Over the 4-year periods, SGH ED received a total of 28,621 cases of dermatological nature. There was a 15.6% drop in presentation during the COVID-19 period compared to pre-pandemic times (15,523 vs. 13,098 cases).
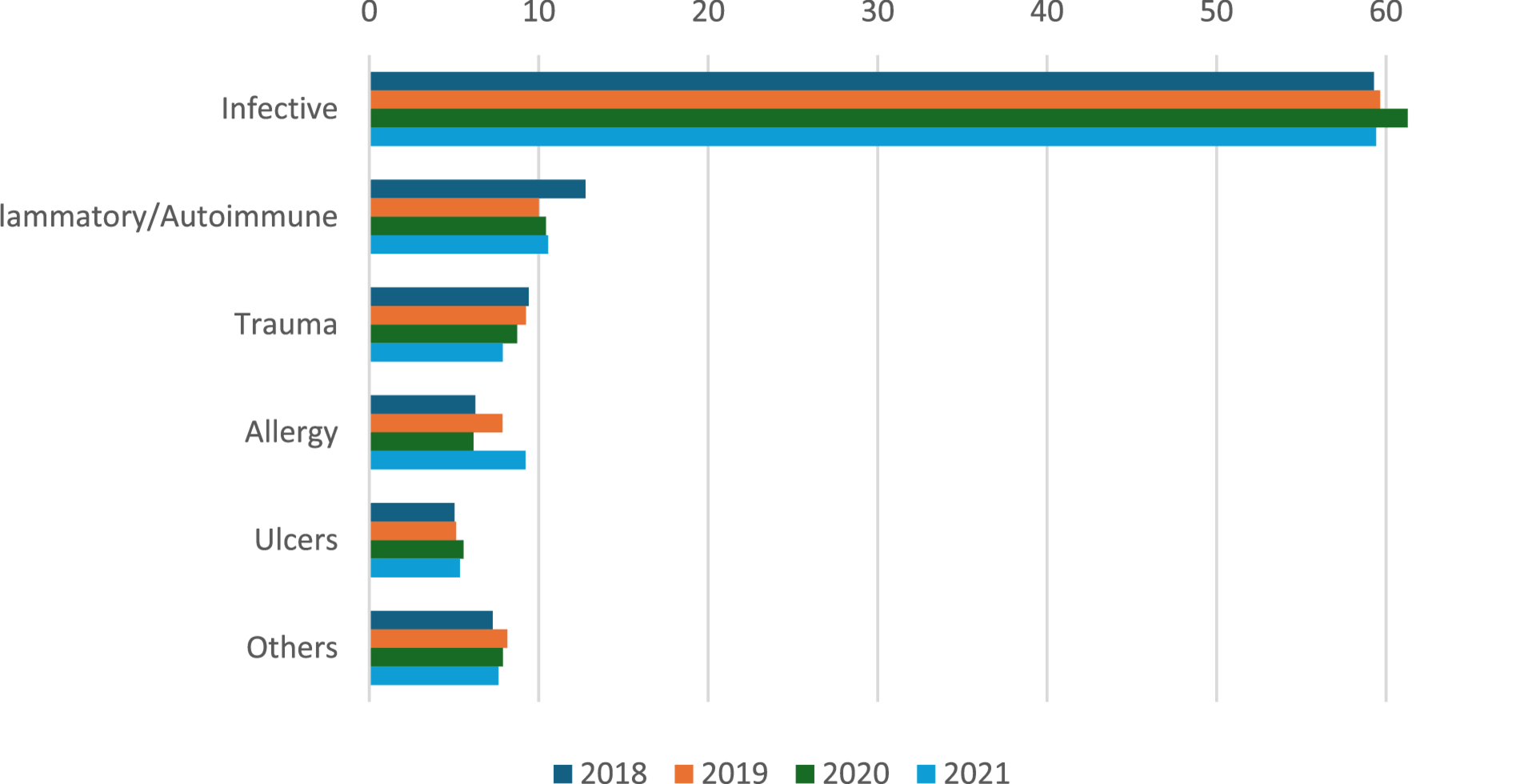
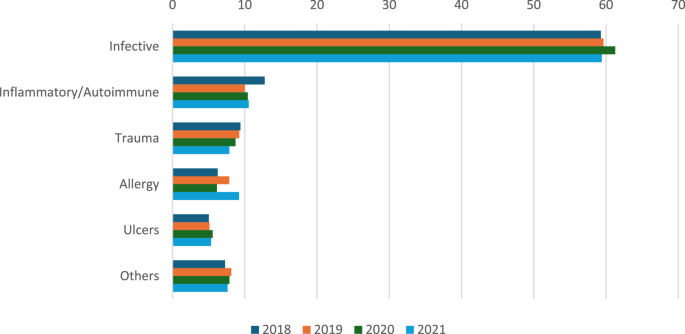
We have grouped the ICD-9 diagnoses into different including infective, inflammatory/autoimmune, trauma (which includes laceration, bites, nail trauma etc.), allergy, ulcers, and others (including cyst, non-immunobullous blisters, cancers etc.). (Fig. 1). A more detailed breakdown year-by-year is provided in Supplementary Table S1.
Trends of diagnostic categories throughout the 4 years 2018 to 2021 in percentage of all dermatological presentations to the SGH ED
Through all 4 years, the was a wide variability of dermatological presentations to the SGH ED. The most encountered condition is infective condition, followed by inflammatory, trauma, and allergy. There was a mild increase in the proportion of infective cases in 2020 to 61.3% of all cases (p = 0.0705), but normalized back to 59.4% in 2021. Most of the infective cases were bacterial cellulitis, followed by herpes zoster and fungal infection. Other bacterial infections seen included abscess, carbuncle, furuncle, and venereal diseases (accounting for a small percentage of total cases). Common viral infections included warts, herpes simplex, hand foot mouth disease. Lastly, other parasitic infections, such as scabies, lice were also seen.
In the COVID-19 period, inflammatory dermatoses became the second most encountered, averaging 9.5-9.8% of the presentations, a significant change from previous years (p = 7 × 10−4). Inflammatory conditions that were most seen included urticaria (acute and chronic, > 30% of all inflammatory cases), atopic dermatitis, followed by contact dermatitis (allergic and irritant).
Most frequent traumatic presentations included scalp laceration, animal bites, and bruising. For other diagnostic categories, notably, it was observed that there was a significant surge in allergy cases in 2021 (accounting for 9.2% of all cases seen, p = 6.9 × 10−14). Of the allergy cases, most were due to drugs and food (> 40%) and 10% of cases were anaphylactic in nature. Angioedema accounts for about 10% of all allergy cases. Conditions that do not belong to any subgroups were classified under “others”, which included, in order of frequency: cyst, ingrown toenail, non-immunobulous blisters, itch, lipoma, foreign body in skin, cancers etc. Under the autoimmune subgroup, systemic lupus erythematosus was most common (23%), followed by immunobullous disorders like bullous pemphigoid (19%) and vasculitides (13%). Ulcer conditions included arterial, venous, neuropathic, and pressure ulcers tend to occur at a more advanced age (average 65.7 years old). Cystic lesions (sebaceous, Bartholin, pilonidal), non-immune blisters and cancers (basal cell carcinoma, squamous cell carcinoma, malignant melanoma and other skin tumours) on a whole were much less commonly seen, accounting for 2.31% pre-COVID and dropped to 1.4% of all cases during COVID times and were subsumed under “Others” category to facilitate data visualization.
During the 4 years, conditions that experienced significant changes include inflammatory, trauma (including burns, laceration, bruise, bites, nail trauma, etc.), allergy, autoimmune, cysts, and cancers (p < 0.05 for all).
Dermatological emergencies such as Stevens-Johnson Syndrome, Toxic Epidermal Necrolysis, necrotising fasciitis and erythroderma were not as common and remained quite stable throughout the 4 years (less than 1% of total cases each year), with a slight surge in erythroderma to 34 cases in 2020 as seen in Supplementary Table S2.
The age and gender trends for different dermatological conditions are presented in Table 1 (a more detailed breakdown is presented in supplementary tables S3 and S4 for age and gender, respectively). There was not a very significant change in age distribution pre- and during COVID. The average age for all conditions was 56.2 years pre-COVID-19 and 55.1 after the onset of COVID-19. Conditions affecting more elderly (> 65 years) included cancers, ulcers, and autoimmune conditions. Conditions affecting younger populations included trauma, cysts, and allergy. Overall, men tended to present more commonly at the ED than women by 16-17%. Conditions that are male-predominant included infective (> 30% more frequent in men), ulcers, trauma, cancers. Conditions that are female-predominant included allergy, inflammatory.
Table 1 Gender and age distribution of dermatological conditions throughout the study
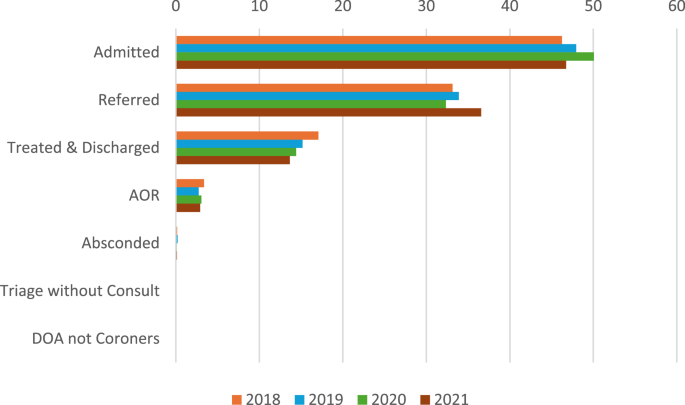
Disposition trends are presented in Fig. 2 and supplementary table S5. Overall, the majority of cases were admitted throughout the 4 years with a significant peak in 2020 (50.07%) compared to pre-COVID times ~ 47% (p = 3.35 × 10−5), despite a 15.6% drop in total cases presented as mentioned earlier. Referral trends were relatively stable from 2018 to 2020 (32.34-33.89%) and rose significantly to 36.57% in 2021 (p = 1.19 × 10−6). There was a gradual downtrend in terms of cases treated and discharged on the spot by ED physicians from 17.07% in 2018 to 13.65% in 2021 (p = 5.07 × 10−8). The number of patients discharged against medical advice (AOR) was relatively stable throughout the 4 years (~ 3%). Other dispositions (absconded, triage without consult, dead on arrival (DOA)) contributed a small (< 1%) proportion of all cases.
Disposition trends in percentage of dermatological conditions from 2018 to 2021 at SGH ED
Table 2 and supplementary Figure S1 show that there were more GP referrals compared to dermatologists pre-COVID (GP: dermatologist ~ 1.5). This trend was reversed during COVID time (GP: dermatologist ~ 0.6). The top 3 most common conditions for 2018–2020 were inflammatory, infective and others, whereas for 2021, most referrals to dermatologists were for inflammatory, allergy, and other conditions.
Table 2 Referral trends of dermatological cases presenting to SGH ED from 2018 to 2021