Many earlier studies and classical anatomy textbooks have agreed that the LPM consists of two heads: the SLPM and the ILPM [3, 19, 20]. However, more recent anatomical research has reported the presence of medial fibers, suggesting that the LPM may in fact be composed of three distinct parts [11, 21, 22]. In our study, medial fibers were observed in 9.8% of cases, supporting the findings of these recent investigations. Pompei Filho et al. [22] reported a prevalence of 20.22% for the third head in their MRI-based study, while Dergin et al. [8] found it in 29.6% of cases.
The literature presents variability regarding LPM attachment patterns. Visibility of more than two heads may depend on factors such as signal quality, imaging sequences, slice thickness, and the angulation of oblique sagittal slices relative to the condylar head. Although most authors agree that the ILPM inserts into the condyle, there is less consensus regarding the insertion site of the SLPM [7, 8, 10].
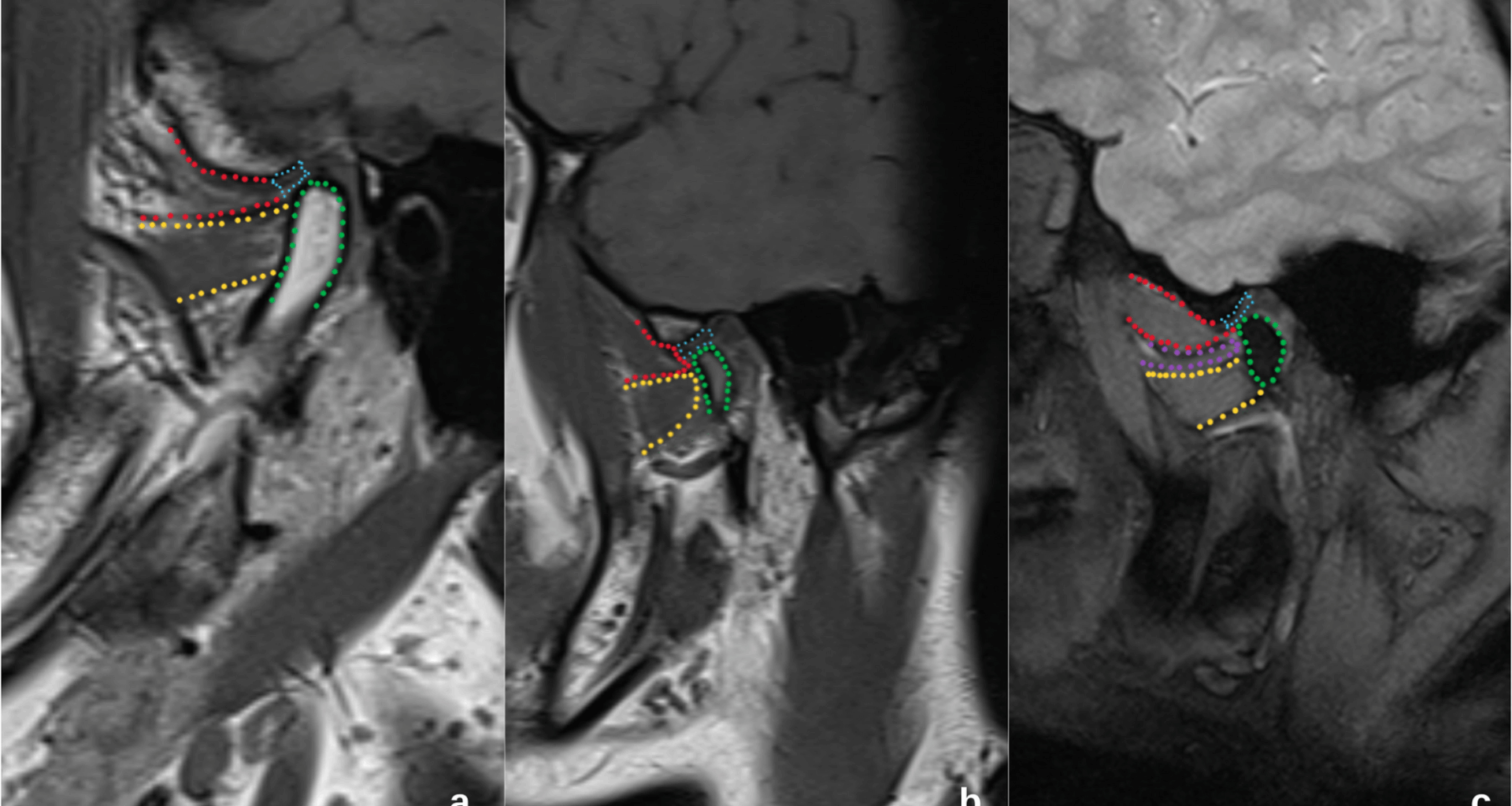
Our results confirm that the LPM demonstrates variable attachment patterns. MRI evaluations in this study identified three different types of attachment to the DCC. One of the key challenges in the literature arises from the absence of a standardized classification system for these attachment types. For instance, Kılıç et al. [11] defined four types, while Litko et al. [17] used a three-type classification. Our study adopted the system proposed by Litko et al. [17], as outlined in Figure-1.
Dergin et al. [8], in their study examining the relationship between LPM attachment types and IDs, reported that the group in which the SLPM was attached to the disc and the ILPM to the condyle was present in 29.6% of cases. The configuration in which the SLPM was attached to both the disc and condyle, and the ILPM to the condyle, was seen in 40.8%, while the pattern involving SLPM to the disc and both middle and inferior heads to the condyle was also found in 29.6%.
In a cadaveric study, Kılıç et al. [11] identified four different attachment patterns: in 36.7% of cases, the SLPM was attached to both the DCC and the condyle, while the ILPM was attached only to the condyle; in 28.6%, the SLPM was attached to the DCC and the ILPM to the condyle; in 26.5%, both heads were attached to the condyle; and in 8.2%, the SLPM was attached to the DCC, while the ILPM was attached to both the DCC and the condyle.
Antonopoulou et al. [7], in a study involving 18 cadavers, reported that the SLPM was attached to both the condyle and DCC in 55.5% of cases, to the condyle only in 27.8%, and to the DCC only in 16.7%. In their MRI-based analysis of 382 joints, Litko et al. [17] found that in 7.6% of cases, the SLPM was attached to the disc and the ILPM to the condyle; in 66.7%, the SLPM was attached to both the disc and condyle; and in 25.7%, the SLPM was attached to the disc while the ILPM and MLPM were attached to the condyle.
Taskaya-Yılmaz et al. [4] published a study including MRI images of 272 TMJs—42 with normal disc position, 166 with DDwR, and 64 with DDwoR—to investigate the relationship between LPM and internal derangement. Among the 42 TMJs with normal disc position, 76.2% had the SLPM attached to the disc and the ILPM to the condyle, while 23.8% had the SLPM attached to both the disc and condyle and the ILPM to the condyle. Among the 166 TMJs with DDwR, 57.2% had the SLPM attached to the disc and the ILPM to the condyle, while 42.8% had the SLPM attached to both the disc and condyle and the ILPM to the condyle. Among the 64 TMJs with DDwoR, 85.9% showed SLPM to disc and ILPM to condyle, while 14.1% showed SLPM to both disc and condyle and ILPM to condyle.
In our study, Type 1 attachment (ILPM to the condyle and SLPM to the disc) was observed in 27.8%, Type 2 (SLPM to both disc and condyle and ILPM to condyle) in 62.4%, and Type 3 (SLPM to the disc and ILPM and medial fibers to the condyle) in 9.8% of cases.
Studies investigating the relationship between LPM attachment types and disc displacement have reported conflicting results. Yeşiltepe et al. [18], in an MRI-based study, found that the LPM area was smaller in the DDwR group and larger in the DDwoR group, though the difference was not statistically significant. Similarly, Taskaya-Yılmaz et al. [4], Dergin et al. [8], Imanimoghaddam et al. [9], and Omami et al. [10] also found no significant correlation between LPM attachment and disc displacement.
On the other hand, Litko et al. [17] reported a significant correlation between these variables. This discrepancy may stem from the fact that they evaluated disc position not only in the sagittal plane but also in the coronal plane and included anterior, anteromedial, and anterolateral displacements. Moreover, their use of oblique sagittal slices aligned parallel to the LPM may have allowed for more accurate evaluation of both LPM and disc positioning.
Wang et al. [23], in an electromyographic study, demonstrated that the SLPM stabilizes the disc and condyle, whereas the ILPM is primarily involved in mouth opening. A displaced disc that fails to reduce spontaneously may impair normal joint function. The resulting imbalance between the disc and condyle may lead to overactivation of the SLPM as a compensatory response. Yang et al. [20] reported that both SLPM and ILPM may undergo pathological changes in the presence of disc displacement.
Finden et al. [24] used MRI to examine pathological changes in the LPM in patients with disc displacement and found that signal intensity changes, particularly in the SLPM, may correlate with the severity of displacement. The researchers reported that increased T2 and T1 signal intensity at the superior end of the LPM correlated with the severity of disc displacement, suggesting the presence of edema and fatty degeneration. However, the relationship between ILPM and disc position has often been neglected. Cabuk et al. [25], in an MRI study, suggested that both heads may be affected by changes in disc position.
In our study, the relationship between LPM attachment types and TMJ disc position was not statistically significant, consistent with the findings of Taskaya-Yılmaz et al. [4], Dergin et al. [8], Imanimoghaddam et al. [9], and Omami et al. [10].
In addition to LPM attachment patterns and disc position, several other variables—including joint effusion, degenerative joint changes, restricted motion, and morphological characteristics—may significantly impact TMJ pathology. Joint effusion, visible on T2-weighted MRI, is frequently associated with symptomatic disc displacement and TMJ pain [26, 27]. Degenerative changes such as osteoarthrosis are often observed concurrently with disc displacement and can exacerbate TMJ symptoms [28, 29]. Restricted mandibular motion, such as limited mouth opening, is another common clinical manifestation of internal derangement, reflecting functional impairment [30]. Morphological features like condylar remodeling or altered joint contours may further influence joint biomechanics and the progression of TMJ disorders.
Furthermore, the excessive and prolonged contraction of the LPM may be attributed to various etiological factors, irrespective of anatomical variations. Habits such as a prone sleeping position, which places continuous stress on the masticatory muscles and the TMJ, or prolonged dental treatments that require the mouth to be held open for extended periods, can lead to muscle overactivity and contribute to TMJ symptomatology [31, 32]. Moreover, the clinical significance of pain and tenderness in the lateral pterygoid muscle extends beyond its association with disc displacement. Tenderness of the LPM is a common finding in patients with TMDs and is frequently correlated with pain and limited mouth opening. This finding can serve as an important indicator of a muscle-related TMD, even in the absence of a confirmed disc displacement diagnosis [33]. Future prospective studies incorporating these additional variables would provide a more comprehensive understanding of the multifactorial etiology of disc displacement.
Considering this alternative perspectives, it may be hypothesized that the attachment type could play a contributory role in the persistence of disc displacement once triggered by other etiological factors (e.g., trauma, parafunctional habits, internal derangements). Indeed, Wongwatana et al. [34] suggested that as long as the joint structure remains normal, the type of muscular attachment does not play a decisive role in disc displacement. They reported that the superior head of the LPM may contribute to anteromedial disc displacement only in cases where preexisting damage to the disc—such as stretching and/or tearing of its lateral or posterior attachments—has occurred. Similarly, Tanaka et al. [35], using a mathematical model, demonstrated that hyperactivity of the LPM during clenching could contribute to the progression of disc displacement.
In our study, intra-articular changes such as thinned discs and elongation of retrodiscal tissues were observed in MR images of joints with disc displacement. Taken together, these findings suggest that the anatomy of the LPM may not directly determine disc position, but rather contribute as part of a complex interplay of functional and biomechanical factors. To further elucidate this relationship, future studies incorporating functional imaging and longitudinal follow-up are warranted, as the LPM could potentially be targeted for therapeutic interventions, thereby improving the management of this disorder. Understanding the relationship between LPM attachment types and disc displacement may help guide such treatment approaches. Furthermore, studies correlating TMJ and LPM MR images obtained from different planes with clinical findings are recommended to advance our understanding of the pathomechanism of TMJ disorders.
Additionally, although the Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) were not applied in our study due to its retrospective and imaging-based design, our findings provide valuable contributions into the anatomical relationship between LPM attachment types and disc displacement. Nevertheless, future prospective studies that simultaneously evaluate both RDC/TMD diagnostic criteria and MRI findings may help to better elucidate the multifactorial nature of TMJ disorders and further clarify the role of the LPM in their etiopathogenesis.
This study has certain limitations. First, a control group consisting of asymptomatic individuals was not included, as all participants presented with TMJ complaints. Future studies including asymptomatic controls are recommended to improve the reliability of the findings. Second, the use of 2 mm slice thickness, which may introduce partial volume averaging and obscure fine anatomical details of the LPM attachments or TMJ disc. However, this slice thickness is consistent with widely used TMJ MRI protocols in the literature, and multiplanar evaluation was performed to reduce misclassification risk. Additionally, variations in signal quality and the lack of a dedicated TMJ coil may have reduced the accuracy and resolution of the obtained images. Imaging angulation may also have influenced the visualization of the LPM and articular disc. Future studies employing higher-resolution imaging, optimized coil selection, and standardized angulation protocols may help overcome these limitations and provide more reliable results.