Rochwerg B, Brochard L, Elliott MW, et al. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017;50:1602426.
Bellani G, Laffey JG, Pham T, et al. Noninvasive ventilation of patients with acute respiratory distress syndrome. Insights from the LUNG SAFE study. Am J Respir Crit Care Med. 2017;195:67–77.
Rezoagli E, Magliocca A, Bellani G, Pesenti A, Grasselli G. Development of a critical care response – experiences from Italy during the coronavirus disease 2019 pandemic. Anesthesiol Clin. 2021;39:265–84.
RISC-19-ICU, Investigators W, Garcia PD, Aguirre-Bermeo H, et al. Implications of early respiratory support strategies on disease progression in critical COVID-19: a matched subanalysis of the prospective RISC-19-ICU cohort. Crit Care. 2021;25:175.
Bellani G, Grasselli G, Cecconi M, et al. Noninvasive ventilatory support of patients with COVID-19 outside the intensive care units (WARd-COVID). Ann Am Thorac Soc. 2021;18:1020–6.
Bazuaye EA, Stone TN, Corris PA, Gibson GJ. Variability of inspired oxygen concentration with nasal cannulas. Thorax. 1992;47:609–11.
Coudroy R, Frat J-P, Girault C, Thille AW. Reliability of methods to estimate the fraction of inspired oxygen in patients with acute respiratory failure breathing through non-rebreather reservoir bag oxygen mask. Thorax. 2020;75:805–7.
Chanques G, Constantin J-M, Sauter M, et al. Discomfort associated with underhumidified high-flow oxygen therapy in critically ill patients. Intensive Care Med. 2009;35:996–1003.
for the REVA Network, Poiroux L, Piquilloud L, et al. Effect on comfort of administering bubble-humidified or dry oxygen: the oxyrea non-inferiority randomized study. Ann Intensive Care. 2018;8:126.
Papazian L, Corley A, Hess D, et al. Use of high-flow nasal cannula oxygenation in ICU adults: a narrative review. Intensive Care Med. 2016;42:1336–49.
Grieco DL, Maggiore SM, Roca O, et al. Non-invasive ventilatory support and high-flow nasal oxygen as first-line treatment of acute hypoxemic respiratory failure and ARDS. Intensive Care Med. 2021;47:851–66.
Goligher EC, Slutsky AS. Not just oxygen? Mechanisms of benefit from high-flow nasal cannula in hypoxemic respiratory failure. Am J Respir Crit Care Med. 2017;195:1128–31.
Chanques G, Riboulet F, Molinari N, et al. Comparison of three high flow oxygen therapy delivery devices: a clinical physiological cross-over study. Minerva Anestesiol. 2013;79:1344–55.
Wagstaff TAJ, Soni N. Performance of six types of oxygen delivery devices at varying respiratory rates*. Anaesthesia. 2007;62:492–503.
Parke RL, Eccleston ML, McGuinness SP. The effects of flow on airway pressure during nasal High-Flow oxygen therapy. Respir Care. 2011;56:1151–5.
Parke RL, McGuinness SP. Pressures delivered by nasal high flow oxygen during all phases of the respiratory cycle. Respir Care. 2013;58:1621–4.
Corley A, Caruana LR, Barnett AG, Tronstad O, Fraser JF. Oxygen delivery through high-flow nasal cannulae increase end-expiratory lung volume and reduce respiratory rate in post-cardiac surgical patients. Br J Anaesth. 2011;107:998–1004.
Mauri T, Turrini C, Eronia N, et al. Physiologic effects of high-flow nasal cannula in acute hypoxemic respiratory failure. Am J Respir Crit Care Med. 2017;195:1207–15.
Roca O, Riera J, Torres F, Masclans JR. High-flow oxygen therapy in acute respiratory failure. Respir Care. 2010;55:408–13.
Dewan NA, Bell CW. Effect of low flow and high flow oxygen delivery on exercise tolerance and sensation of dyspnea. Chest. 1994;105:1061–5.
Sztrymf B, Messika J, Mayot T, Lenglet H, Dreyfuss D, Ricard J-D. Impact of high-flow nasal cannula oxygen therapy on intensive care unit patients with acute respiratory failure: a prospective observational study. J Crit Care. 2012;27:e3249–32413.
Mauri T, Alban L, Turrini C, et al. Optimum support by high-flow nasal cannula in acute hypoxemic respiratory failure: effects of increasing flow rates. Intensive Care Med. 2017;43:1453–63.
Pinkham M, Tatkov S. Effect of flow and cannula size on generated pressure during nasal high flow. Crit Care. 2020;24:248.
Zhao E, Zhou Y, He C, Ma D. Factors influencing nasal airway pressure and comfort in high-flow nasal cannula oxygen therapy: a volunteer study. BMC Pulm Med. 2023;23:449.
Onodera Y, Akimoto R, Suzuki H, Masaki N, Kawamae K. A high-flow nasal cannula system set at relatively low flow effectively washes out CO2 from the anatomical dead space of a respiratory-system model. Korean J Anesthesiol. 2017;70:105.
Tatkov S, Rees M, Gulley A, Van Den Heuij LGT. Nilius G: Bernanrd. J Appl Physiol. 2023;134:365–77.
Slobod D, Spinelli E, Crotti S, et al. Effects of an asymmetrical high flow nasal cannula interface in hypoxemic patients. Crit Care. 2023;27:145.
Boscolo A, Pettenuzzo T, Zarantonello F, et al. Asymmetrical high-flow nasal cannula performs similarly to standard interface in patients with acute hypoxemic post-extubation respiratory failure: a pilot study. BMC Pulm Med. 2024;24:21.
Mauri T, Galazzi A, Binda F, et al. Impact of flow and temperature on patient comfort during respiratory support by high-flow nasal cannula. Crit Care. 2018;22:120.
Bongiovanni F, Grieco DL, Anzellotti GM, et al. Gas conditioning during helmet noninvasive ventilation: effect on comfort, gas exchange, inspiratory effort, transpulmonary pressure and patient–ventilator interaction. Ann Intensive Care. 2021;11(1):184 https://doi.org/10.1186/s13613-021-00972-9
De Beaufort E, Carteaux G, Morin F, et al. A new reservoir-based CPAP with low oxygen consumption: the bag-CPAP. Crit Care. 2023;27:262.
Perkins GD, Ji C, Connolly BA, et al. Effect of noninvasive respiratory strategies on intubation or mortality among patients with acute hypoxemic respiratory failure and COVID-19: the RECOVERY-RS randomized clinical trial. JAMA. 2022;327:546–58.
Alviset S, Riller Q, Aboab J, et al. Continuous positive airway pressure (CPAP) face-mask ventilation is an easy and cheap option to manage a massive influx of patients presenting acute respiratory failure during the SARS-CoV-2 outbreak: A retrospective cohort study. PLoS ONE Edited Den Uil C. 2020;15:e0240645.
Carteaux G, Pons M, Morin F, et al. Continuous positive airway pressure for respiratory support during COVID-19 pandemic: a frugal approach from bench to bedside. Ann Intensive Care. 2021;11:38.
Alviar CL, Miller PE, McAreavey D, et al. Positive pressure ventilation in the cardiac intensive care unit. J Am Coll Cardiol. 2018;72:1532–53.
L’Her E, Deye N, Lellouche F, et al. Physiologic effects of noninvasive ventilation during acute lung injury. Am J Respir Crit Care Med. 2005;172:1112–8.
Rezoagli E, Laffey JG, Bellani G. Monitoring lung injury severity and ventilation intensity during mechanical ventilation. Semin Respir Crit Care Med. 2022;43(3):346–68.
Ducros L, Logeart D, Vicaut E, et al. CPAP for acute cardiogenic pulmonary oedema from out-of-hospital to cardiac intensive care unit: a randomised multicentre study. Intensive Care Med. 2011;37:1501–9.
Guyton AC, Lindsey AW, Abernathy B, Richardson T. Venous return at various right atrial pressures and the normal venous return curve. American Journal of Physiology-Legacy Content. 1957;189:609–15.
Nanas S, Magder S. Adaptations of the peripheral circulation to PEEP. Am Rev Respir Dis. 1992;146:688–93.
Ashbaugh DG, Petty TL. Positive end-expiratory pressure. Physiology, indications, and contraindications. J Thorac Cardiovasc Surg. 1973;65:165–70.
Hopkins SR, Stickland MK. The pulmonary vasculature. Semin Respir Crit Care Med. 2023;44:538–54.
Luecke T, Pelosi P. Positive end-expiratory pressure and cardiac output. Crit Care. 2005;9:607.
Lenique F, Habis M, Lofaso F, Dubois-Randé JL, Harf A, Brochard L. Ventilatory and hemodynamic effects of continuous positive airway pressure in left heart failure. Am J Respir Crit Care Med. 1997;155:500–5.
Buda AJ, Pinsky MR, Ingels NB, Daughters GT, Stinson EB, Alderman EL. Effect of intrathoracic pressure on left ventricular performance. N Engl J Med. 1979;301:453–9.
Bradley TD, Holloway RM, McLaughlin PR, Ross BL, Walters J, Liu PP. Cardiac output response to continuous positive airway pressure in congestive heart failure. Am Rev Respir Dis. 1992;145:377–82.
Bernard GR, Pou NA, Coggeshall JW, Carroll FE, Snapper JR. Comparison of the pulmonary dysfunction caused by cardiogenic and noncardiogenic pulmonary edema. Chest. 1995;108:798–803.
Taccone P, Hess D, Caironi P, Bigatello LM. Continuous positive airway pressure delivered with a helmet: effects on carbon dioxide rebreathing*. Crit Care Med. 2004;32:2090–6.
Bradley MN, Mcarthur KT, Lyons C. An oxygen head tent for hypoxia. Ann Surg. 1964;159:683–9.
Giani M, Fumagalli B, Cipulli F, et al. The ZEEP-PEEP test to evaluate the response to positive end-expiratory pressure delivered by helmet: a prospective physiologic study. Heliyon. 2024;10:e28339.
Menga LS, Delle Cese L, Rosà T, et al. Respective effects of helmet pressure support, continuous positive airway pressure, and nasal high-flow in hypoxemic respiratory failure: a randomized crossover clinical trial. Am J Respir Crit Care Med. 2023;207:1310–23.
Yoshida T, Torsani V, Gomes S, et al. Spontaneous effort causes occult pendelluft during mechanical ventilation. Am J Respir Crit Care Med. 2013;188:1420–7.
Yoshida T, Amato MBP, Kavanagh BP. Understanding spontaneous vs. ventilator breaths: impact and monitoring. Intensive Care Med. 2018;44:2235–8.
Tonelli R, Fantini R, Tabbì L, et al. Early inspiratory effort assessment by esophageal manometry predicts noninvasive ventilation outcome in de novo respiratory failure. A pilot study. Am J Respir Crit Care Med. 2020;202:558–67.
Tonelli R, Bruzzi G, Manicardi L, et al. Risk factors for pulmonary air leak and clinical prognosis in patients with COVID-19 related acute respiratory failure: a retrospective matched control study. Front Med. 2022;9:848639.
Junhasavasdikul D, Telias I, Grieco DL, et al. Expiratory flow limitation during mechanical ventilation. Chest. 2018;154:948–62.
for the VENTILAB group, Natalini G, Tuzzo D, et al. Effect of external PEEP in patients under controlled mechanical ventilation with an auto-PEEP of 5 cmH2O or higher. Ann Intensive Care. 2016;6:53.
Caramez MP, Borges JB, Tucci MR, et al. Paradoxical responses to positive end-expiratory pressure in patients with airway obstruction during controlled ventilation*. Crit Care Med. 2005;33:1519–28.
Rezoagli E, Pozzi M, Cereda M, Foti G. Overestimation of driving pressure by the analysis of the conductive pressure during venous-arterial ECMO: airway closure or intrinsic PEEP? Crit Care. 2023;27:497.
Brochard L. Intrinsic (or auto-) positive end-expiratory pressure during spontaneous or assisted ventilation. Intensive Care Med. 2002;28:1552–4.
Plens GM, Droghi MT, Alcala GC, et al. Expiratory muscle activity counteracts positive end-expiratory pressure and is associated with Fentanyl dose in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2024;209:563–72.
Pankow W, Podszus T, Gutheil T, Penzel T, Peter J-H, Von Wichert P. Expiratory flow limitation and intrinsic positive end-expiratory pressure in obesity. J Appl Physiol. 1998;85:1236–43.
Nova A, Xin Y, Victor M, et al. Biomechanical implications of mass loading in a swine model of acute hypoxemic respiratory failure. J Appl Physiol. 2025(3). https://doi.org/10.1152/japplphysiol.00377.2025.
Behazin N, Jones SB, Cohen RI, Loring SH. Respiratory restriction and elevated pleural and esophageal pressures in morbid obesity. J Appl Physiol. 2010;108(1):212–8.
Fumagalli J, Santiago RRS, Teggia Droghi M, et al. Lung recruitment in obese patients with acute respiratory distress syndrome. Anesthesiology. 2019;130:791–803.
Nicolini A, Ferrando M, Solidoro P, Di Marco F, Facchini F, Braido F. Non-invasive ventilation in acute respiratory failure of patients with obesity hypoventilation syndrome. Minerva Med. 2018;109(6 Suppl 1):1-5. https://doi.org/10.23736/S0026-4806.18.05921-9.
Florio G, De Santis Santiago RR, Fumagalli J, et al. Pleural pressure targeted positive airway pressure improves cardiopulmonary function in spontaneously breathing patients with obesity. Chest. 2021;159:2373–83.
Longhini F, Bruni A, Garofalo E, et al. Monitoring the patient–ventilator asynchrony during non-invasive ventilation. Front Med. 2023;9:1119924.
Carteaux G, Lyazidi A, Cordoba-Izquierdo A, et al. Patient-ventilator asynchrony during noninvasive ventilation. Chest. 2012;142:367–76.
Calderini E, Confalonieri M, Puccio PG, Francavilla N, Stella L, Gregoretti C. Patient-ventilator asynchrony during noninvasive ventilation: the role of expiratory trigger. Intensive Care Med. 1999;25:662–7.
Fontanari P, Burnet H, Zattara-Hartmann MC, Jammes Y. Changes in airway resistance induced by nasal inhalation of cold dry, dry, or moist air in normal individuals. J Appl Physiol. 1996;81:1739–43.
Iotti GA, Olivei MC, Braschi A. [No title found]. Crit Care. 1999;3:R77.
Ploysongsang Y, Branson R, Rashkin MC, Hurst JM. Pressure flow characteristics of commonly used heat-moisture exchangers. Am Rev Respir Dis. 1988;138:675–8.
Lellouche F, Pignataro C, Maggiore SM, et al. Short-term effects of humidification devices on respiratory pattern and arterial blood gases during noninvasive ventilation. Respir Care. 2012;57:1879–86.
Lellouche F, Maggiore SM, Deye N, et al. Effect of the humidification device on the work of breathing during noninvasive ventilation. Intensive Care Med. 2002;28:1582–9.
Lellouche F, L’Her E, Abroug F, et al. Impact of the humidification device on intubation rate during noninvasive ventilation with ICU ventilators: results of a multicenter randomized controlled trial. Intensive Care Med. 2014;40:211–9.
Restrepo RD, Walsh BK. Humidification during invasive and noninvasive mechanical ventilation: 2012. Respir Care. 2012;57:782–8.
Lucchini A, Valsecchi D, Elli S, et al. [The comfort of patients ventilated with the helmet Bundle]. Assist Inferm Ric. 2010;29:174–83.
Ambrosetti L, Giani M, Rezoagli E, et al. Gas humidification during helmet continuous positive airway pressure: a crossover randomized physiologic study in healthy subjects. Dimens Crit Care Nurs. 2024;43:21–7.
American National Standards Institute, American Society of Anesthesiologists. American National standard for humidifiers and nebulizers for medical use. New York: The Institute; 1979.
Esquinas Rodriguez AM, Scala R, Soroksky A, et al. Clinical review: humidifiers during non-invasive ventilation – key topics and practical implications. Crit Care. 2011;16:203.
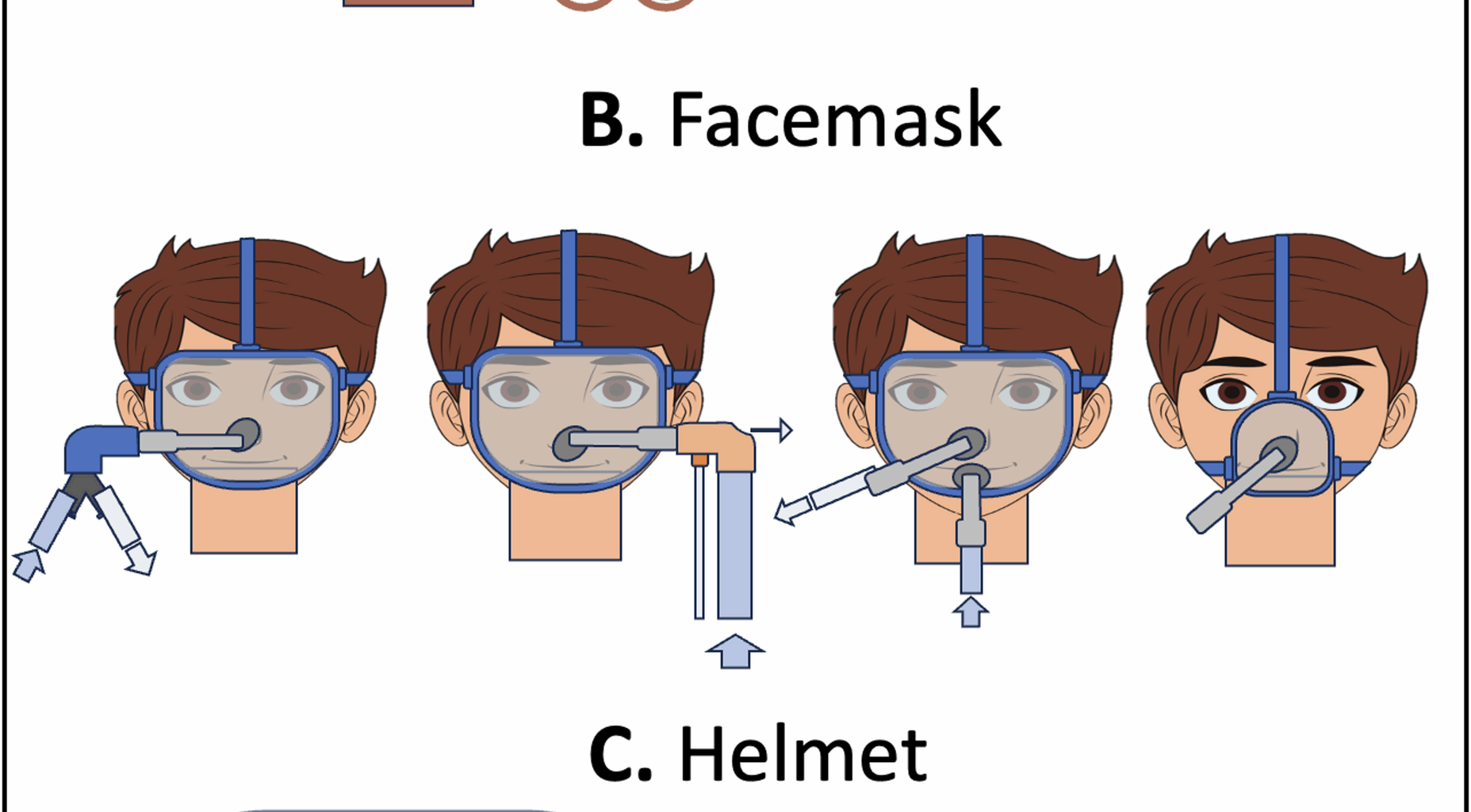
Tarabini Fraticelli A, Lellouche F, L’Her E, Taillé S, Mancebo J, Brochard L. Physiological effects of different interfaces during noninvasive ventilation for acute respiratory failure*. Crit Care Med. 2009;37:939–45.
Gregoretti C, Confalonieri M, Navalesi P, et al. Evaluation of patient skin breakdown and comfort with a new face mask for non-invasive ventilation: a multi-center study. Intensive Care Med. 2002;28:278–84.
Antón A, Tárrega J, Giner J, Güell R, Sanchis J. Acute physiologic effects of nasal and full-face masks during noninvasive positive-pressure ventilation in patients with acute exacerbations of chronic obstructive pulmonary disease. Respir Care. 2003;48:922–5.
Saatci E, Miller DM, Stell IM, Lee KC, Moxham J. Dynamic dead space in face masks used with noninvasive ventilators: a lung model study. Eur Respir J. 2004;23:129–35.
Lofaso F, Brochard L, Touchard D, Hang T, Harf A, Isabey D. Evaluation of carbon dioxide rebreathing during pressure support ventilation with airway management system (BiPAP) devices. Chest. 1995;108:772–8.
Nava S, Navalesi P, Gregoretti C. Interfaces and humidification for noninvasive mechanical ventilation. Respir Care. 2009;54:71–84.
Scala R. Bi-level home ventilators for Non invasive positive pressure ventilation. Monaldi Arch Chest Dis. 2004;61(4):213-21. https://doi.org/10.4081/monaldi.2004.684
Schettino GPP, Chatmongkolchart S, Hess DR, Kacmarek RM. Position of exhalation port and mask design affect CO2 rebreathing during noninvasive positive pressure ventilation*. Crit Care Med. 2003;31:2178–82.
Ferguson GT, Gilmartin M. CO2 rebreathing during BiPAP® ventilatory assistance. Am J Respir Crit Care Med. 1995;151:1126–35.
Rezoagli E, Signori D, Grassi A, et al. A novel mask with selective ports for inflow and outflow reduces CO2 rebreathing during non-invasive ventilation: a physiological study in healthy volunteers. Respiration. 2023;102(1):1–11.
Signori D, Bellani G, Calcinati S, Grassi A, Patroniti N, Foti G. Effect of face mask design and bias flow on rebreathing during noninvasive ventilation. Respir Care. 2019;64:793–800.
Grieco DL, Menga LS, Raggi V, et al. Physiological comparison of high-flow nasal cannula and helmet noninvasive ventilation in acute hypoxemic respiratory failure. Am J Respir Crit Care Med. 2020;201:303–12.
Blanco M, Jaritos V, Ernst G, Salvado A, Nogueira F, Borsini E. Patients’ preferences and the efficacy of a hybrid model of a minimal contact nasal mask in patients with sleep apnea treated with CPAP. Sleep Sci. 2018;11:254–9.
Patroniti N, Foti G, Manfio A, Coppo A, Bellani G, Pesenti A. Head helmet versus face mask for non-invasive continuous positive airway pressure: a physiological study. Intensive Care Med. 2003;29:1680–7.
Coppadoro A, Zago E, Pavan F, Foti G, Bellani G. The use of head helmets to deliver noninvasive ventilatory support: a comprehensive review of technical aspects and clinical findings. Crit Care. 2021;25:327.
Isgrò S, Zanella A, Giani M, Abd El Aziz El Sayed, Deab S, Pesenti A, Patroniti N. Performance of different PEEP valves and helmet outlets at increasing gas flow rates: a bench top study. Minerva Anestesiol. 2012;78:1095–100.
Rezoagli E, Coppola G, Dezza L, et al. High efficiency particulate air filters and heat & moisture exchanger filters increase positive end-expiratory pressure in helmet continuous positive airway pressure: A bench-top study. Pulmonology. 2024;30:8–16.
Coppadoro A, Fracchia R, Nova A, et al. Not too much, not too little. Titrating flow rate to minimise inspiratory effort during helmet CPAP: a bench study. Pulmonology. 2025;31:2411804.
Bshouty ZH, Roeseier J, Reynaert MS, Rodenstein D. The importance of the balloon reservoir volume of a CPAP system in reducing the work of breathing. Intensive Care Med. 1986;12(3):153-6. https://doi.org/10.1007/BF00254931.
Roeseler J, Bshouty ZH, Reynaert MS. The importance of the circuit capacity in the administration of CPAP. Intensive Care Med. 1984;10(6):305-308. https://doi.org/10.1007/BF00254321.
Braschi A, Iotti G, Locatelli A, Bellinzona G. Functional evaluation of a CPAP circuit with a high compliance reservoir bag. Intensive Care Med. 1985;11:85–9.
Poulton TJ, Downs JB. Humidification of rapidly flowing gas. Crit Care Med. 1981;9:59–63.
Kacmarek RM, Dimas S, Reynolds J, Shapiro BA. Technical aspects of positive end-expiratory pressure (PEEP): part II. PEEP with positive-pressure ventilation. Respir Care. 1982;27:1490–504.
Lucchini A, Giani M, Minotti D, Elli S, Bambi S. Helmet CPAP bundle: a narrative review of practical aspects and nursing interventions to improve patient’s comfort. Intensive Crit Care Nurs. 2023;74:103335.
Lucchini A, Elli S, Bambi S, et al. How different helmet fixing options could affect patients’ pain experience during helmet-continuous positive airway pressure. Nurs Crit Care. 2019;24:369–74.
Chiumello D, Chierichetti M, Tallarini F, et al. Effect of a heated humidifier during continuous positive airway pressure delivered by a helmet. Crit Care. 2008;12:R55.
Duan J, Liu X, Shu W, et al. Low versus high positive end expiratory pressure in noninvasive ventilation for hypoxemic respiratory failure: a multicenter randomized controlled trial. Intensive Care Med. 2025;51:861–9.
Grieco DL, Patel BK, Antonelli M. Helmet noninvasive support in hypoxemic respiratory failure. Intensive Care Med. 2022;48:1072–5.
Vaschetto R, De Jong A, Conseil M, et al. Comparative evaluation of three interfaces for non-invasive ventilation: a randomized cross-over design physiologic study on healthy volunteers. Crit Care. 2014;18:R2.
Haudebourg A-F, Maraffi T, Tuffet S, Le Corvoisier P, Mekontso Dessap A, Carteaux G. Influence of different noninvasive oxygenation support devices on tidal volume. Ann Intensive Care. 2023;13:116.
Olivieri C, Costa R, Spinazzola G, et al. Bench comparative evaluation of a new generation and standard helmet for delivering non-invasive ventilation. Intensive Care Med. 2013;39:734–8.
Olivieri C, Longhini F, Cena T, et al. New versus conventional helmet for delivering noninvasive ventilation. Anesthesiology. 2016;124:101–8.
Cesarano M, Grieco DL, Michi T, et al. Helmet noninvasive support for acute hypoxemic respiratory failure: rationale, mechanism of action and bedside application. Ann Intensive Care. 2022;12:94.
Pisani L, Mega C, Vaschetto R, et al. Oronasal mask versus helmet in acute hypercapnic respiratory failure. Eur Respir J. 2015;45:691–9.
Vargas F, Thille A, Lyazidi A, Master BE, Roche Campo F, Brochard L. Helmet with specific settings versus facemask for noninvasive ventilation*. Crit Care Med. 2009;37:1921–8.
Berbenetz N, Wang Y, Brown J, et al. Non-invasive positive pressure ventilation (CPAP or bilevel NPPV) for cardiogenic pulmonary oedema. Cochrane Database Syst Rev. 2019;4:CD005351.
Masip J, Peacock WF, Price S, et al. Indications and practical approach to non-invasive ventilation in acute heart failure. Eur Heart J. 2018;39:17–25.
Gray A, Goodacre S, Newby DE, et al. Noninvasive ventilation in acute cardiogenic pulmonary edema. N Engl J Med. 2008;359:142–51.
Mehta S, Jay GD, Woolard RH, et al. Randomized, prospective trial of bilevel versus continuous positive airway pressure in acute pulmonary edema. Crit Care Med. 1997;25:620.
Bellone A, Monari A, Cortellaro F, Vettorello M, Arlati S, Coen D. Myocardial infarction rate in acute pulmonary edema: noninvasive pressure support ventilation versus continuous positive airway pressure. Crit Care Med. 2004;32:1860–5.
Moritz F, Brousse B, Gellée B, et al. Continuous positive airway pressure versus bilevel noninvasive ventilation in acute cardiogenic pulmonary edema: a randomized multicenter trial. Ann Emerg Med. 2007;50:666–75. 675.e1.
Liesching T, Nelson DL, Cormier KL. Randomized trial of bilevel versus continuous positive airway pressure for acute pulmonary edema. J Emerg Med. 2014;46:130–40.
Makdee O, Monsomboon A, Surabenjawong U, et al. High-Flow nasal cannula versus conventional oxygen therapy in emergency department patients with cardiogenic pulmonary edema: A randomized controlled trial. Ann Emerg Med. 2017;70:465–e4722.
RENOVATE Investigators and the BRICNet, Authors, Francio F, Weigert RM, et al. High-Flow nasal oxygen vs noninvasive ventilation in patients with acute respiratory failure: the RENOVATE randomized clinical trial. JAMA. 2024. https://doi.org/10.1001/jama.2024.26244.
Osman A, Via G, Sallehuddin RM, et al. Helmet continuous positive airway pressure vs. high flow nasal cannula oxygen in acute cardiogenic pulmonary oedema: a randomized controlled trial. Eur Heart J Acute Cardiovasc Care. 2021;10:1103–11.
Frat J-P, Brugiere B, Ragot S, et al. Sequential application of oxygen therapy via high-flow nasal cannula and noninvasive ventilation in acute respiratory failure: an observational pilot study. Respir Care. 2015;60:170–8.
Plaisance P, Pirracchio R, Berton C, Vicaut E. A randomized study of out-of-hospital continuous positive airway pressure for acute cardiogenic pulmonary oedema: physiological and clinical effects. Eur Heart J. 2007;28:2895–901.
Foti G, Sangalli F, Berra L, et al. Is helmet CPAP first line pre-hospital treatment of presumed severe acute pulmonary edema? Intensive Care Med. 2009;35:656–62.
Frat J-P, Thille AW, Mercat A, et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. 2015;372:2185–96.
Andino R, Vega G, Pacheco SK, et al. High-flow nasal oxygen reduces endotracheal intubation: a randomized clinical trial. Ther Adv Respir Dis. 2020;14:1753466620956459.
Frat J-P, Quenot J-P, Badie J, et al. Carte JAMA. 2022;328:1212–22.
Bouadma L, Mekontso-Dessap A, Burdet C, et al. High-dose dexamethasone and oxygen support strategies in intensive care unit patients with severe COVID-19 acute hypoxemic respiratory failure: the COVIDICUS randomized clinical trial. JAMA Intern Med. 2022;182:906–16.
Crimi C, Noto A, Madotto F, et al. High-flow nasal oxygen versus conventional oxygen therapy in patients with COVID-19 pneumonia and mild hypoxaemia: a randomised controlled trial. Thorax. 2023;78:354–61.
Nazir N, Saxena A. The effectiveness of high-flow nasal cannula and standard non-rebreathing mask for oxygen therapy in moderate category COVID-19 pneumonia: randomised controlled trial. Afr J Thorac Crit Care Med. 2022;28(1):10.7196/AJTCCM.2022.v28i1.206. https://doi.org/10.7196/AJTCCM.2022.v28i1.206 .
Le Pape S, Savart S, Arrivé F, et al. High-flow nasal cannula oxygen versus conventional oxygen therapy for acute respiratory failure due to COVID-19: a systematic review and meta-analysis. Ann Intensive Care. 2023;13:114.
Azoulay E, Lemiale V, Mokart D, et al. Effect of high-flow nasal oxygen vs standard oxygen on 28-day mortality in immunocompromised patients with acute respiratory failure: the HIGH randomized clinical trial. JAMA. 2018;320(20):2099–107.
Coudroy R, Frat J-P, Ehrmann S, et al. High-flow nasal oxygen alone or alternating with non-invasive ventilation in critically ill immunocompromised patients with acute respiratory failure: a randomised controlled trial. Lancet Respir Med. 2022;10:641–9.
Delclaux C, L’Her E, Alberti C, et al. Treatment of acute hypoxemic nonhypercapnic respiratory insufficiency with continuous positive airway pressure delivered by a face mask: A randomized controlled trial. JAMA. 2000;284:2352.
Cosentini R, Brambilla AM, Aliberti S, et al. Helmet continuous positive airway pressure vs oxygen therapy to improve oxygenation in community-acquired pneumonia. Chest. 2010;138:114–20.
Squadrone V, Massaia M, Bruno B, et al. Early CPAP prevents evolution of acute lung injury in patients with hematologic malignancy. Intensive Care Med. 2010;36:1666–74.
Brambilla AM, Aliberti S, Prina E, et al. Helmet CPAP vs. oxygen therapy in severe hypoxemic respiratory failure due to pneumonia. Intensive Care Med. 2014;40:942–9.
Grasselli G, Calfee CS, Camporota L, et al. ESICM guidelines on acute respiratory distress syndrome: definition, phenotyping and respiratory support strategies. Intensive Care Med. 2023;49:727–59.
Ferrer M, Esquinas A, Leon M, Gonzalez G, Alarcon A, Torres A. Noninvasive ventilation in severe hypoxemic respiratory failure: a randomized clinical trial. Am J Respir Crit Care Med. 2003;168:1438–44.
Hilbert G, Gruson D, Vargas F, et al. Noninvasive ventilation in immunosuppressed patients with pulmonary infiltrates, fever, and acute respiratory failure. N Engl J Med. 2001;344:481–7.
Antonelli M, Conti G, Bufi M, et al. Noninvasive ventilation for treatment of acute respiratory failure in patients undergoing solid organ transplantation: a randomized trial. JAMA. 2000;283:235–41.
Martin TJ, Hovis JD, Costantino JP, et al. A randomized, prospective evaluation of noninvasive ventilation for acute respiratory failure. Am J Respir Crit Care Med. 2000;161:807–13.
Confalonieri M, Potena A, Carbone G, Porta RD, Tolley EA, Umberto Meduri G. Acute respiratory failure in patients with severe community-acquired pneumonia. A prospective randomized evaluation of noninvasive ventilation. Am J Respir Crit Care Med. 1999;160:1585–91.
Kramer N, Meyer TJ, Meharg J, Cece RD, Hill NS. Randomized, prospective trial of noninvasive positive pressure ventilation in acute respiratory failure. Am J Respir Crit Care Med. 1995;151:1799–806.
Zhan Q, Sun B, Liang L, et al. Early use of noninvasive positive pressure ventilation for acute lung injury: a multicenter randomized controlled trial. Crit Care Med. 2012;40:455–60.
Ferreyro BL, Angriman F, Munshi L, et al. Association of noninvasive oxygenation strategies with all-cause mortality in adults with acute hypoxemic respiratory failure: a systematic review and meta-analysis. JAMA. 2020;324:57.
Nair PR, Haritha D, Behera S, et al. Comparison of high-flow nasal cannula and noninvasive ventilation in acute hypoxemic respiratory failure due to severe COVID-19 pneumonia. Respir Care. 2021;66:1824–30.
Grieco DL, Menga LS, Cesarano M, et al. Effect of helmet noninvasive ventilation vs high-flow nasal oxygen on days free of respiratory support in patients with COVID-19 and moderate to severe hypoxemic respiratory failure: the HENIVOT randomized clinical trial. JAMA. 2021;325:1731–43.
Chaudhuri D, Jinah R, Burns KEA, et al. Helmet noninvasive ventilation compared to facemask noninvasive ventilation and high-flow nasal cannula in acute respiratory failure: a systematic review and meta-analysis. Eur Respir J. 2022;59:2101269.
Patel BK, Wolfe KS, Pohlman AS, Hall JB, Kress JP. Effect of noninvasive ventilation delivered by helmet vs face mask on the rate of endotracheal intubation in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. 2016;315:2435–41.
Arabi YM, Aldekhyl S, Al Qahtani S, et al. Effect of helmet noninvasive ventilation vs usual respiratory support on mortality among patients with acute hypoxemic respiratory failure due to COVID-19: the HELMET-COVID randomized clinical trial. JAMA. 2022;328:1063–72.
Collaborative Research Group of Noninvasive Mechanical Ventilation for Chronic Obstructive Pulmonary Disease. Early use of non-invasive positive pressure ventilation for acute exacerbations of chronic obstructive pulmonary disease: a multicentre randomized controlled trial. Chin Med J (Engl). 2005;118:2034–40.
Bott J, Carroll MP, Conway JH, et al. Randomised controlled trial of nasal ventilation in acute ventilatory failure due to chronic obstructive airways disease. Lancet. 1993;341:1555–7.
Brochard L, Mancebo J, Wysocki M, et al. Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease. N Engl J Med. 1995;333:817–22.
Carrera M, Marín JM, Antón A, et al. A controlled trial of noninvasive ventilation for chronic obstructive pulmonary disease exacerbations. J Crit Care. 2009;24:e4737–14.
Celikel T, Sungur M, Ceyhan B, Karakurt S. Comparison of noninvasive positive pressure ventilation with standard medical therapy in hypercapnic acute respiratory failure. Chest. 1998;114:1636–42.
Plant PK, Owen JL, Elliott MW. Early use of non-invasive ventilation for acute exacerbations of chronic obstructive pulmonary disease on general respiratory wards: a multicentre randomised controlled trial. Lancet. 2000;355:1931–5.
Thys F, Roeseler J, Reynaert M, Liistro G, Rodenstein DO. Noninvasive ventilation for acute respiratory failure: a prospective randomised placebo-controlled trial. Eur Respir J. 2002;20:545–55.
Conti G, Antonelli M, Navalesi P, et al. Noninvasive vs. conventional mechanical ventilation in patients with chronic obstructive pulmonary disease after failure of medical treatment in the ward: a randomized trial. Intensive Care Med. 2002;28:1701–7.
Jurjević M, Matić I, Sakić-Zdravcević K, Sakić S, Danić D, Buković D. Mechanical ventilation in chronic obstructive pulmonary disease patients, noninvasive vs. invasive method (randomized prospective study). Coll Antropol. 2009;33:791–7.
Li X-Y, Tang X, Wang R et al. High-Flow Nasal Cannula for Chronic Obstructive Pulmonary Disease with Acute Compensated Hypercapnic Respiratory Failure: A Randomized, Controlled Trial. COPD 2020; 15:3051–61<\/bib><\/p>
Fraser JF, Spooner AJ, Dunster KR, Anstey CM, Corley A Nasal high flow oxygen therapy in patients with COPD reduces respiratory rate and tissue carbon dioxide while increasing tidal and end-expiratory lung volumes: a randomised crossover trial. Thorax 2016; 71:759–61
Nagata K, Horie T, Chohnabayashi N, Home High-Flow Nasal Cannula Oxygen Therapy for Stable Hypercapnic COPD: A Randomized Clinical Trial. Am J Respir Crit Care Med. 2022;206(11):1326-35. https://doi.org/10.1164/rccm.202201-0199OC.
Xia J, Gu S, Lei W. High-flow nasal cannula versus conventional oxygen therapy in acute COPD exacerbation with mild hypercapnia: a multicenter randomized controlled trial. Crit Care. 2022. https://doi.org/10.1186/s13054-022-03973-7.
Tan D, Wang B, Cao P. High flow nasal cannula oxygen therapy versus non-invasive ventilation for acute exacerbations of chronic obstructive pulmonary disease with acute-moderate hypercapnic respiratory failure: a randomized controlled non-inferiority trial. Crit Care. 2024;28:250.
Luo Z, Li Y, Li W, Effect of High-Intensity vs Low-Intensity Noninvasive Positive Pressure Ventilation on the Need for Endotracheal Intubation in Patients With an Acute Exacerbation of Chronic Obstructive Pulmonary Disease: The HAPPEN Randomized Clinical Trial.JAMA2024; 332:1709
Agustí A, Celli BR, Criner GJ, Global Initiative for Chronic Obstructive Lung Disease 2023 Report: GOLD Executive Summary.Eur Respir J2023; 61:2300239
Díaz GG, Alcaraz AC, Talavera JCP. Noninvasive positive-pressure ventilation to treat hypercapnic coma secondary to respiratory failure. Chest. 2005;127:952–60.
Oczkowski S, Ergan B, Bos L, ERS clinical practice guidelines: high-flow nasal cannula in acute respiratory failure.Eur Respir J2022; 59:2101574
Hernández G, Vaquero C, Colinas L. Effect of postextubation high-flow nasal cannula vs noninvasive ventilation on reintubation and postextubation respiratory failure in high-risk patients: a randomized clinical trial. JAMA. 2016;316:1565.
Hernández G, Paredes I, Moran F. Effect of postextubation noninvasive ventilation with active humidification vs high-flow nasal cannula on reintubation in patients at very high risk for extubation failure: a randomized trial. Intensive Care Med. 2022;48:1751–9.
Thille AW, Muller G, Gacouin A, Effect of Postextubation High-Flow Nasal Oxygen With Noninvasive Ventilation vs High-Flow Nasal Oxygen Alone on Reintubation Among Patients at High Risk of Extubation Failure: A Randomized Clinical Trial.JAMA2019; 322:1465
Boscolo A, Pettenuzzo T, Sella N, Noninvasive respiratory support after extubation: a systematic review and network meta-analysis.Eur Respir Rev2023; 32:220196
Pettenuzzo T, Boscolo A, Pistollato E. Effects of non-invasive respiratory support in post-operative patients: a systematic review and network meta-analysis. Crit Care. 2024;28:152.
Thille AW, Coudroy R, Nay M-A, Beneficial Effects of Noninvasive Ventilation after Extubation in Obese or Overweight Patients: A Post Hoc Analysis of a Randomized Clinical Trial.Am J Respir Crit Care Med2022; 205:440–9
Maggiore SM, Idone FA, Vaschetto R. Nasal high-flow versus Venturi mask oxygen therapy after extubation. Effects on oxygenation, comfort, and clinical outcome. Am J Respir Crit Care Med. 2014;190:282–8.
Hernández G, Vaquero C, González P. Effect of postextubation high-flow nasal cannula vs conventional oxygen therapy on reintubation in low-risk patients: a randomized clinical trial. JAMA. 2016;315:1354.
Maggiore SM, Jaber S, Grieco DL. High-flow versus venturimask oxygen therapy to prevent reintubation in hypoxemic patients after extubation: a multicenter randomized clinical trial. Am J Respir Crit Care Med. 2022;206:1452–62.
Hernández G, Dianti J, Paredes I. Humidified noninvasive ventilation versus high-flow therapy to prevent reintubation in patients with obesity: a randomized clinical trial. Am J Respir Crit Care Med. 2025;211:222–9.
Mokhlesi B, Masa JF, Brozek JL. Evaluation and management of obesity hypoventilation syndrome. An official American Thoracic Society clinical practice guideline. Am J Respir Crit Care Med. 2019;200:e6-24.
Masa JF, Corral J, Alonso ML. Efficacy of different treatment alternatives for obesity hypoventilation syndrome. Pickwick study. Am J Respir Crit Care Med. 2015;192:86–95.
Masa JF, Corral J, Caballero C, Non-invasive ventilation in obesity hypoventilation syndrome without severe obstructive sleep apnoea.Thorax2016; 71:899–906
Borel J-C, Tamisier R, Gonzalez-Bermejo J. Noninvasive ventilation in mild obesity hypoventilation syndrome. Chest. 2012;141:692–702.
Nowbar S, Burkart KM, Gonzales R. Obesity-associated hypoventilation in hospitalized patients: prevalence, effects, and outcome. Am J Med. 2004;116:1–7.
Lee WY, Mokhlesi B Diagnosis and Management of Obesity Hypoventilation Syndrome in the ICU.Critical Care Clinics2008; 24:533–49
Navalesi P, Fanfulla F, Frigerio P, Gregoretti C, Nava S. Physiologic evaluation of noninvasive mechanical ventilation delivered with three types of masks in patients with chronic hypercapnic respiratory failure. Crit Care Med. 2000;28:1785–90.
Fauroux B Why, when and how to propose noninvasive ventilation in cystic fibrosis?.Minerva Anestesiol2011; 77:1108–14
Sood N, Paradowski LJ, Yankaskas JR. Outcomes of intensive care unit care in adults with cystic fibrosis. Am J Respir Crit Care Med. 2001;163:335–8.
Texereau J, Jamal D, Choukroun G. Determinants of mortality for adults with cystic fibrosis admitted in intensive care unit: a multicenter study. Respir Res. 2006;7:14.
Sklar MC, Dres M, Rittayamai N. High-flow nasal oxygen versus noninvasive ventilation in adult patients with cystic fibrosis: a randomized crossover physiological study. Ann Intensive Care. 2018;8:85.
Bersten AD, Holt AW, Vedig AE, Skowronski GA, Baggoley CJ Treatment of Severe Cardiogenic Pulmonary Edema with Continuous Positive Airway Pressure Delivered by Face Mask.N Engl J Med1991; 325:1825–30
Yoshida T, Uchiyama A, Matsuura N, Mashimo T, Fujino Y. The comparison of spontaneous breathing and muscle paralysis in two different severities of experimental lung injury. Crit Care Med. 2013;41:536–45.
Brochard L, Slutsky A, Pesenti A Mechanical Ventilation to Minimize Progression of Lung Injury in Acute Respiratory Failure.Am J Respir Crit Care Med2017; 195:438–42
Bhattacharya M, Kallet RH, Ware LB, Matthay MA. Negative-pressure pulmonary edema. Chest. 2016;150:927–33.
Cressoni M, Cadringher P, Chiurazzi C. Lung inhomogeneity in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2014;189:149–58.
Antonelli M, Conti G, Moro M, Predictors of failure of noninvasive positive pressure ventilation in patients with acute hypoxemic respiratory failure: a multi-center study.Intensive Care Med2001; 27:1718–28
Thille AW, Contou D, Fragnoli C, Córdoba-Izquierdo A, Boissier F, Brun-Buisson C. Non-invasive ventilation for acute hypoxemic respiratory failure: intubation rate and risk factors. Crit Care. 2013;17:R269.
Rana S, Jenad H, Gay PC, Buck CF, Hubmayr RD, Gajic O. Failure of non-invasive ventilation in patients with acute lung injury: observational cohort study. Crit Care. 2006;10:R79.
Frat J-P, Ragot S, Coudroy R. Predictors of intubation in patients with acute hypoxemic respiratory failure treated with a noninvasive oxygenation strategy*. Crit Care Med. 2018;46:208–15.
Antonelli M, Conti G, Esquinas A, A multiple-center survey on the use in clinical practice of noninvasive ventilation as a first-line intervention for acute respiratory distress syndrome*.Critical Care Medicine2007; 35:18–25
Carrillo A, Gonzalez-Diaz G, Ferrer M, Non-invasive ventilation in community-acquired pneumonia and severe acute respiratory failure.Intensive Care Med2012; 38:458–66
Carteaux G, Millán-Guilarte T, De Prost N, Failure of Noninvasive Ventilation for De Novo Acute Hypoxemic Respiratory Failure: Role of Tidal Volume*.Critical Care Medicine2016; 44:282–90
Docci M, Rezoagli E, Teggia-Droghi M. Individual response in patient’s effort and driving pressure to variations in assistance during pressure support ventilation. Ann Intensive Care. 2023;13:132.
Marti S, Carsin A-E, Sampol J. Higher mortality and intubation rate in COVID-19 patients treated with noninvasive ventilation compared with high-flow oxygen or CPAP. Sci Rep. 2022;12:6527.
Rezoagli E, Villa S, Gatti S, Helmet and face mask for non-invasive respiratory support in patients with acute hypoxemic respiratory failure: A retrospective study.Journal of Critical Care2021; 65:56–61
Tuffet S, Boujelben MA, Haudebourg A-F, High flow nasal cannula and low level continuous positive airway pressure have different physiological effects during de novo acute hypoxemic respiratory failure.Ann Intensive Care2024; 14:171
Giani M, Rezoagli E, Raimondi Cominesi D. Effect of helmet CPAP on tidal volume assessed by bioelectrical impedance. Respir Care. 2024;69:1332–5.
Gatti S, Rezoagli E, Madotto F, Foti G, Bellani G. A non-invasive continuous and real-time volumetric monitoring in spontaneous breathing subjects based on bioimpedance—ExSpiron®Xi: a validation study in healthy volunteers. J Clin Monit Comput. 2024;38:539–51.
Grieco DL, Menga LS, Cesarano M, Phenotypes of Patients with COVID-19 Who Have a Positive Clinical Response to Helmet Noninvasive Ventilation.Am J Respir Crit Care Med2022; 205:360–4
Duan J, Han X, Bai L, Zhou L, Huang S Assessment of heart rate, acidosis, consciousness, oxygenation, and respiratory rate to predict noninvasive ventilation failure in hypoxemic patients.Intensive Care Med2017; 43:192–9
Duan J, Wang S, Liu P, Early prediction of noninvasive ventilation failure in COPD patients: derivation, internal validation, and external validation of a simple risk score.Ann Intensive Care2019; 9:108
Roca O, Caralt B, Messika J. An index combining respiratory rate and oxygenation to predict outcome of nasal high-flow therapy. Am J Respir Crit Care Med. 2019;199:1368–76.
Colaianni-Alfonso N, Montiel GC, Castro-Sayat M, Roca O, Grieco DL. Rox index to predict CPAP outcome in hypoxemic respiratory failure due to COVID-19. Intensive Care Med. 2022;48:1818–9.
Chen D, Heunks L, Pan C. A novel index to predict the failure of high-flow nasal cannula in patients with acute hypoxemic respiratory failure: a pilot study. Am J Respir Crit Care Med. 2022;206:910–3.
Registry Team, De Alencar JCG, Marchini JFM. Lung ultrasound score predicts outcomes in COVID-19 patients admitted to the emergency department. Ann Intensive Care. 2021;11:6.
Nova A, Rezoagli E, Eronia N. Prognostic performance of bedside lung ultrasound score (LUSS) and ROX index in hypoxemic respiratory failure due to COVID-19. Diagnostics. 2023;13:1361.
Goligher EC, Laghi F, Detsky ME. Measuring diaphragm thickness with ultrasound in mechanically ventilated patients: feasibility, reproducibility and validity. Intensive Care Med. 2015;41:734.
Mercurio G, D’Arrigo S, Moroni R, Diaphragm thickening fraction predicts noninvasive ventilation outcome: a preliminary physiological study.Crit Care2021; 25:219
Sakuraya M, Douno E, Iwata W, Accuracy evaluation of mainstream and sidestream end-tidal carbon dioxide monitoring during noninvasive ventilation: a randomized crossover trial (MASCAT-NIV trial).j intensive care2022;10
Rauseo M, Mirabella L, Laforgia D. A pilot study on electrical impedance tomography during CPAP trial in patients with severe acute respiratory syndrome coronavirus 2 pneumonia: the bright side of non-invasive ventilation. Front Physiol. 2021;12:728243.
Wisse JJ, Flinsenberg MJW, Jonkman AH, Goos TG, Gommers D. Respiratory rate monitoring in ICU patients and healthy volunteers using electrical impedance tomography: a validation study. Physiol Meas. 2024;45:055026.
Lin W-C, Su P-F, Chen C-W Pendelluft in patients with acute respiratory distress syndrome during trigger and reverse triggering breaths.Sci Rep2023; 13:22143
Sang L, Zhao Z, Yun P-J, Qualitative and quantitative assessment of pendelluft: a simple method based on electrical impedance tomography.Ann Transl Med2020; 8:1216–1216