alzheimer’s disease using the Zarit burden interview. J Alzheimers Dis. 2021;82(1):285–91. https://doi.org/10.3233/JAD-210025.
Wang X, Huang W, Su L, Xing Y, Jessen F, Sun Y, et al. Neuroimaging advances regarding subjective cognitive decline in preclinical alzheimer’s disease. Mol Neurodegeneration. 2020;15(1):55. https://doi.org/10.1186/s13024-020-00395-3.
Rabin LA, Smart CM, Amariglio RE. Subjective cognitive decline in preclinical alzheimer’s disease. Ann Rev Clin Psychol. 2017;13:369–96. https://doi.org/10.1146/annurev-clinpsy-032816-045136.
Liew TM. Trajectories of subjective cognitive decline, and the risk of mild cognitive impairment and dementia. Alzheimers Res Ther. 2020;12(1):135. https://doi.org/10.1186/s13195-020-00699-y.
Rosenberg PB, Lyketsos C. Mild cognitive impairment: searching for the prodrome of alzheimer’s disease. World Psychiatry: Official J World Psychiatric Association (WPA). 2008;7(2):72–8. https://doi.org/10.1002/j.2051-5545.2008.tb00159.x.
Sperling RA, Donohue MC, Raman R, Sun CK, Yaari R, Holdridge K, et al. Association of factors with elevated amyloid burden in clinically normal older individuals. JAMA Neurol. 2020;77(6):735. https://doi.org/10.1001/jamaneurol.2020.0387.
Si T, Xing G, Han Y. Subjective cognitive decline and related cognitive deficits. Front Neurol. 2020;11:247. https://doi.org/10.3389/fneur.2020.00247.
Sheng C, Yang K, Wang X, Li H, Li T, Lin L, et al. Advances in Non-Pharmacological interventions for subjective cognitive decline: A systematic review and Meta-Analysis. J Alzheimers Dis. 2020;77(2):903–20. https://doi.org/10.3233/jad-191295.
Tromp D, Dufour A, Lithfous S, Pebayle T, Després O. Episodic memory in normal aging and alzheimer disease: insights from imaging and behavioral studies. Ageing Res Rev. 2015;24(Pt B):232–62. https://doi.org/10.1016/j.arr.2015.08.006.
Xue G. The neural representations underlying human episodic memory. Trends Cogn Sci. 2018;22(6):544–61. https://doi.org/10.1016/j.tics.2018.03.004.
Yu Q, Cheval B, Becker B, Herold F, Chan CCH, Delevoye-Turrell YN, et al. Episodic memory encoding and retrieval in Face-Name paired paradigm: an fNIRS study. Brain Sci. 2021;11(7). https://doi.org/10.3390/brainsci11070951.
Torres-Morales C, Cansino S. Brain representations of space and time in episodic memory: A systematic review and meta-analysis. Cogn Affect Behav Neurosci. 2024;24(1):1–18. https://doi.org/10.3758/s13415-023-01140-1.
Ergis AM, Eusop-Roussel E. [Early episodic memory impairments in alzheimer’s disease]. Rev Neurol. 2008;164(Suppl 3):S96–s. https://doi.org/10.1016/s0035-3787(08)73298-3.
Takehara-Nishiuchi K. Prefrontal-hippocampal interaction during the encoding of new memories. Brain Neurosci Adv. 2020;4:2398212820925580. https://doi.org/10.1177/2398212820925580.
Zhu Y, Zang F, Wang Q, Zhang Q, Tan C, Zhang S, et al. Connectome-based model predicts episodic memory performance in individuals with subjective cognitive decline and amnestic mild cognitive impairment. Behav Brain Res. 2021;411:113387. https://doi.org/10.1016/j.bbr.2021.113387.
Vidal-Piñeiro D, Martin-Trias P, Arenaza-Urquijo EM, Sala-Llonch R, Clemente IC, Mena-Sánchez I, et al. Task-dependent activity and connectivity predict episodic memory network-based responses to brain stimulation in healthy aging. Brain Stimul. 2014;7(2):287–96. https://doi.org/10.1016/j.brs.2013.12.016.
Wichmann C, Kuner T. Heterogeneity of glutamatergic synapses: cellular mechanisms and network consequences. Physiol Rev. 2022;102(1):269–318. https://doi.org/10.1152/physrev.00039.2020.
Shankar GM, Li S, Mehta TH, Garcia-Munoz A, Shepardson NE, Smith I, et al. Amyloid-beta protein dimers isolated directly from alzheimer’s brains impair synaptic plasticity and memory. Nat Med. 2008;14(8):837–42. https://doi.org/10.1038/nm1782.
Walsh DM, Selkoe DJ. Deciphering the molecular basis of memory failure in alzheimer’s disease. Neuron. 2004;44(1):181–93. https://doi.org/10.1016/j.neuron.2004.09.010.
Motta C, Di Lorenzo F, Ponzo V, Pellicciari MC, Bonnì S, Picazio S, et al. Transcranial magnetic stimulation predicts cognitive decline in patients with alzheimer’s disease. J Neurol Neurosurg Psychiatry. 2018;89(12):1237–42. https://doi.org/10.1136/jnnp-2017-317879.
Di Lorenzo F, Motta C, Casula EP, Bonnì S, Assogna M, Caltagirone C, et al. LTP-like cortical plasticity predicts conversion to dementia in patients with memory impairment. Brain Stimul. 2020;13(5):1175–82. https://doi.org/10.1016/j.brs.2020.05.013.
Di Lazzaro V, Bella R, Benussi A, Bologna M, Borroni B, Capone F, et al. Diagnostic contribution and therapeutic perspectives of transcranial magnetic stimulation in dementia. Clin Neurophysiology: Official J Int Federation Clin Neurophysiol. 2021;132(10):2568–607. https://doi.org/10.1016/j.clinph.2021.05.035.
Tian Y, Margulies DS, Breakspear M, Zalesky A. Topographic organization of the human subcortex unveiled with functional connectivity gradients. Nat Neurosci. 2020;23(11):1421–32. https://doi.org/10.1038/s41593-020-00711-6.
Di Lorenzo F, Ponzo V, Bonnì S, Motta C, Negrão Serra PC, Bozzali M, et al. Long-term potentiation-like cortical plasticity is disrupted in alzheimer’s disease patients independently from age of onset. Ann Neurol. 2016;80(2):202–10. https://doi.org/10.1002/ana.24695.
Lefaucheur JP, Aleman A, Baeken C, Benninger DH, Brunelin J, Di Lazzaro V, et al. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS): an update (2014–2018). Clin Neurophysiology: Official J Int Federation Clin Neurophysiol. 2020;131(2):474–528. https://doi.org/10.1016/j.clinph.2019.11.002.
Suppa A, Li Voti P, Rocchi L, Papazachariadis O, Berardelli A. Early visuomotor integration processes induce LTP/LTD-like plasticity in the human motor cortex. Cerebral cortex (New York, NY: 1991). 2015;25(3):703-12. https://doi.org/10.1093/cercor/bht264.
Cirillo G, Di Pino G, Capone F, Ranieri F, Florio L, Todisco V, et al. Neurobiological after-effects of non-invasive brain stimulation. Brain Stimul. 2017;10(1):1–18. https://doi.org/10.1016/j.brs.2016.11.009.
Solé-Padullés C, Bartrés-Faz D, Junqué C, Clemente IC, Molinuevo JL, Bargalló N et al. Repetitive transcranial magnetic stimulation effects on brain function and cognition among elders with memory dysfunction. A randomized sham-controlled study. Cerebral cortex (New York, NY: 1991). 2006;16(10):1487-93. https://doi.org/10.1093/cercor/bhj083.
Liu M, Nie ZY, Li RR, Zhang W, Huang LH, Wang JQ, et al. Neural mechanism of repeated transcranial magnetic stimulation to enhance visual working memory in elderly individuals with subjective cognitive decline. Front Neurol. 2021;12:665218. https://doi.org/10.3389/fneur.2021.665218.
Liang X, Xue C, Zheng D, Yuan Q, Qi W, Ruan Y, et al. Repetitive transcranial magnetic stimulation regulates effective connectivity patterns of brain networks in the spectrum of preclinical alzheimer’s disease. Front Aging Neurosci. 2024;16:1343926. https://doi.org/10.3389/fnagi.2024.1343926.
Lin Y, Jiang WJ, Shan PY, Lu M, Wang T, Li RH, et al. The role of repetitive transcranial magnetic stimulation (rTMS) in the treatment of cognitive impairment in patients with alzheimer’s disease: A systematic review and meta-analysis. J Neurol Sci. 2019;398:184–91. https://doi.org/10.1016/j.jns.2019.01.038.
Zhang T, Sui Y, Lu Q, Xu X, Zhu Y, Dai W, et al. Effects of rTMS treatment on global cognitive function in alzheimer’s disease: A systematic review and meta-analysis. Front Aging Neurosci. 2022;14:984708. https://doi.org/10.3389/fnagi.2022.984708.
Hauer L, Sellner J, Brigo F, Trinka E, Sebastianelli L, Saltuari L, et al. Effects of repetitive transcranial magnetic stimulation over prefrontal cortex on attention in psychiatric disorders: A systematic review. J Clin Med. 2019;8(4). https://doi.org/10.3390/jcm8040416.
Balconi M. Dorsolateral prefrontal cortex, working memory and episodic memory processes: insight through transcranial magnetic stimulation techniques. Neurosci Bull. 2013;29(3):381–9. https://doi.org/10.1007/s12264-013-1309-z.
Li Y, Wang L, Jia M, Guo J, Wang H, Wang M. The effects of high-frequency rTMS over the left DLPFC on cognitive control in young healthy participants. PLoS ONE. 2017;12(6):e0179430. https://doi.org/10.1371/journal.pone.0179430.
Davis SW, Luber B, Murphy DLK, Lisanby SH, Cabeza R. Frequency-specific neuromodulation of local and distant connectivity in aging and episodic memory function. Hum Brain Mapp. 2017;38(12):5987–6004. https://doi.org/10.1002/hbm.23803.
Li X, Qi G, Yu C, Lian G, Zheng H, Wu S, et al. Cortical plasticity is correlated with cognitive improvement in alzheimer’s disease patients after rTMS treatment. Brain Stimul. 2021;14(3):503–10. https://doi.org/10.1016/j.brs.2021.01.012.
Wu Q, Xu X, Zhai C, Zhao Z, Dai W, Wang T, et al. High-frequency repetitive transcranial magnetic stimulation improves Spatial episodic learning and memory performance by regulating brain plasticity in healthy rats. Front NeuroSci. 2022;16:974940. https://doi.org/10.3389/fnins.2022.974940.
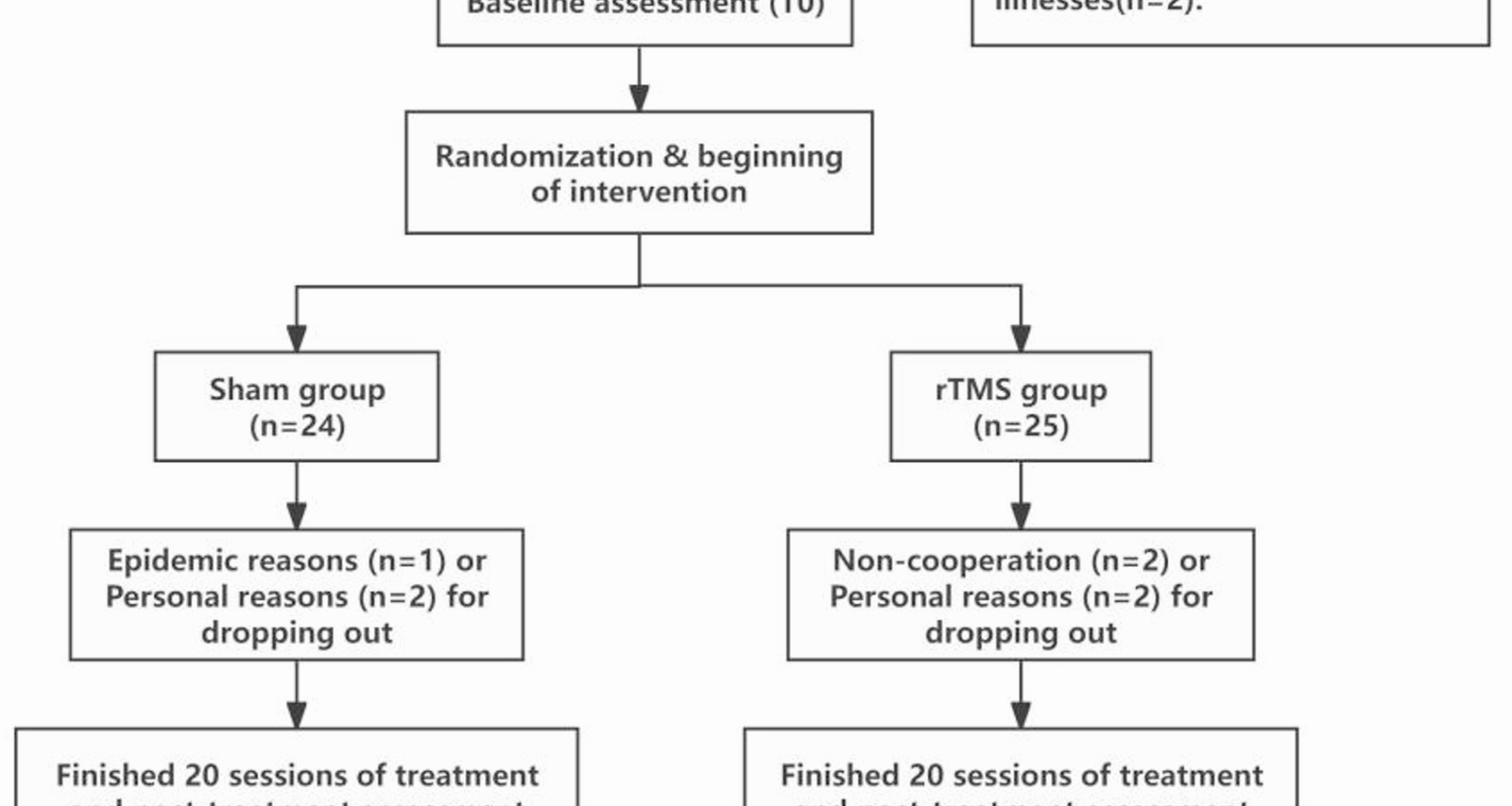
Zhang T, Huang S, Lu Q, Song J, Teng J, Wang T, et al. Effects of repetitive transcranial magnetic stimulation on episodic memory in patients with subjective cognitive decline: study protocol for a randomized clinical trial. Front Psychol. 2023;14:1298065. https://doi.org/10.3389/fpsyg.2023.1298065.
Zhong Q, Ali N, Gao Y, Wu H, Wu X, Sun C, et al. Gait kinematic and kinetic characteristics of older adults with mild cognitive impairment and subjective cognitive decline: A Cross-Sectional study. Front Aging Neurosci. 2021;13:664558. https://doi.org/10.3389/fnagi.2021.664558.
Shen Y, Lu Q, Zhang T, Yan H, Mansouri N, Osipowicz K, et al. Use of machine learning to identify functional connectivity changes in a clinical cohort of patients at risk for dementia. Front Aging Neurosci. 2022;14:962319. https://doi.org/10.3389/fnagi.2022.962319.
Jia Y, Xu L, Yang K, Zhang Y, Lv X, Zhu Z, et al. Precision repetitive transcranial magnetic stimulation over the left parietal cortex improves memory in alzheimer’s disease: A randomized, Double-Blind, Sham-Controlled study. Front Aging Neurosci. 2021;13:693611. https://doi.org/10.3389/fnagi.2021.693611.
Beam W, Borckardt JJ, Reeves ST, George MS. An efficient and accurate new method for locating the F3 position for prefrontal TMS applications. Brain Stimul. 2009;2(1):50–4. https://doi.org/10.1016/j.brs.2008.09.006.
Li Q, MIAO Y, ZHONG Y. Auditory verbal learning test-HuaShan version in the diagnosis of amnestic mild cognitive impairment. Geriatr Health Care. 2016;22(5):282–5.
Z Q, G Y. Application of auditory verbal learning test-Huashan version in patients with subjective cognitive decline and mild cognitive impairment. Chin J Rehabilitation Med. 2024;39(2):191–5.
Yu F, Tang X, Hu R, Liang S, Wang W, Tian S, et al. The After-Effect of accelerated intermittent theta burst stimulation at different session intervals. Front NeuroSci. 2020;14:576. https://doi.org/10.3389/fnins.2020.00576.
Huang YZ, Edwards MJ, Rounis E, Bhatia KP, Rothwell JC. Theta burst stimulation of the human motor cortex. Neuron. 2005;45(2):201. https://doi.org/10.1016/j.neuron.2004.12.033.
Kensara OA, Helal OF, El-Kafy EMA, Ghafouri KJ, Ghaith MM, Alsolami FJ, et al. The combined effect of vitamin D deficiency and hyperparathyroidism on postural stability among healthy adult males. Pakistan J Biol Sciences: PJBS. 2019;22(9):406–11. https://doi.org/10.3923/pjbs.2019.406.411.
Freedberg MV, Reeves JA, Fioriti CM, Murillo J, Wassermann EM. Reproducing the effect of hippocampal network-targeted transcranial magnetic stimulation on episodic memory. Behav Brain Res. 2022;419:113707. https://doi.org/10.1016/j.bbr.2021.113707.
van der Plas M, Braun V, Stauch BJ, Hanslmayr S. Stimulation of the left dorsolateral prefrontal cortex with slow rTMS enhances verbal memory formation. PLoS Biol. 2021;19(9):e3001363. https://doi.org/10.1371/journal.pbio.3001363.
Traikapi A, Kalli I, Kyriakou A, Stylianou E, Symeou RT, Kardama A, et al. Episodic memory effects of gamma frequency precuneus transcranial magnetic stimulation in alzheimer’s disease: A randomized multiple baseline study. J Neuropsychol. 2023;17(2):279–301. https://doi.org/10.1111/jnp.12299.
Hoy KE, Emonson MRL, Bailey NW, Rogers C, Coyle H, Stockman F, et al. Gamma connectivity predicts response to intermittent theta burst stimulation in alzheimer’s disease: a randomized controlled trial. Neurobiol Aging. 2023;132:13–23. https://doi.org/10.1016/j.neurobiolaging.2023.08.006.
Canas PM, Simões AP, Rodrigues RJ, Cunha RA. Predominant loss of glutamatergic terminal markers in a β-amyloid peptide model of Alzheimer’s disease. Neuropharmacol 2014;76 Pt A:51–610.1016/j.neuropharm.2013.08.026
Koch G, Bonnì S, Pellicciari MC, Casula EP, Mancini M, Esposito R, et al. Transcranial magnetic stimulation of the precuneus enhances memory and neural activity in prodromal alzheimer’s disease. NeuroImage. 2018;169:302–11. https://doi.org/10.1016/j.neuroimage.2017.12.048.
Cui X, Ren W, Zheng Z, Li J. Repetitive transcranial magnetic stimulation improved source memory and modulated Recollection-Based retrieval in healthy older adults. Front Psychol. 2020;11:1137. https://doi.org/10.3389/fpsyg.2020.01137.
Zhao Q, Lv Y, Zhou Y, Hong Z, Guo Q. Short-term delayed recall of auditory verbal learning test is equivalent to long-term delayed recall for identifying amnestic mild cognitive impairment. PLoS ONE. 2012;7(12):e51157. https://doi.org/10.1371/journal.pone.0051157.
Ma J, Zheng MX, Wu JJ, Xing XX, Xiang YT, Wei D, et al. Mapping the long-term delayed recall-based cortex-hippocampus network constrained by the structural and functional connectome: a case-control multimodal MRI study. Alzheimers Res Ther. 2023;15(1):61. https://doi.org/10.1186/s13195-023-01197-7.
Jin J, Maren S. Prefrontal-Hippocampal interactions in memory and emotion. Front Syst Neurosci. 2015;9:170. https://doi.org/10.3389/fnsys.2015.00170.
Ye Z, Shi L, Li A, Chen C, Xue G. Retrieval practice facilitates memory updating by enhancing and differentiating medial prefrontal cortex representations. eLife. 2020;9. https://doi.org/10.7554/eLife.57023.
Kluen LM, Dandolo LC, Jocham G, Schwabe L. Dorsolateral Prefrontal Cortex Enables Updating of Established Memories. Cerebral cortex (New York, NY: 1991). 2019;29(10):4154-68. https://doi.org/10.1093/cercor/bhy298
Higo T, Mars RB, Boorman ED, Buch ER, Rushworth MF. Distributed and causal influence of frontal operculum in task control. Proc Natl Acad Sci USA. 2011;108(10):4230–5. https://doi.org/10.1073/pnas.1013361108.
Manenti R, Brambilla M, Petesi M, Ferrari C, Cotelli M. Enhancing verbal episodic memory in older and young subjects after non-invasive brain stimulation. Front Aging Neurosci. 2013;5:49. https://doi.org/10.3389/fnagi.2013.00049.
Manenti R, Sandrini M, Gobbi E, Cobelli C, Brambilla M, Binetti G, et al. Strengthening of existing episodic memories through Non-invasive stimulation of prefrontal cortex in older adults with subjective memory complaints. Front Aging Neurosci. 2017;9:401. https://doi.org/10.3389/fnagi.2017.00401.
Scarmeas N, Stern Y. fMRI evidence of compensatory mechanisms in older adults at genetic risk for alzheimer disease. Neurology. 2005;65(9):1514–5. https://doi.org/10.1212/wnl.65.9.1514-a. author reply – 5.
Gigi A, Babai R, Penker A, Hendler T, Korczyn AD. Prefrontal compensatory mechanism May enable normal semantic memory performance in mild cognitive impairment (MCI). J Neuroimaging: Official J Am Soc Neuroimaging. 2010;20(2):163–8. https://doi.org/10.1111/j.1552-6569.2009.00386.x.
Erk S, Spottke A, Meisen A, Wagner M, Walter H, Jessen F. Evidence of neuronal compensation during episodic memory in subjective memory impairment. Arch Gen Psychiatry. 2011;68(8):845–52. https://doi.org/10.1001/archgenpsychiatry.2011.80.
Haley MS, Maffei A. Versatility and flexibility of cortical circuits. The neuroscientist: a review journal bringing neurobiology. Neurol Psychiatry. 2018;24(5):456–70. https://doi.org/10.1177/1073858417733720.
Mansvelder HD, Verhoog MB, Goriounova NA. Synaptic plasticity in human cortical circuits: cellular mechanisms of learning and memory in the human brain? Current opinion in neurobiology. 2019;54:186–9310.1016/j.conb.2018.06.013
Stampanoni Bassi M, Iezzi E, Gilio L, Centonze D, Buttari F. Synaptic plasticity shapes brain connectivity: implications for network topology. Int J Mol Sci. 2019;20(24). https://doi.org/10.3390/ijms20246193.
Francesco DL, Koch G. Synaptic impairment: the new battlefield of alzheimer’s disease. Alzheimer’s Dement J Alzheimer’s Assoc. 2021;17(2):314. https://doi.org/10.1002/alz.12189.
Buss SS, Press DZ, McDonald K, Kitchener E, O’Connor M, Donohoe K, et al. LTP-like plasticity is impaired in amyloid-positive amnestic MCI but independent of PET-amyloid burden. Neurobiol Aging. 2020;96:109–16. https://doi.org/10.1016/j.neurobiolaging.2020.08.021.
Vossel KA, Ranasinghe KG, Beagle AJ, Mizuiri D, Honma SM, Dowling AF, et al. Incidence and impact of subclinical epileptiform activity in alzheimer’s disease. Ann Neurol. 2016;80(6):858–70. https://doi.org/10.1002/ana.24794.
Styr B, Slutsky I. Imbalance between firing homeostasis and synaptic plasticity drives early-phase alzheimer’s disease. Nat Neurosci. 2018;21(4):463–73. https://doi.org/10.1038/s41593-018-0080-x.