Bauersachs J, König T, van der Meer P, Petrie MC, Hilfiker-Kleiner D, Mbakwem A, et al. Pathophysiology, diagnosis and management of peripartum cardiomyopathy: a position statement from the Heart Failure Association of the European Society of Cardiology study group on peripartum cardiomyopathy. Eur J Heart Fail. 2019;21(7):827–43.
Sliwa K, Petrie MC, van der Meer P, Mebazaa A, Hilfiker-Kleiner D, Jackson AM, et al. Clinical presentation, management, and 6-month outcomes in women with peripartum cardiomyopathy: an ESC EORP registry. Eur Heart J. 2020;41:3787–97.
Davis MB, Arany Z, McNamara DM, Goland S, Elkayam U. Peripartum cardiomyopathy: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75(2):207–21.
Hilfiker-Kleiner D, Haghikia A, Masuko D, Nonhoff J, Held D, Libhaber E, et al. Outcome of subsequent pregnancies in patients with a history of peripartum cardiomyopathy. Eur J Heart Fail. 2017;19:1723–8.
Stergiopoulos K, Lima FV. Peripartum cardiomyopathy-diagnosis, management, and long term implications. Trends Cardiovasc Med. 2019;29:164–73.
Sliwa K, Petrie MC, Hilfiker-Kleiner D, Mebazaa A, Jackson A, Johnson MR, et al. Long-term prognosis, subsequent pregnancy, contraception and overall management of peripartum cardiomyopathy: practical guidance paper from the heart failure association of the European society of cardiology study group on peripartum cardiomyopathy. Eur J Heart Fail. 2018;20:951–62.
LeeS CGJ, ParkGU KLY, Choi LTSKDY, Youn SW, Han JC, Ryu SW, Na KH, Choi JO, Seo CU, Kim HS. Incidence, risk factors, and clinical characteristics of peripartum cardiomyopathy in South Korea. Circ Heart Fail. 2018;11:e0041347.
Kao DP, Hsich E, Lindenfeld J. Characteristics, adverse events, and racial differences among delivering mothers with peripartum cardiomyopathy. JACC: Heart Failure. 2013;1(5):409–16.
Behrens I, Basit S, Lykke JA, Ranthe MF, Wohlfahrt J, Bundgaard H, et al. Hypertensive disorders of pregnancy and peripartum cardiomyopathy: a nationwide cohort study. PLoS ONE. 2019;14(2):e0211857.
Barasa A, Rosengren A, Sandström TZ, Ladfors L, Schaufelberger M. Heart failure in late pregnancy and postpartum: incidence and long-term mortality in Sweden from 1997 to 2010. J Card Fail. 2017;23(5):370–8.
Zahid S, Hashem A, Minhas AS, Bennett WL, Honigberg MC, Lewey J, et al. Trends, predictors, and outcomes of cardiovascular complications at delivery associated with gestational diabetes: a national inpatient sample analysis (2004–2019). J Am Heart Assoc. 2022;11(21):e026786.
Malhamé I, Dayan N, Moura CS, Samuel M, Vinet E, Pilote L. Peripartum cardiomyopathy with co-incident preeclampsia: a cohort study of clinical risk factors and outcomes among commercially insured women. Pregnancy Hypertens. 2019;17:82–8.
Gunderson EP, Croen LA, Chiang V, Yoshida CK, Walton D, Go AS. Epidemiology of peripartum cardiomyopathy: incidence, predictors, and outcomes. Obstet Gynecol. 2011;118(3):583–91.
Jackson AM, Macartney M, Brooksbank K, Brown C, Dawson D, Francis M, et al. A 20-year population study of peripartum cardiomyopathy. Eur Heart J. 2023;44(48):5128–41.
Nabbaale J, Okello E, Kibirige D, Ssekitoleko I, Isanga J, Karungi P, et al. Burden, predictors and short-term outcomes of peripartum cardiomyopathy in a black African cohort. PLoS ONE. 2020;15(10):e0240837.
Prameswari HS, Dewi TI, Hasan M, Martanto E, Aprami TM. Hypertension in pregnancy as the most influential risk factor for PPCM. Br J Cardiol. 2018;25:111–4.
Puhakka AM, Macharey G, Ziller V, Gissler M, Tekay A, Keil C, Hilfiker-Kleiner D. Peripartum heart failure in Finland: A population-based record linkage study. ESC Heart Fail., Gentry MB, Dias JK, Luis A, Patel R, Thornton J, Reed GL. African-American women have a higher risk for developing peripartum cardiomyopathy. JAmColl Cardiol. 2010;55:654–59.
Bello N, Rendon IS, Arany Z. The relationship between pre-eclampsia and peripartum cardiomyopathy: a systematic review and meta-analysis. J AmColl Cardiol. 2013;62:1715–23.
Azad H, Wen T, Bello NA, Booker WA, Purisch S, D’Alton ME, et al. Peripartum cardiomyopathy delivery hospitalization and postpartum readmission trends, risk factors, and outcomes. Pregnancy Hypertens. 2023;34:116–23.
Gambahaya ET, Minhas AS, Sharma G, Vaught AJ, Adamo L, Zakaria S, et al. Racial differences in delivery outcomes among women with peripartum cardiomyopathy. CJC Open. 2021;4(4):373–7.
Echouffo-Tcheugui JB, Guan J, Fu L, Retnakaran R, Shah BR. Incidence of heart failure related to co-occurrence of gestational hypertensive disorders and gestational diabetes. JACC: Advances. 2023;2(4):10037.
Dhesi S, Savu A, Ezekowitz JA, Kaul P. Association between diabetes during pregnancy and peripartum cardiomyopathy: a population-level analysis of 309,825 women. Can J Cardiol. 2017;33:911–7.
Stapel B, Kohlhaas M, Ricke-Hoch M, Haghikia A, Erschow S, Knuuti J, Silvola JM, Roivainen A, Saraste A, Nickel AG, Saar JA, Sieve I, Pietzsch S, Muller M, Bogeski I, Kappl R, Jauhiainen M, Thackeray JT, Scherr M, Bengel FM, Hagl C, Tudorache I, Bauersachs J, Maack C, Hilfiker-Kleiner D. Low STAT3 expression sensitizes to toxic effects of beta-adrenergic receptor stimulation in peripartum cardiomyopathy. Eur Heart J. 2017;38:349–61.
Goland S, Weinstein JM, Zalik A, Kuperstein R, Zilberman L, Shimoni S, et al. Angiogenic imbalance and residual myocardial injury in recovered peripartum cardiomyopathy patients. Circ Heart Fail. 2016;9(11):e003349.
Safira A, Tjahjadi AK, Adytia GJ, Waitupu A, Sutanto H. Peripartum cardiomyopathy unveiled: etiology, diagnosis, and therapeutic insights. Curr Probl Cardiol. 2024;49(5):102474.
Ware JS, Li J, Mazaika E, Yasso CM, DeSouza T, Cappola TP, Tsai EJ, Hilfiker-Kleiner D, Kamiya CA, Mazzarotto F, Cook SA, Halder I, Prasad SK, Pisarcik J, Hanley-Yanez K, Alharethi R, Damp J, Hsich E, Elkayam U, Sheppard R, Kealey A, Alexis J, Ramani G, Safirstein J, Boehmer J, Pauly DF, Wittstein IS, Tho V, Zucker MJ, Liu P, Gorcsan J 3rd, McNamara DM, Seidman CE, Seidman JG, Arany Z. IMAC-2 and IPAC Investigators. Shared genetic predisposition in peripartum and dilated cardiomyopathies. NEngl JMed. 2016;374:233–41.
Ware JS, Li J, Mazaika E, Yasso CM, DeSouza T, Cappola TP, Tsai EJ, Hilfiker-Kleiner D, Kamiya CA, Mazzarotto F, Cook SA, Halder I, Prasad SK, Pisarcik J, Hanley-Yanez K, Alharethi R, Damp J, Hsich E, Elkayam U, Sheppard R, Kealey A, Alexis J, Ramani G, Safirstein J, Boehmer J, Pauly DF, Wittstein IS, Thohan V, Zucker MJ, Liu P, Gorcsan J 3rd, McNamara DM, Seidman CE, Seidman JG, Arany Z. IMAC-2 and IPAC Investigators. Shared genetic predisposition in peripartum and dilated cardiomyopathies. N Engl J Med. 2016;374(3):233–41.
Spracklen TF, Chakafana G, Schwartz PJ, Kotta MC, Shaboodien G, Ntusi NAB, et al. Genetics of peripartum cardiomyopathy: current knowledge, future directions and clinical implications. Genes. 2021;12(1):103.
Kumar A, Ravi R, Sivakumar RK, Chidambaram V, Majella MG, Sinha S, Adamo L, Lau ES, Al’Aref SJ, Asnani A, Sharma G, Mehta JL. Prolactin Inhibition in peripartum cardiomyopathy: systematic review and Meta-analysis. Curr Probl Cardiol. 2023;48(2):101461.
Polsinelli VB, Hanley-Yanez K, McTiernan CF, Modi K, Haythe J, Skopicki H, Elkayam U, Cooper LT Jr, Fett JD, McNamara DM. IPAC investigators. Cathepsin-D and outcomes in peripartum cardiomyopathy: results from IPAC. Am Heart J Plus. 2024;49:100489.
Karaye KM, Yahaya IA, Lindmark K, Henein MY. Serum selenium and ceruloplasmin in Nigerians with peripartum cardiomyopathy. Int J Mol Sci. 2015;16:7644–54.
Kryczka KE, Demkow M, Dzielińska Z. Biomarkers in peripartum cardiomyopathy-what we know and what is still to be found. Biomolecules. 2024;14(1):103.
Bello NA, Arany Z. Molecular mechanisms of peripartum cardiomyopathy: a vascular/hormonal hypothesis. Trends Cardiovasc Med. 2015;25:499–504.
Mebazaa A, Seronde MF, Gayat E, Tibazarwa K, Anumba DOC, Akrout N, et al. Imbalanced angiogenesis in peripartum cardiomyopathy – diagnostic value of placenta growth factor. Circ J. 2017;81(11):1654–61.
Rana S, Burke SD, Karumanchi SA. Imbalances in circulating angiogenic factors in the pathophysiology of preeclampsia and related disorders. Am J Obstet Gynecol. 2022;226(2S):S1019-34.
Kryczka KE, Demkow M, Dzielińska Z. Biomarkers in peripartum cardiomyopathy—what we know and what is still to be found. Biomolecules. 2024;14:103.
Ersbøll AS, Goetze JP, Johansen M, Hauge MG, Sliwa K, Vejlstrup N, et al. Biomarkers and their relation to cardiac function late after peripartum cardiomyopathy. J Card Fail. 2021;27(2):168–75.
Damp J, Givertz MM, Semigran M, Alharethi R, Ewald G, Felker GM, Bozkurt B, Boehmer J, Haythe J, Skopicki H, Hanley-Yanez K, Pisarcik J, Halder I, Gorcsan J 3rd, Rana S, Arany Z, Fett JD, McNamara DM. IPAC Investigators. Relaxin-2 and soluble Flt1 levels in peripartum cardiomyopathy: results of the multicenter IPAC study. JACC Heart Fail. 2016;4(5):380–8.
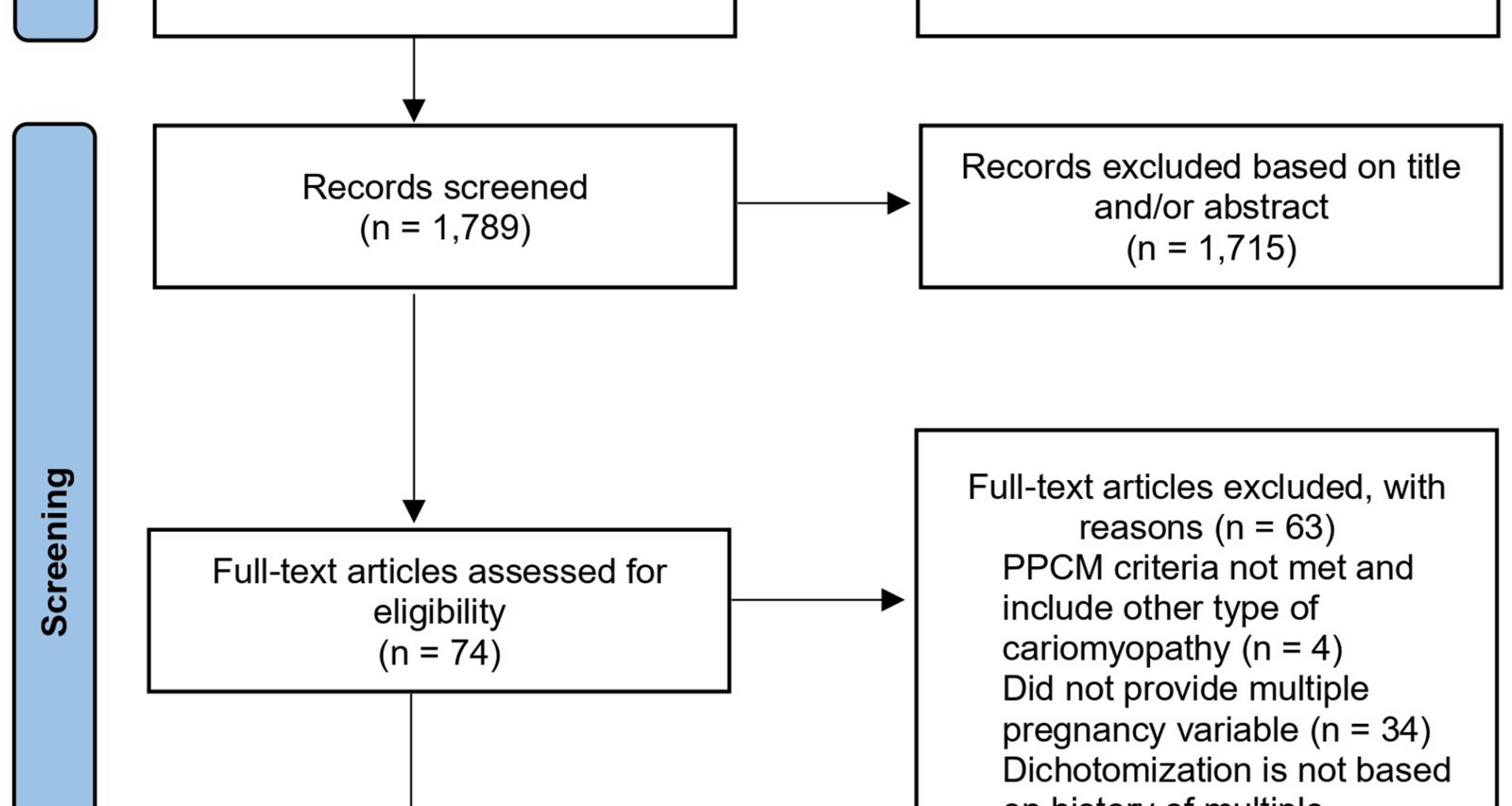
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5.
Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Vol. 5.1.0. The Cochrane Collaboration; 2011.
Hoes MF, Arany Z, Bauersachs J, Hilfiker-Kleiner D, Petrie MC, Sliwa K, et al. Pathophysiology and risk factors of peripartum cardiomyopathy. Nat Rev Cardiol. 2022;19:555–65.
Hilfiker-Kleiner D, Kaminski K, Podewski E, Bonda T, Schaefer A, Sliwa K, et al. A cathepsin D-cleaved 16 kDa form of prolactin mediates postpartum cardiomyopathy. Cell. 2007;128:589–600.
Bollen IAE, Ehler E, Fleischanderl K, Bouwman F, Ricke-Hoch KL. Myofilament remodeling and function is more impaired in peripartum cardiomyopathy compared with dilated cardiomyopathy and ischemic heart disease. Am J Pathol. 2017;187:2645–58.
Hiersch L, Ray JG, Barrett J, Berger H, Geary M, McDonald SD, et al. DOH-NET (Diabetes, obesity and hypertension in pregnancy research Network). Maternal cardiovascular disease after twin pregnancies complicated by hypertensive disorders of pregnancy: a population-based cohort study. CMAJ. 2021;193(37):E1448–58.
Korzeniewski SJ, Romero R, Chaiworapongsa T, et al. Maternal plasma angiogenic index-1 (placental growth factor/soluble vascular endothelial growth factor receptor-1) is a biomarker for the burden of placental lesions consistent with uteroplacental underperfusion: a longitudinal case-cohort study. Am J Obstet Gynecol. 2016;214:e6291–17.
Silasi M, Cohen B, Karumanchi SA, et al. Abnormal placentation, angiogenic factors, and the pathogenesis of preeclampsia. Obstet Gynecol Clin North Am. 2010;37:239–53.
Young BC, Levine RJ, Karumanchi SA. Pathogenesis of preeclampsia. Annu Rev Pathol. 2010;5:173–92.
Udell JA, Lu H, Redelmeier DA. Failure of fertility therapy and subsequent adverse cardiovascular events. CMAJ. 2017;189:E391–7.
Satorres E, Martínez-Varea A, Diago-Almela V. SFlt-1/PlGF ratio as a predictor of pregnancy outcomes in twin pregnancies: a systematic review. J Matern Fetal Neonatal Med. 2023;36(2):2230514.
Dröge L, Herraìz I, Zeisler H, Schlembach D, Stepan H, Küssel L, et al. Maternal serum sFlt-1/PlGF ratio in twin pregnancies with and without pre-eclampsia in comparison with singleton pregnancies. Ultrasound Obstet Gynecol. 2015;45(3):286–93.
Yang M, Bai Y, Li M, Lin X, Duan X, Zhang X. Predictive value of the soluble fms-like tyrosine kinase 1 to placental growth factor ratio for preeclampsia in twin pregnancies: a systematic review and meta-analysis. American Journal of Obstetrics & Gynecology MFM. 2024;6(3):101290.
De La Calle M, Delgado JL, Verlohren S, Escudero AI, Bartha JL, Campillos JM, De La Aguarón A, et al. Gestational Age-Specific reference ranges for the sFlt-1/PlGF immunoassay ratio in twin pregnancies. Fetal Diagn Ther. 2021;48(4):288–96.
Binder J, Palmrich P, Pateisky P, Kalafat E, Kuessel L, Zeisler H, et al. The prognostic value of angiogenic markers in twin pregnancies to predict delivery due to maternal complications of preeclampsia. Hypertension. 2020;76(1):176–83.
Halkein J, Tabruyn SP, Ricke-Hoch M, Haghikia A, Nguyen NQ, Scherr M, et al. Microrna-146a is a therapeutic target and biomarker for peripartum cardiomyopathy. J Clin Invest. 2013;123(5):2143–54.
Ricke-Hoch M, Hoes MF, Pfeffer TJ, Schlothauer S, Nonhoff J, Haidari S, et al. In peripartum cardiomyopathy plasminogen activator inhibitor-1 is a potential new biomarker with controversial roles. Cardiovasc Res. 2020;116:1875–86.
Gorog DA, Vilahur G. Peripartum cardiomyopathy: can the link between prolactin and PAI-1 provide a clue? Cardiovasc Res. 2020;116(11):1791–3.