Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315:801. https://doi.org/10.1001/jama.2016.0287.
de Grooth H-J, Postema J, Loer SA, Parienti J-J, Oudemans-van Straaten HM, Girbes AR. Unexplained mortality differences between septic shock trials: a systematic analysis of population characteristics and control-group mortality rates. Intensive Care Med. 2018;44:311–22. https://doi.org/10.1007/s00134-018-5134-8.
Bauer M, Gerlach H, Vogelmann T, Preissing F, Stiefel J, Adam D. Mortality in sepsis and septic shock in Europe, North America and Australia between 2009 and 2019- results from a systematic review and meta-analysis. Crit Care. 2020;24:239. https://doi.org/10.1186/s13054-020-02950-2.
Zarbock A, Nadim MK, Pickkers P, Gomez H, Bell S, Joannidis M, et al. Sepsis-associated acute kidney injury: consensus report of the 28th Acute Disease Quality Initiative workgroup. Nat Rev Nephrol. 2023;19:401–17. https://doi.org/10.1038/s41581-023-00683-3.
Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S, et al. Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA. 2005;294:813–8. https://doi.org/10.1001/jama.294.7.813.
Schrier RW, Wang W. Acute renal failure and sepsis. N Engl J Med. 2004;351:159–69. https://doi.org/10.1056/nejmra032401.
Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Crit Care Med. 2021;49:e1063–143.
Russell JA. Vasopressor therapy in critically ill patients with shock. Intensive Care Med. 2019;45:1503–17. https://doi.org/10.1007/s00134-019-05801-z.
Dünser MW, Festic E, Dondorp A, Kissoon N, Ganbat T, Kwizera A, et al. Recommendations for sepsis management in resource-limited settings. Intensive Care Med. 2012;38:557–74. https://doi.org/10.1007/s00134-012-2468-5.
Avni T, Lador A, Lev S, Leibovici L, Paul M, Grossman A. Vasopressors for the treatment of septic shock: systematic review and meta-analysis. PLoS ONE. 2015;10: e0129305. https://doi.org/10.1371/journal.pone.0129305.
Ye E, Ye H, Wang S, Fang X. Initiation timing of vasopressor in patients with septic shock: a systematic review and meta-analysis. Shock. 2023. https://doi.org/10.1097/SHK.0000000000002214.
Sedhai YR, Shrestha DB, Budhathoki P, Memon W, Acharya R, Gaire S, et al. Vasopressin versus norepinephrine as the first-line vasopressor in septic shock: a systematic review and meta-analysis. J Clin Transl Res. 2022;8:185–99.
Backer D, Aldecoa C, Njimi H, Vincent J-L. Dopamine versus norepinephrine in the treatment of septic shock: a meta-analysis. Crit Care Med. 2012;40:725–30. https://doi.org/10.1097/CCM.0b013e31823778ee.
Huang P, Guo Y, Li B, Liu Q. Terlipressin versus norepinephrine for septic shock: a systematic review and meta-analysis. Front Pharmacol. 2019;10:1492. https://doi.org/10.3389/fphar.2019.01492.
Huang H, Wu C, Shen Q, Xu H, Fang Y, Mao W. The effect of early vasopressin use on patients with septic shock: a systematic review and meta-analysis. Am J Emerg Med. 2021;48:203–8. https://doi.org/10.1016/j.ajem.2021.05.007.
Belletti A, Musu M, Silvetti S, Saleh O, Pasin L, Monaco F, et al. Non-adrenergic vasopressors in patients with or at risk for vasodilatory shock. A systematic review and meta-analysis of randomized trials. PLoS ONE. 2015;10: e0142605. https://doi.org/10.1371/journal.pone.0142605.
Serpa Neto A, Nassar AP, Cardoso SO, Manetta JA, Pereira VGM, Espósito DC, et al. Vasopressin and terlipressin in adult vasodilatory shock: a systematic review and meta-analysis of nine randomized controlled trials. Crit Care. 2012;16:R154. https://doi.org/10.1186/cc11469.
Nagendran M, Russell JA, Walley KR, Brett SJ, Perkins GD, Hajjar L, et al. Vasopressin in septic shock: an individual patient data meta-analysis of randomised controlled trials. Intensive Care Med. 2019;45:844–55. https://doi.org/10.1007/s00134-019-05620-2.
Einav S, Helviz Y, Ippolito M, Cortegiani A. Vasopressor and inotrope treatment for septic shock: an umbrella review of reviews. J Crit Care. 2021;65:65–71. https://doi.org/10.1016/j.jcrc.2021.05.017.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358: j4008. https://doi.org/10.1136/bmj.j4008.
Vernon-Elliot J, Goradia S, Bellomo R, Lankadeva YR, Burrell LM, See EJ. The effect of catecholamine versus non-catecholamine vasopressors on renal function and recovery in vasodilatory shock: a systematic review of preclinical and clinical studies. Shock. 2024. https://doi.org/10.1097/SHK.0000000000002515.
Nedel WL, Rech TH, Ribeiro RA, Pellegrini JAS, Moraes RB. Renal outcomes of vasopressin and its analogs in distributive shock: a systematic review and meta-analysis of randomized trials. Crit Care Med. 2019;47:e44–51. https://doi.org/10.1097/ccm.0000000000003471.
Backer D, Deutschman CS, Hellman J, Myatra SN, Ostermann M, Prescott HC, et al. Surviving sepsis campaign research priorities 2023. Crit Care Med. 2024;52(2):268–96. https://doi.org/10.1097/CCM.0000000000006135.
de Backer D, Hajjar L, Monnet X. Vasoconstriction in septic shock. Intensive Care Med. 2024. https://doi.org/10.1007/s00134-024-07332-8.
See EJ, Clapham C, Liu J, Khasin M, Liskaser G, Chan JW, et al. A pilot study of angiotensin II as primary vasopressor in critically ill adults with vasodilatory hypotension: the ARAMIS study. Shock. 2023;59:691–6. https://doi.org/10.1097/SHK.0000000000002109.
de Backer D, Cecconi M, Chew MS, Hajjar L, Monnet X, Ospina-Tascón GA, et al. A plea for personalization of the hemodynamic management of septic shock. Crit Care. 2022;26:372. https://doi.org/10.1186/s13054-022-04255-y.
Wieruszewski PM, Khanna AK. Vasopressor choice and timing in vasodilatory shock. Crit Care. 2022;26:76. https://doi.org/10.1186/s13054-022-03911-7.
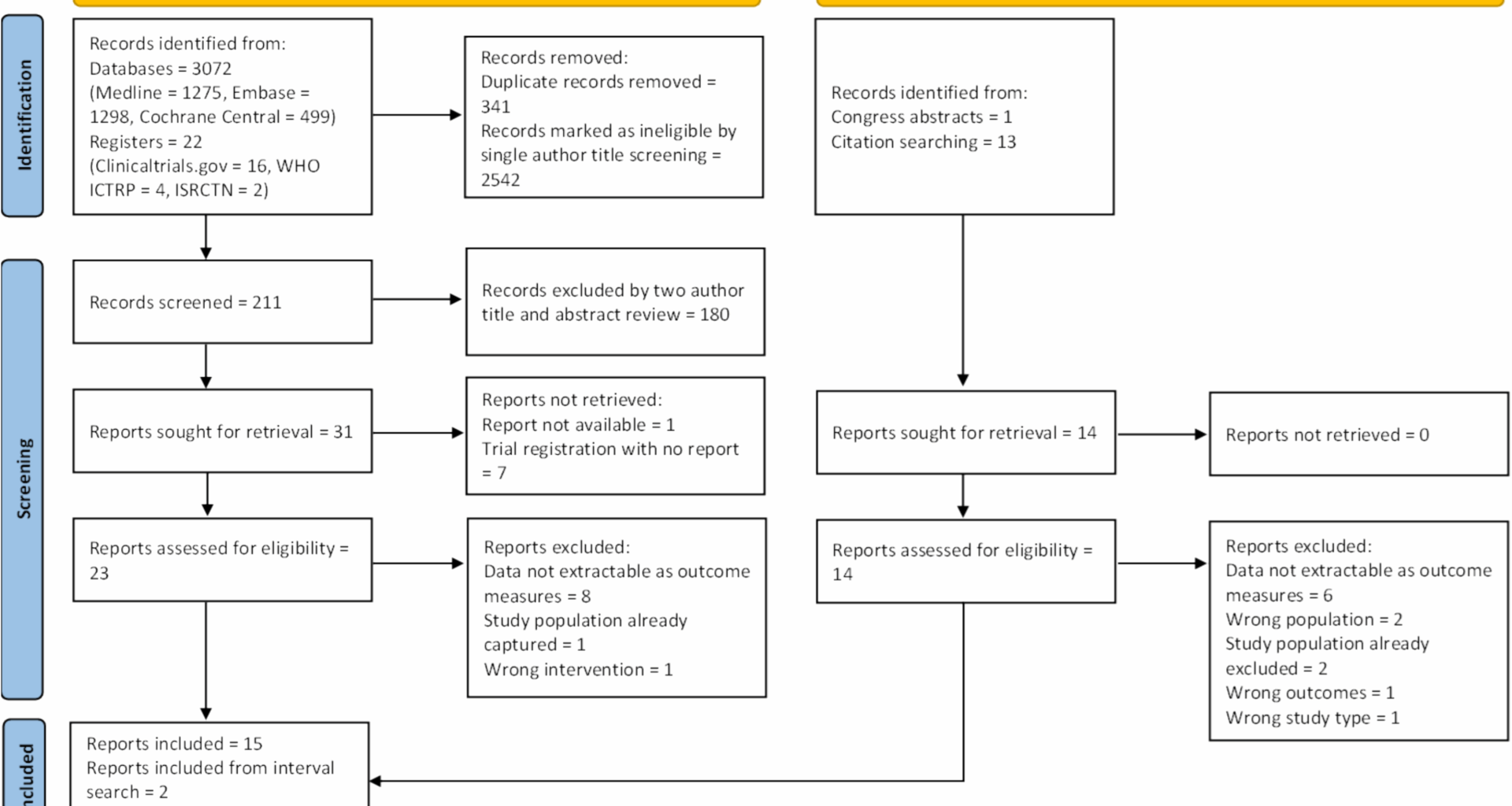
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71. https://doi.org/10.1136/bmj.n71.
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372: n160. https://doi.org/10.1136/bmj.n160.
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest. 1992;101:1644–55. https://doi.org/10.1378/chest.101.6.1644.
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Intensive Care Med. 2003;29:530–8. https://doi.org/10.1007/s00134-003-1662-x.
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group: KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2:1–138.
Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, Levin A. Acute kidney injury network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11:R31. https://doi.org/10.1186/cc5713.
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute renal failure– definition, outcome measures, animal models, fluid therapy and information technology needs: the second international consensus conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8:R204. https://doi.org/10.1186/cc2872.
Billings Iv FT, Shaw AD. Clinical trial endpoints in acute kidney injury. Nephron Clin Pract. 2014;127:89–93. https://doi.org/10.1159/000363725.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366: l4898. https://doi.org/10.1136/bmj.l4898.
Elmenesy TM, Nassar Y. A randomized double-blind comparative study between short-term norepinephrine and vasopressin infusion in septic shock. Egypt J Anaesth. 2008;24:355–62.
Wang J, Shi M, Huang L, Li Q, Meng S, Xu J, et al. Addition of terlipressin to norepinephrine in septic shock and effect of renal perfusion: a pilot study. Ren Fail. 2022;44:1207–15. https://doi.org/10.1080/0886022X.2022.2095286.
Lauzier F, Lévy B, Lamarre P, Lesur O. Vasopressin or norepinephrine in early hyperdynamic septic shock: a randomized clinical trial. Intensive Care Med. 2006;32:1782–9. https://doi.org/10.1007/s00134-006-0378-0.
Wieruszewski PM, Leone M, Kaas-Hansen BS, Dugar S, Legrand M, McKenzie CA, et al. Position paper on the reporting of norepinephrine formulations in critical care from the Society of Critical Care Medicine and European Society of Intensive Care Medicine Joint Task Force. Crit Care Med. 2024;52:521–30. https://doi.org/10.1097/CCM.0000000000006176.
Gordon AC, Mason AJ, Thirunavukkarasu N, Perkins GD, Cecconi M, Cepkova M, et al. Effect of early vasopressin vs norepinephrine on kidney failure in patients with septic shock. JAMA. 2016;316:509. https://doi.org/10.1001/jama.2016.10485.
Chawla LS, Busse L, Brasha-Mitchell E, Davison D, Honiq J, Alotaibi Z, Seneff MG. Intravenous angiotensin II for the treatment of high-output shock (ATHOS trial): a pilot study. Crit Care. 2014. https://doi.org/10.1186/s13054-014-0534-9.
Gupta T, Saini A, Gaur V, Goel A. Comparative study of Terlipressin and noradrenaline as vasopressors in patients with acute-on-chronic liver failure and septic shock: a randomized controlled trial. J Clin Exp Hepatol. 2025;15: 102494. https://doi.org/10.1016/j.jceh.2024.102494.
Liu Z-M, Chen J, Kou Q, Lin Q, Huang X, Tang Z, et al. Terlipressin versus norepinephrine as infusion in patients with septic shock: a multicentre, randomised, double-blinded trial. Intensive Care Med. 2018;44:1816–25. https://doi.org/10.1007/s00134-018-5267-9.
Xiao X, Zhang J, Wang Y, Zhou J, Zhu Y, Jiang D, et al. Effects of terlipressin on patients with sepsis via improving tissue blood flow. J Surg Res. 2016;200:274–82. https://doi.org/10.1016/j.jss.2015.07.016.
Hajjar LA, Zambolim C, Belletti A, de Almeida JP, Gordon AC, Oliveira G, et al. Vasopressin versus norepinephrine for the management of septic shock in cancer patients: the VANCS II randomized clinical trial. Crit Care Med. 2019;47:1743–50. https://doi.org/10.1097/CCM.0000000000004023.
Davoudi-Monfared E, Mohammadi M, Khoshavi M, Khalili H. The effect of midodrine on lactate clearance in patients with septic shock: a pilot study. J Comp Eff Res. 2021;10:673–83.
Laterre P-F, Berry SM, Blemings A, Carlsen JE, François B, Graves T, et al. Effect of selepressin vs placebo on ventilator- and vasopressor-free days in patients with septic shock: the SEPSIS-ACT randomized clinical trial. JAMA. 2019;322:1476–85. https://doi.org/10.1001/jama.2019.14607.
Morelli A, Ertmer C, Rehberg S, Lange M, Orecchioni A, Cecchini V, et al. Continuous terlipressin versus vasopressin infusion in septic shock (TERLIVAP): a randomized, controlled pilot study. Crit Care. 2009;13:R130. https://doi.org/10.1186/cc7990.
Barzegar E, Ahmadi A, Mousavi S, Nouri M, Mojtahedzadeh M. The therapeutic role of vasopressin on improving lactate clearance during and after vasogenic shock: microcirculation, is it the black box? Acta Med Iran. 2016;54:15–23.
Russell JA, Walley KR, Singer J, Gordon AC, Hébert PC, Cooper DJ, et al. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 2008;358:877–87. https://doi.org/10.1056/NEJMoa067373.
Sahoo P, Kothari N, Goyal S, Sharma A, Bhatia PK. Comparison of norepinephrine and terlipressin vs norepinephrine alone for management of septic shock: a randomized control study. Indian J Crit Care Med. 2022;26:669–75.
Choudhury A, Kedarisetty CK, Vashishtha C, Saini D, Kumar S, Maiwall R, et al. A randomized trial comparing terlipressin and noradrenaline in patients with cirrhosis and septic shock. Liver Int. 2017;37:552–61. https://doi.org/10.1111/liv.13252.
Zampieri FG, Bagshaw SM, Njimi H, Vincent J-L, DeBacker D. Exploration of different statistical approaches in the comparison of dopamine and norepinephrine in the treatment of shock: SOAP II. Crit Care. 2024;28:299. https://doi.org/10.1186/s13054-024-05016-9.
de Backer D, Biston P, Devriendt J, Madl C, Chochrad D, Aldecoa C, et al. Comparison of dopamine and norepinephrine in the treatment of shock. N Engl J Med. 2010;362:779–89. https://doi.org/10.1056/NEJMoa0907118.
Morelli A, Ertmer C, Rehberg S, Lange M, Orecchioni A, Laderchi A, et al. Phenylephrine versus norepinephrine for initial hemodynamic support of patients with septic shock: a randomized, controlled trial. Crit Care. 2008;12:R143. https://doi.org/10.1186/cc7121.
Busse LW, Ostermann M. Vasopressor therapy and blood pressure management in the setting of acute kidney injury. Semin Nephrol. 2019;39:462–72. https://doi.org/10.1016/j.semnephrol.2019.06.006.
Chawla LS, Eggers PW, Star RA, Kimmel PL. Acute kidney injury and chronic kidney disease as interconnected syndromes. N Engl J Med. 2014;371:58–66. https://doi.org/10.1056/NEJMra1214243.
Vaara ST, Serpa Neto A, Bellomo R, Adhikari NKJ, Dreyfuss D, Gallagher M, et al. Regional practice variation and outcomes in the standard versus accelerated initiation of renal replacement therapy in acute kidney injury (STARRT-AKI) trial: a post hoc secondary analysis. Crit Care Explor. 2024;6: e1053. https://doi.org/10.1097/CCE.0000000000001053.
Maeda A, Inokuchi R, Bellomo R, Doi K. Heterogeneity in the definition of major adverse kidney events: a scoping review. Intensive Care Med. 2024;50:1049–63. https://doi.org/10.1007/s00134-024-07480-x.
Zarbock A, Forni LG, Ostermann M, Ronco C, Bagshaw SM, Mehta RL, et al. Designing acute kidney injury clinical trials. Nat Rev Nephrol. 2024;20:137–46. https://doi.org/10.1038/s41581-023-00758-1.
Zarbock A, Forni LG, Koyner JL, Bell S, Reis T, Meersch M, et al. Recommendations for clinical trial design in acute kidney injury from the 31st acute disease quality initiative consensus conference. A consensus statement. Intensive Care Med. 2024;50:1426–37. https://doi.org/10.1007/s00134-024-07560-y.
McIlroy DR, Bellomo R, Billings IVFT, Karkouti K, Prowle JR, Shaw AD, Myles PS. Systematic review and consensus definitions for the Standardised Endpoints in Perioperative Medicine (StEP) initiative: renal endpoints. Br J Anaesth. 2018;121:1013–24. https://doi.org/10.1016/j.bja.2018.08.010.
Khanna A, English SW, Wang XS, Ham K, Tumlin J, Szerlip H, et al. Angiotensin II for the treatment of vasodilatory shock. N Engl J Med. 2017;377:419–30. https://doi.org/10.1056/NEJMoa1704154.
Tumlin JA, Murugan R, Deane AM, Ostermann M, Busse LW, Ham KR, et al. Outcomes in patients with vasodilatory shock and renal replacement therapy treated with intravenous angiotensin II. Crit Care Med. 2018;46:949–57. https://doi.org/10.1097/CCM.0000000000003092.
Ostermann M, Lumlertgul N, Jeong R, See E, Joannidis M, James M. Acute kidney injury. Lancet. 2025;405:241–56. https://doi.org/10.1016/S0140-6736(24)02385-7.