Cervical carcinoma is one of the most common malignancies among women worldwide, which has been becoming a serious public health problem all over the world. Various researches had confirmed that the high-risk type HPV persistent infection was the main factor causing cervical carcinoma and precancerous lesions in women. In China, the prevalence of HPV was greatly varies between provinces [17]. However, the researches on the prevalence of HPV infection in Henan Province were rare. In our study, we provide evidence for the prevalence and genotype data in Henan Province.
In this study, among the enrolled participants, the overall prevalence of HPV was 21.31% (12,950/60,765), which is consistent with the reported rates of 21.0% in the Beijing area [18] and 22.41% in the Hangzhou [19]. It was lower than the rates in Heilongjiang at 27.1% [12] and Shandong at 28.4% [20], but higher than the reported rates in Hubei at 16.09% [21] and Xiamen at 17.13% [22]. In the distribution within the Henan region, it is higher than the reported rate of 19.7% in northern Henan [23]. These differences may be attributed to variations in population composition, education levels, and economic status among different regions [24]. These data suggest that the HPV infection level in Henan remains relatively high. We should strengthen education and vaccination efforts in the region to reduce the HPV infection rate.
Most studies have been only used the outpatient samples for the HPV epidemiology. Since the outpatients usually visit the hospital for further treatment, the HPV prevalence may be different from the whole population. Our study cohort comprised a large sample of women from both a routine health screening setting (n=10,750) and a hospital-based clinical care setting (n=50,015). It is important to note that the combined cohort is not intended to be a perfect representation of the general population of Henan Province, as hospital-based studies are susceptible to selection bias (e.g., the Outpatient/Inpatient Group may have a higher burden of health issues). However, the immense size of our dataset provides a powerful snapshot of the circulating HPV genotypes within a major tertiary hospital catchment area. The Health Examination Group sub-cohort, while also subject to the biases of a self-selected screening population, offers a better estimate of prevalence in asymptomatic women. The primary value of our data lies in the detailed analysis of genotype distribution, which is less likely to be severely skewed by the sampling framework than the absolute prevalence estimate. The results showed that the HPV prevalence in the Health Examination Group was only 14.73% (1,584/10,750), which is significantly lower than that of 21.31% (12,950/60,765) and the prevalence of Outpatient/Inpatient Group at 22.73% (11,366/50,015). Among the positive patients, HR-HPV infections accounted for 83.67% (10,836/12,950).
In genotype infections, single-type infections accounted for 69.51% (9,001/12,950), double infections accounted for 19.95% (2,584/12,950), and multiple infections accounted for 10.52% (1,365/12,950). Single-type infections were the predominant infection type, consistent with reports from most regions across the country. In this study, the highest number of genotypes observed in a single infection reached up to 9-fold infections.
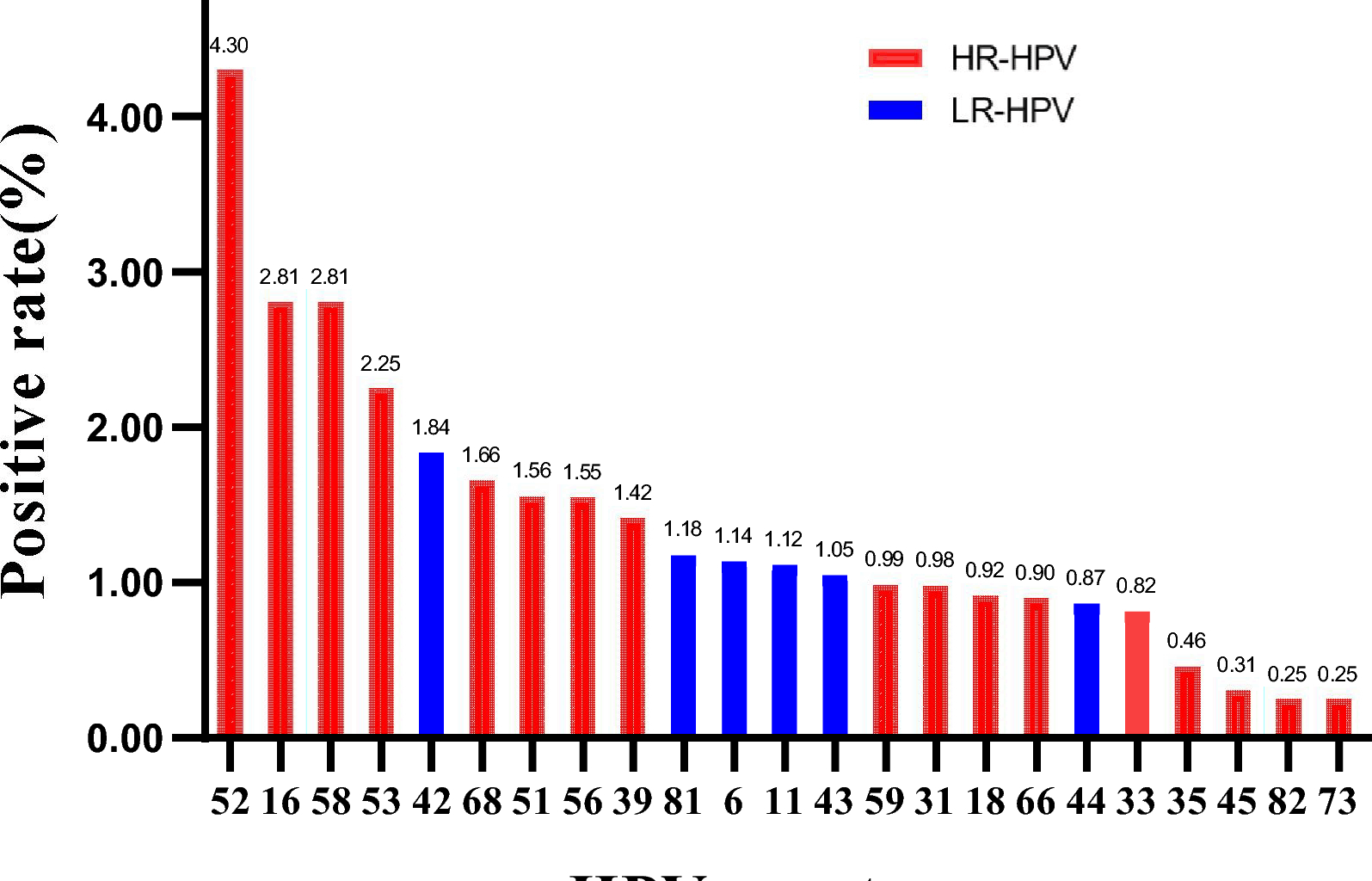
As widely acknowledged, the distribution of HPV genotypes plays a crucial role in shaping vaccination strategies and providing essential data support. Among the high-risk HPV genotypes, HPV 16, 18, 31, 58, and 52 were globally prevalent, with particular emphasis on HPV 16 and 18, which were detected in approximately 70% of cervical cancer cases [25]. In various regions of China, the most frequently observed high-risk HPV genotypes are HPV 16, 52, and 58 [24, 26]. Our research findings indicate that the top five high-risk HPV genotypes, namely 52, 16, 58, 53, and 39, are closely associated with the occurrence of cervical cancer. Notably, HPV 52 exhibits the highest prevalence rate, accounting for 4.30% (2,612/60,765), higher than the 16 and 18 types with higher prevalence worldwide. In addition, we also analyzed the distribution of LR-HPV, and its top three genotypes were HPV42, 81, 6. These results indicate that in addition to considering the traditional HR-HPV 16 and 18 genotypes, the 52, 58, 53 genotypes with higher prevalence also should be included in our vaccination plan in Henan Province.
As a result of this study, we found that the age group under 20 had the highest HPV infection rate, reaching 34.02% (395/1,161). On the other hand, the age group over 60 had the second highest infection rate, reaching 27.06% (679/2,509). Among individuals aged 21–60, the HPV infection rate exhibits a trend of initially decreasing and then increasing, with the lowest HPV infection rate observed in the 41–50 age group, followed by a continuous increase.
The distribution of infections across various age groups exhibits a “U” shaped pattern, akin to investigations conducted on the female populace in China [24] and internationally [27]. Females under the age of 20 demonstrate a higher prevalence of HPV infection, potentially attributed to more frequent engagement in sexual activity without sufficient protective measures, as well as an incompletely developed immune system [28]. It has been documented that the infections in the majority of young women are transient [29].
After the age of 50, there was an increase in the HPV infection rate, possibly due to changes of women in the perimenopausal period, which may experience hormonal fluctuations and a decline in physical function, leading to a weakened immune system [10, 30]. This can result in reduced ability to clear viral infections, leading to sustained viral infections and disease progression. We observed that women in the ≤20 and >60 age groups, the overall infection rate, single infection rate, dual infection rate, and multiple infection rate were all very high. Therefore, we should simultaneously strengthen vaccination efforts for teenagers and HPV screening for the elderly regularly [31, 32]. This approach may help reduce HPV infections and the incidence of cervical cancer. In addition, among the distribution of infected individuals, the age of 21–60 years old has the highest number of infections. While we focus on the infection rate, it is also important to consider the size of the infected population. This can better guide us in formulating prevention and treatment strategies for HPV.
This research has certain limitations that should be considered. The primary limitation is the lack of detailed clinical data, such as cytology or histology results, which prevents us from determining the actual disease status (e.g., normal, CIN1, CIN2+, or cancer) of the HPV-positive individuals. Therefore, our results depict the circulation of HPV genotypes in the population but cannot directly assess their association with cervical disease progression. Secondly, as a single-center study, although conducted at a major referral hospital, our participant cohort may not be fully representative of the entire population of Henan Province, potentially limiting the generalizability of our findings. The patient population at a large tertiary hospital might differ from that in community screening centers. Future multi-center studies that combine HPV genotyping with clinical outcomes are essential to confirm the oncogenic impact of the most prevalent genotypes and to provide more robust data on the HPV prevalence landscape for the region.