To explore the interplay among OSA severity, hypoxia, and cardiac circulatory function, we examined associations among sleep disorder indices, oximetry-related parameters, and the LVEF across OSA severity levels. Results indicated that despite comparable baseline characteristics and comorbidities, the severe OSA group exhibited significantly lower LVEF, alongside higher AHI and ODI values compared to the mild-to-moderate OSA group. Although not statistically significant, the severe OSA group demonstrated a trend toward lower LFCT. These findings indicated an inverse relationship between the event frequency and desaturation duration. Notably, the novel composite index, RERTA, was significantly elevated in the severe OSA group compared to the mild-to-moderate OSA group. A multivariable linear regression analysis further revealed a significant inverse association between the RERTA and LVEF, independent of age, sex, and BMI.
The severe OSA group demonstrated significantly lower LVEF values compared to the mild-to-moderate group. Several underlying mechanisms may account for this result, including an alteration in the cardiac structure, generation of reactive oxygen species, and activation of the sympathetic nervous system. For instance, previous research demonstrated that OSA-related intermittent hypoxia is linked to endothelial dysfunction and higher oxidative stress [22, 23], predisposing one to compromised cardiac output and reduced circulatory efficiency [24]. Next, intermittent hypoxia activates the sympathetic nervous system, contributing to peripheral vasoconstriction, and an elevated heart rate and blood pressure, thereby deteriorating cardiac health [25]. Several studies indicated that sympathetic overactivity is linked to increased risks of cardiovascular pathologies, such as arterial stiffness and arrhythmias [26, 27]. Overall, the current findings underscore the complex interplay between the respiratory event frequency and physiological compensation in OSA, reinforcing its association with cardiac dysfunction.
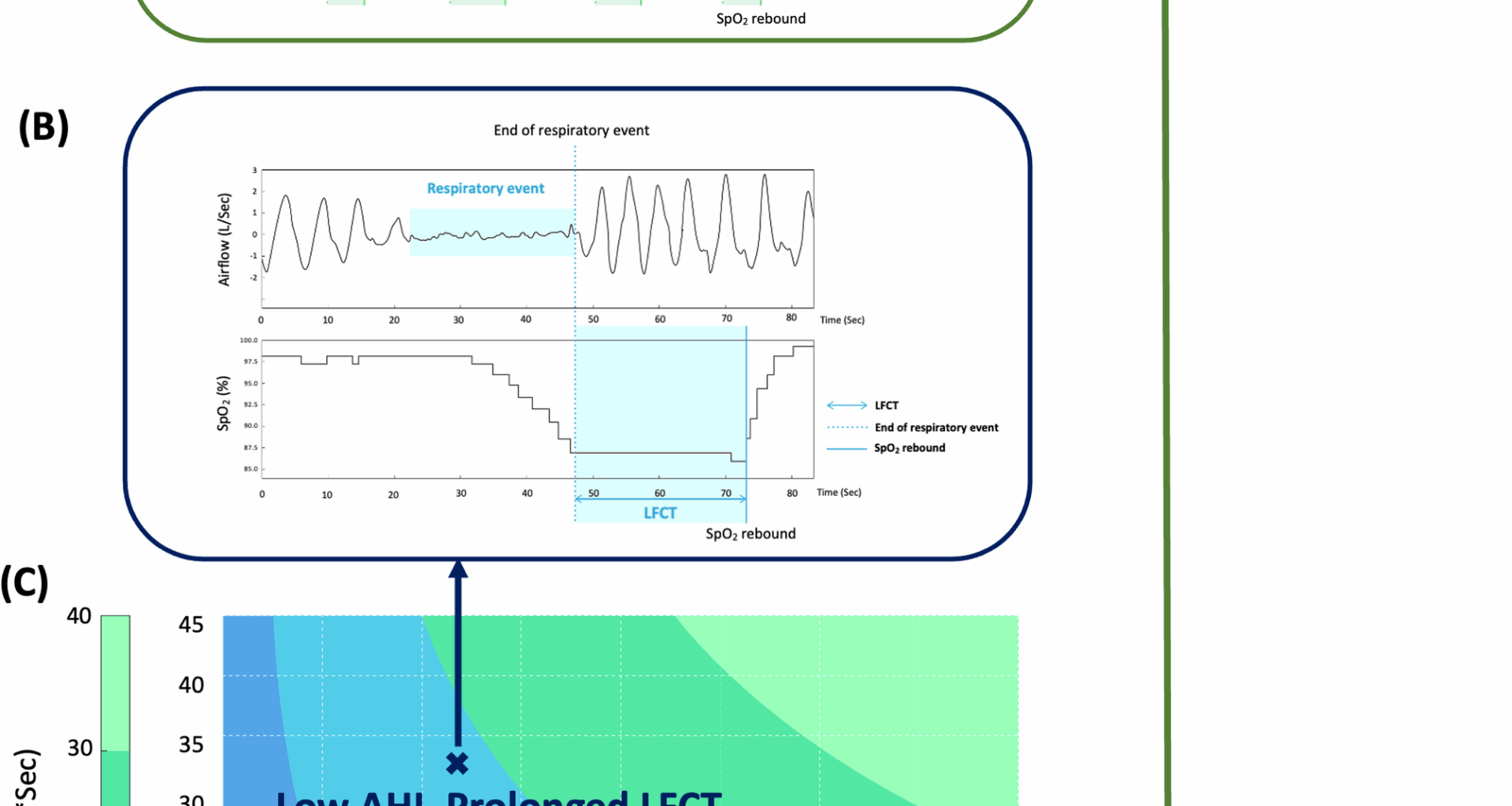
The LFCT, which primarily reflects the duration of responding to and accommodating hypoxia, serves as a crucial indicator for evaluating cardiac function in patients with OSA. A trend toward a lower LFCT in the severe OSA group suggests a potential inverse relationship with the AHI. Despite no direct evidence, several reasons may explain this finding. First, as aforementioned, intermittent hypoxia induces excessive sympathetic activation, leading to vasoconstriction, tachycardia, and elevated blood pressure and potentially shortens the LFCT [28]. Second, previous studies demonstrated that a higher hypoxic frequency reduces the baroreflex gain and increases the heart rate, potentially leading to a shorter LFCT [29, 30]. Additionally, a prior study reported that a prolonged LFCT was strongly associated with longer respiratory events, which may in turn reduce the event frequency [31]. While a shortened LFCT reflects an enhanced compensatory response to hypoxia, an increased AHI may contribute to progressive cardiac deterioration. Therefore, these findings underscore the potential of integrating both parameters for cardiovascular risk assessments in patients with OSA.
To comprehensively evaluate the reciprocal dynamics between the LFCT and AHI and their impacts on cardiac function in OSA, the RERTA metric was introduced. Furthermore, to contextualize the clinical feasibility of this novel metric, cutoff values for the RERTA, AHI, and LFCT in classifying the LVEF at the 60% threshold are provided in the Supplementary materials. The severe OSA group exhibited significantly higher mean RERTA values compared to the mild-to-moderate OSA group. Multivariable linear regression models revealed a significant inverse association between the RERTA and LVEF, independent of age, gender, and BMI. Similar results were observed after adjusting for age, gender, and height (Supplementary materials). Given the relatively high mean LVEF (>60%) and small sample size, the modest coefficient may indicate subclinical cardiac impairment. In this cohort, the severe OSA group exhibited a significantly lower LVEF compared to the mild-to-moderate group, suggesting that greater OSA severity may be associated with early declines in cardiac function, even within the normal LVEF range. Previous studies reported an increased risk of stroke and all-cause death among individuals with an LVEF lower than 60%, emphasizing the clinical importance of detecting early functional changes within the normal LVEF range [32, 33]. The geometric mean used to calculate the RERTA captures the cumulative area under the oxygen desaturation curve from all respiratory events, potentially reflecting the hypoxic burden in individuals with OSA [34]. One previous study also demonstrated the utility of geometric mean principles in cardiovascular risk assessments, improving the predictive accuracy by integrating various cardiovascular risk factors [35]. Additionally, an increased hypoxic burden is associated with elevated blood pressure, greater cardiovascular event risks, and all-cause mortality [36, 37]. Collectively, these findings suggest that the RERTA may serve as a clinically relevant indicator for identifying individuals with OSA at increased risk of cardiac dysfunction, highlighting its potential role in risk stratification and guiding clinical decision-making.
The main strength of this study is the introduction of the novel composite RERTA metric, which integrates the AHI (event frequency) and LFCT (desaturation duration) to comprehensively evaluate the impact of OSA on cardiac function. This dual-index approach addresses limitations of relying on a single metric, offering a broader perspective for assessing circulatory stress and cardiovascular risks. The significant inverse association between the RERTA and LVEF further supports its potential as a clinically relevant tool. Additionally, the use of the geometric mean methodology reinforces the utility of mathematically integrating physiological variables into a stable and informative index, in line with prior research. Therefore, these findings provide insights into the assessment of the hypoxic burden and cumulative impacts of the respiratory event frequency and desaturation duration on cardiac function in patients with OSA.
There are several limitations to this study. First, the relatively small sample size (n = 34), predominance of participants with severe OSA, and retrospective design may have introduced bias, thereby limiting both the statistical power and generalizability of the current findings. Future prospective studies in larger, independent cohorts are warranted to strengthen the robustness and clinical applicability of the RERTA index. Second, although individuals with acute cerebrovascular and cardiovascular events were excluded, cardiac function assessments solely relied on echocardiography, and the time gap of up to 6 months between the PSG and cardiac evaluations may have led to potential variability in cardiac function. The absence of nocturnal cardiac monitoring may have reduced the precision in capturing hypoxia-related effects. Additionally, given that the mean LVEF exceeded 60% and the majority of participants in both groups had severe OSA, the findings might not be generalizable to populations with reduced LVEF or those with mild to moderate OSA. Future studies should include more-heterogeneous cohorts with a wider range of cardiac phenotypes and OSA severity levels, and should incorporate nocturnal cardiac monitoring, to improve the validity and clinical feasibility of the current results. Third, despite adherence to AASM guidelines, variability in PSG and echocardiography interpretation could have affected the consistency. Future research should adopt automated and standardized scoring systems to improve the data accuracy and consistency. Finally, although the linear regression analyses adjusted for age, sex, and BMI, unmeasured confounders such as lifestyle factors (e.g., smoking, alcohol consumption, and physical activity), use of cardiac medications, socioeconomic status, and baseline cardiopulmonary health may have influenced the results. Future studies could also consider height as an independent confounder. Additionally, non-linear associations between the RERTA and cardiac function were not explored in the present study, which may limit the interpretation of its full clinical relevance. Future research should incorporate non-linear modeling and adjust for additional covariates to enhance the external validity and applicability of the RERTA.