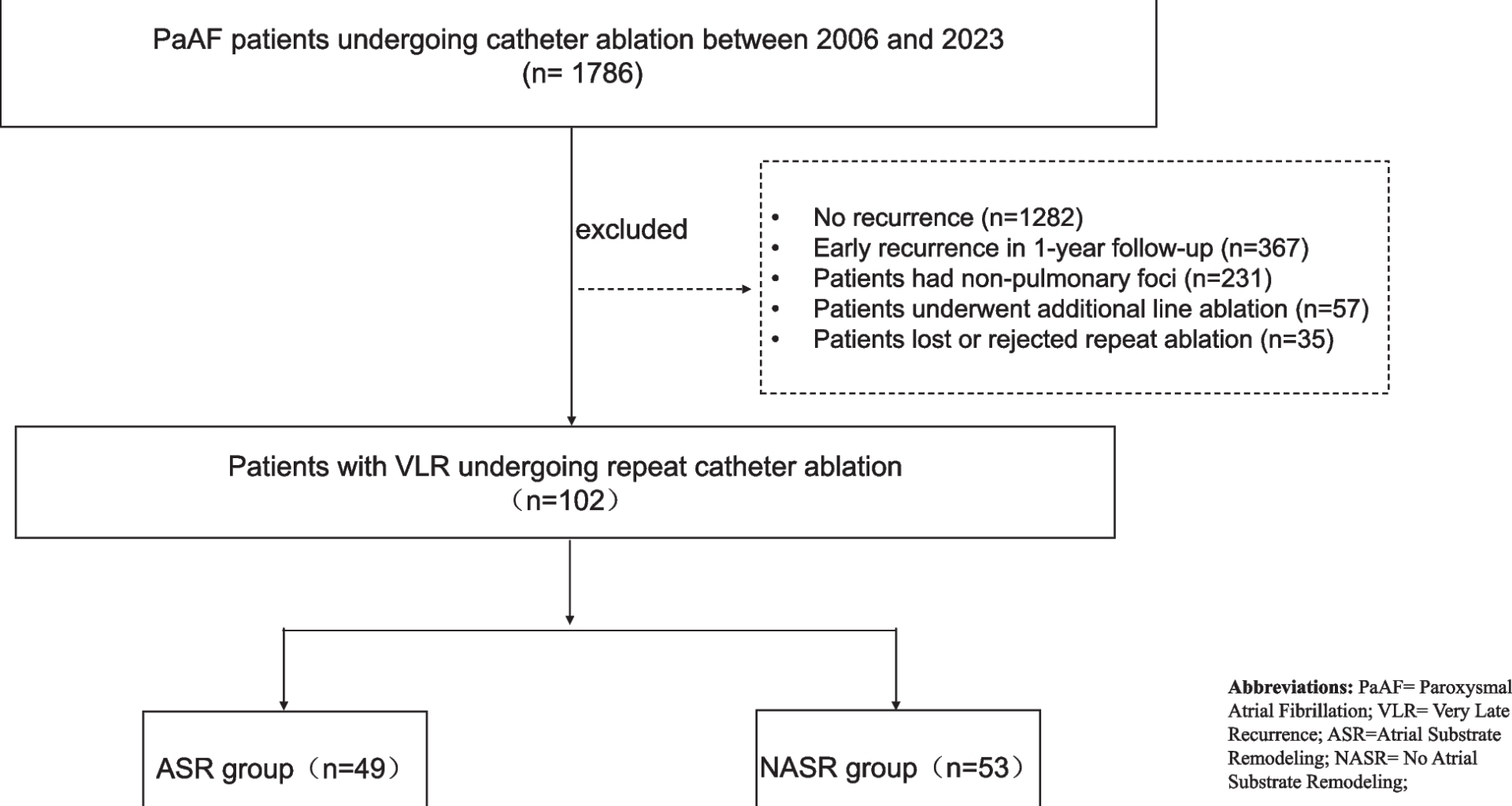
Study population
During a median follow-up period of 4 years, 102 patients undergoing repeat ablation procedures were enrolled, with exclusion criteria detailed in Fig. 1. The cohort was stratified into an atrial substrate remodeling (ASR) group (n = 49, 48%; mean age: 62.0 ± 9.0 years, 45%male) and non-atrial substrate remodeling (NASR) group (n = 53, 52%; mean age: 61.0 ± 10.0 years, 62%male).
The protocol and flow of our study
Baseline characteristics and clinical parameters
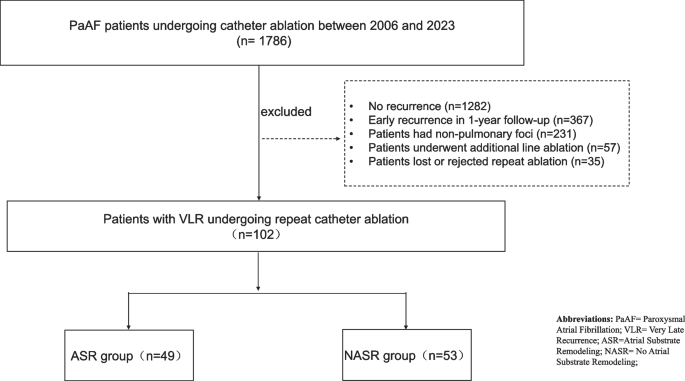
Baseline demographic and clinical characteristics are summarized in Table 1. The two groups demonstrated comparable distributions of age, gender, body mass index (BMI), smoke, alcohol, combined diseases (hypertension, T2DM, heart failure, etc.), NT-pro-BNP, and average HAS-BLED score. Similarly, anti-arrhythmia medication profiles were similarly balanced between groups, including β-blocker use (55% vs. 59%, P = 0.73), amiodarone (57% vs. 74%, P = 0.08), and propafenone (18% vs. 13%, P = 0.47). Notably, the ASR group exhibited a significantly higher CHA2DS2-VASc score compared to the NASR group (2.5 ± 1.4 vs. 1.8 ± 1.6, P = 0.02) (Fig. 2A), suggesting an elevated thromboembolic risk profile.
Table 1 Baseline characteristics of the PaAF population undergoing repeat ablation procedureFig. 2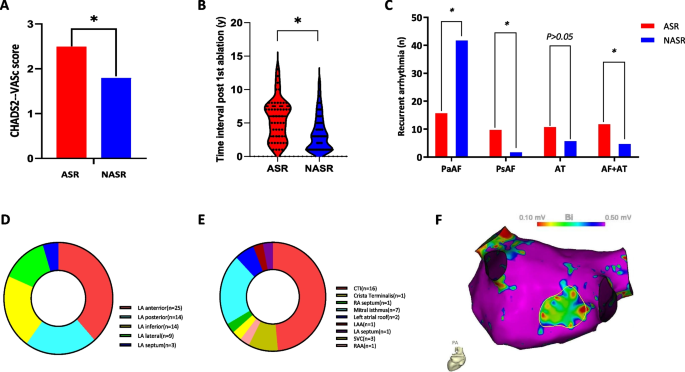
A Patients in ASR group had significantly higher average CHA2DS2-VASc score than that in NASR group. B PaAF patients with atrial substrate remodeling (ASR group) had longer time interval post 1st CPVI ablation than NASR group (P < 0.001) via violin plot. C The recurrent type of arrhythmia made no significant difference between ASR group and NASR group. PaAF was the most common type of recurrent arrhythmia post 1st ablation procedure. D The distribution of abnormal atrial substrate areas in ASR group. E The distribution of non-pulmonary foci of RA and LA in ASR group. F A representative figure of low voltage area (bipolar voltage < 0.5 mV, tagged by yellow circle) locating at the LA posterior wall on CARTO system. ASR = Atrial Substrate Remodeling; NASR = No Atrial Substrate Remodeling; PaAF = paroxysmal atrial fibrillation; PsAF = persistent atrial fibrillation; AT = Atrial tachycardia; LA = Left atrium; CTI = Cavo tricuspid isthmus; RA = Right atrium; LAA = Left atrial appendage; SVC = Superior vena cava; RAA = Right atrial appendage. P value < 0.05 means significant difference by arterisk
Recurrence patterns post-ablation
The median time to arrhythmia recurrence following the initial ablation was significantly prolonged in the ASR group (6 years vs. 3 years; P < 0.05; Fig. 2B) compared to the NASR group, indicating a distinct delayed recurrence phenotype in ASR patients after catheter ablation (CA).
PVs-LA reconnection between ASR and NASR group
During repeat ablation procedures, PVs-LA reconnection was systematically analyzed. In the NASR group, 92 PVs-LA reconnection were identified, with 32 patients (60% of the NASR cohort) exhibiting PV recurrence. The recurrence distribution across individual PVs was as follows: right superior PV (RSPV, 16.3%; 15/92), right inferior PV (RIPV, 21.7%; 20/92), left superior PV (LSPV, 38.0%; 35/92) and left inferior PV (LIPV, 23.9%; 22/92)respectively, with LSPV demonstrating the highest recurrence frequency.
In contrast, the ASR group exhibited significantly fewer PVs-LA reconnections compared to the NASR group (16 vs. 92 reconnections, P < 0.001). The recurrence rates for individual PVs in the ASR cohort were RSPV (18.8%; 3/16), RIPV (25.0%; 4/16), LSPV(37.5%; 6/16) and LIPV(18.8%; 3/16), with LSPV remaining the most recurrent PV. Notably, no statistically significant differences were observed in the recurrence rates of individual PVs between the ASR and NASR group (P > 0.05 for all comparisons).
Recurrent arrhythmia profiles
Recurrent arrhythmias during follow-up were classified into four subtypes: paroxysmal atrial fibrillation (PaAF), persistent atrial fibrillation (PsAF), atrial tachycardia (AT), and combined AF/AT. The ASR group exhibited a significantly higher incidence of PsAF recurrence compared to the NASR group (20% [10/49] vs. 4% [2/53]; P < 0.05). Conversely, the NASR group demonstrated a higher predominance of PaAF recurrence (79% [42/53] vs. 33% [16/49] in the ASR group; P < 0.05). No significant intergroup difference was observed in isolated AT recurrence. However, a higher proportion of ASR patients experienced combined AF/AT recurrence compared to the NASR group(24% [12/49] vs. 9% [5/53]; P < 0.05; Fig. 2C).
Area distribution of ASR
In the ASR cohort (n = 65), all newly identified low-voltage areas (LVAs) were localized to the LA (Fig. 2F) with no RA involvement. The LA anterior wall demonstrated the highest prevalence of structural remodeling (38.5%, 25/65), followed by the posterior (21.5%, 14/65) and inferior walls (21.5%, 14/65), lateral wall (13.8%, 9/65), and interatrial septum (4.6%,3/65), as depicted in Fig. 2D.
Non-PV foci were identified in 33 cases, with predominant RA distribution (66.7%, 22/33 vs. 33.3%, 11/33 in LA). RA foci clustered at the cavo tricuspid isthmus (CTI, 72.7%, 16/22), with sparse distribution at the right atrial appendage (RAA, 4.5%,1/22), superior vena cava (SVC, 9.1%,2/22), crista terminalis (4.5%,1/22), and RA septum (4.5%,1/22). LA foci primarily localized to the mitral isthmus (63.6%, 7/11), with additional sites at the roof (18.2%, 2/11), left atrial appendage( LAA,9.1%,1/11), and LA septum (9.1%,1/11), as showed in Fig. 2E.
Cardiac function comparison between ASR and NASR cohorts
No intergroup difference was observed in baseline NT-proBNP levels (P > 0.05), left atrium size (LA1: 38.6 ± 5.3 mm vs. 38.5 ± 4.4 mm, P = 0.86), and left ventricular ejection fraction (LVEF1: 65.3 ± 6.9% vs. 65.3 ± 4.4%, P = 0.95). Furthermore, at the repeat procedure, no significant difference was found in LA size (LA2: 39.9 ± 6.0 mm vs. 38.1 ± 4.4 mm, P = 0.11) and LVEF (LVEF2: 64.0 ± 5.1% vs. 65.6 ± 4.2%, P = 0.10). Longitudinal analysis revealed no significant changes in LA (△LA = LA2-LA1: 0.4(-3.7,6.5) mm vs. -0.9(-5.6,3.7) mm, P = 0.32) and LVEF (△LVEF = LVEF2-LVEF1: -0.1(-4.2,3.1)% vs. 0(-3,3.6)%, P = 0.50) between the ASR and NASR groups, suggesting that ASR did not impact the changes in LA size or LVEF (Table 2).
Table 2 Type of recurrent arrhythmia and cardiac structure between ASR group and NASR groupPredictors of ASR in the VLR of PaAF population
The clinical factors associated with ASR are summarized in Table 3. Cox regression analysis identified recurrent persistent AF (PsAF) as an independent predictor of ASR development: univariate association: HR = 6.54, 95% CI 1.35–31.57, P = 0.02, Multivariate adjustment (HR = 2.66, 95%CI = 1.05–6.73, P = 0.04). (adjusted for age, CHA2DS2-VASc score, and atrial dilatation status).
Table 3 Risk factors associated with ASR in the VLR of PaAF population