Lisowska-Lysiak K, Lauterbach R, Miedzobrodski J, Kosecka-Strojek M. Epidemiology and pathogenesis of Staphylococcus bloodstream infections in humans: a review. Pol J Microbiol. 2021;70(1):13–23. https://doi.org/10.33073/pjm-2021-005.
Heilmann C, Ziebuhr W, Becker K. Are coagulase-negative Staphylococci virulent? Clin Microbiol Infect. 2019;25(9):1071–80. https://doi.org/10.1016/j.cmi.2018.11.012.
Naber CK. Staphylococcus aureus bacteremia: epidemiology, pathophysiology, and management strategies. Clin Infect Dis. 2009;48(Supplement4):S231–7. https://doi.org/10.1086/598189.
Tong SYC, Davis JS, Eichenberger E, Holland TL, Fowler VG. Staphylococcus aureus infections: epidemiology, pathophysiology, clinical manifestations, and management. Clin Microbiol Rev. 2015;28(3):603–61. https://doi.org/10.1128/cmr.00134-14.
Pain M, Wolden R, Jaén-Luchoro D, et al. Staphylococcus borealis sp. nov., isolated from human skin and blood. Int J Syst Evol Microbiol. 2020;70(12):6067–78. https://doi.org/10.1099/ijsem.0.004499.
Król J, Wanecka A, Twardoń J, et al. Staphylococcus borealis – a newly identified pathogen of bovine mammary glands. Vet Microbiol. 2023;286:109876. https://doi.org/10.1016/j.vetmic.2023.109876.
Cavanagh JP, Klingenberg C, Venter HJ et al. Revealing the clinical relevance of Staphylococcus borealis. Microbiol Spectr 13(4):e01988–24. https://doi.org/10.1128/spectrum.01988-24
Bruynoghe R, Maisin J. Essais de thérapeutique au moyen du bacteriophage – ScienceOpen. Accessed August 8, 2024. https://www.scienceopen.com/document?vid=f9178fff-aba9-440f-a4dd-1316136e86a7
Sulakvelidze A, Alavidze Z, Morris JG. Bacteriophage therapy. Antimicrob Agents Chemother. 2001;45(3):649–59. https://doi.org/10.1128/AAC.45.3.649-659.2001.
Almeida GM, de Sundberg F. The forgotten Tale of Brazilian phage therapy. Lancet Infect Dis. 2020;20(5):e90–101. https://doi.org/10.1016/S1473-3099(20)30060-8.
Göller PC, Elsener T, Lorgé D, et al. Multi-species host range of Staphylococcal phages isolated from wastewater. Nat Commun. 2021;12(1):6965. https://doi.org/10.1038/s41467-021-27037-6.
Plumet L, Ahmad-Mansour N, Dunyach-Remy C, et al. Bacteriophage therapy for Staphylococcus aureus infections: a review of animal models, treatments, and clinical trials. Front Cell Infect Microbiol. 2022. https://doi.org/10.3389/fcimb.2022.907314.
Pirnay JP, Djebara S, Steurs G, et al. Personalized bacteriophage therapy outcomes for 100 consecutive cases: a multicentre, multinational, retrospective observational study. Nat Microbiol. 2024;9(6):1434–53. https://doi.org/10.1038/s41564-024-01705-x.
Alsaadi SE, Lu H, Zhang M, Dykes GF, Allison HE, Horsburgh MJ. Bacteriophages from human skin infecting coagulase-negative staphylococcus: diversity, novelty and host resistance. Sci Rep. 2024;14(1):8245. https://doi.org/10.1038/s41598-024-59065-9.
Lopes MS, Silva MD, Azeredo J, Melo LDR. Coagulase-negative staphylococci phages panorama: genomic diversity and in vitro studies for a therapeutic use. Microbiol Res. 2025;290:127944. https://doi.org/10.1016/j.micres.2024.127944.
Merabishvili M, Pirnay JP, Verbeken G, et al. Quality-controlled small-scale production of a well-defined bacteriophage cocktail for use in human clinical trials. PLoS ONE. 2009;4(3):e4944. https://doi.org/10.1371/journal.pone.0004944.
Sharifi F, Montaseri M, Yousefi MH, et al. Isolation and characterization of two Staphylococcus aureus lytic bacteriophages Huma and Simurgh. Virology. 2024;595:110090. https://doi.org/10.1016/j.virol.2024.110090.
Vandersteegen K, Mattheus W, Ceyssens PJ, et al. Microbiological and molecular assessment of bacteriophage ISP for the control of Staphylococcus aureus. PLoS ONE. 2011;6(9):e24418. https://doi.org/10.1371/journal.pone.0024418.
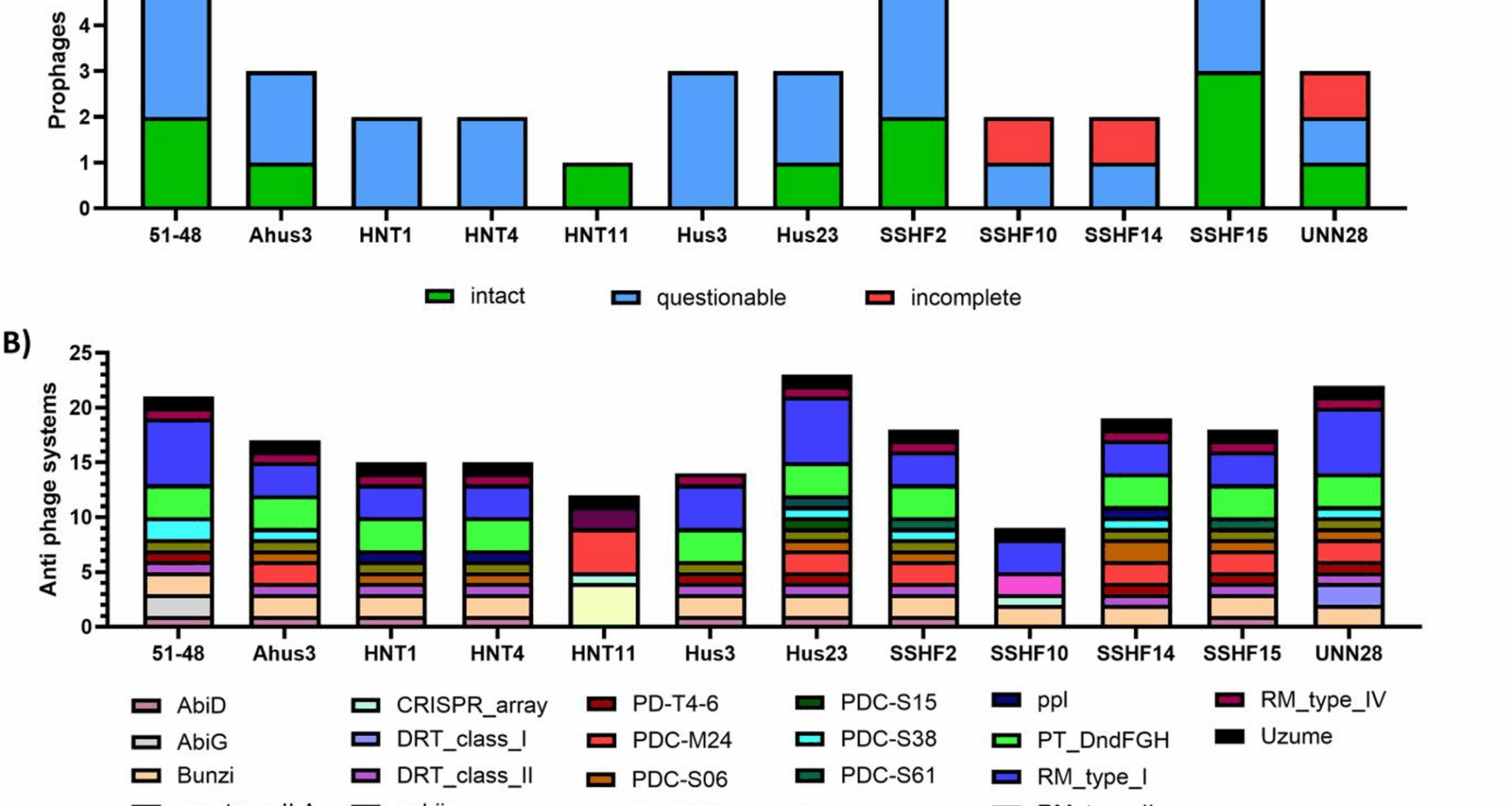
Wishart DS, Han S, Saha S, et al. PHASTEST: faster than PHASTER, better than PHAST. Nucleic Acids Res. 2023;51(W1):W443–50. https://doi.org/10.1093/nar/gkad382.
Payne LJ, Meaden S, Mestre MR, et al. PADLOC: a web server for the identification of antiviral defence systems in microbial genomes. Nucleic Acids Res. 2022;50(W1):W541–50. https://doi.org/10.1093/nar/gkac400.
Daniel A, Bonnen PE, Fischetti VA. First complete genome sequence of two Staphylococcus epidermidis bacteriophages. J Bacteriol. 2007;189(5):2086–100. https://doi.org/10.1128/JB.01637-06.
Zeman M, Bárdy P, Vrbovská V, et al. New genus fibralongavirus in siphoviridae phages of Staphylococcus Pseudintermedius. Viruses. 2019;11(12):1143. https://doi.org/10.3390/v11121143.
Naghavi M, Vollset SE, Ikuta KS, et al. Global burden of bacterial antimicrobial resistance 1990–2021: a systematic analysis with forecasts to 2050. Lancet. 2024. https://doi.org/10.1016/S0140-6736(24)01867-1.
Ngassam-Tchamba C, Duprez JN, Fergestad M, et al. In vitro and in vivo assessment of phage therapy against Staphylococcus aureus causing bovine mastitis. J Glob Antimicrob Resist. 2020;22:762–70. https://doi.org/10.1016/j.jgar.2020.06.020.
Kwan T, Liu J, DuBow M, Gros P, Pelletier J. The complete genomes and proteomes of 27 Staphylococcus aureus bacteriophages. Proc Natl Acad Sci U S A. 2005;102(14):5174–9. https://doi.org/10.1073/pnas.0501140102.
Merabishvili M, Vervaet C, Pirnay JP, et al. Stability of Staphylococcus aureus phage ISP after freeze-drying (lyophilization). PLoS ONE. 2013;8(7):e68797. https://doi.org/10.1371/journal.pone.0068797.
Vandersteegen K, Kropinski AM, Nash JHE, Noben JP, Hermans K, Lavigne R. Romulus and Remus, two phage isolates representing a distinct clade within the twortlikevirus genus, display suitable properties for phage therapy applications. J Virol. 2013;87(6):3237–47. https://doi.org/10.1128/jvi.02763-12.
Verheul M, Mulder AA, van Dun SCJ, et al. Bacteriophage ISP eliminates Staphylococcus aureus in planktonic phase, but not in the various stages of the biofilm cycle. Sci Rep. 2024;14(1):14374. https://doi.org/10.1038/s41598-024-65143-9.
O’Flaherty S, Ross RP, Meaney W, Fitzgerald GF, Elbreki MF, Coffey A. Potential of the polyvalent Anti-Staphylococcus bacteriophage K for control of Antibiotic-Resistant Staphylococci from hospitals. Appl Environ Microbiol. 2005;71(4):1836–42. https://doi.org/10.1128/AEM.71.4.1836-1842.2005.
Łubowska N, Grygorcewicz B, Kosznik-Kwaśnicka K, et al. Characterization of the three new kayviruses and their lytic activity against multidrug-resistant Staphylococcus aureus. Microorganisms. 2019;7(10):471. https://doi.org/10.3390/microorganisms7100471.
Götz F, Popp F, Schleifer KH. Isolation and characterization of a virulent bacteriophage from Staphylococcus carnosus. FEMS Microbiol Lett. 1984;23(2–3):303–7. https://doi.org/10.1111/j.1574-6968.1984.tb01083.x.
Benešík M, Nováček J, Janda L, et al. Role of SH3b binding domain in a natural deletion mutant of kayvirus endolysin LysF1 with a broad range of lytic activity. Virus Genes. 2018;54(1):130–9. https://doi.org/10.1007/s11262-017-1507-2.
Oduor JMO, Kadija E, Nyachieo A, Mureithi MW, Skurnik M. Bioprospecting Staphylococcus phages with therapeutic and bio-control potential. Viruses. 2020;12(2):133. https://doi.org/10.3390/v12020133.
Kolenda C, Bonhomme M, Medina M, et al. Potential of training of anti-Staphylococcus aureus therapeutic phages against Staphylococcus epidermidis multidrug-resistant isolates is restricted by inter- and intra-sequence type specificity. mSystems. 2024;9(10):e00850–24. https://doi.org/10.1128/msystems.00850-24.
Gutiérrez D, Vandenheuvel D, Martínez B, Rodríguez A, Lavigne R, García P. Two phages, phiIPLA-RODI and phiIPLA-C1C, lyse mono- and dual-species Staphylococcal biofilms. Appl Environ Microbiol. 2015;81(10):3336–48. https://doi.org/10.1128/AEM.03560-14.
Meaden S, Westra E, Fineran P. Phage defence system abundances vary across environments and increase with viral density. Published online January 16, 2025:2025.01.16.633327. https://doi.org/10.1101/2025.01.16.633327
Burke KA, Urick CD, Mzhavia N, Nikolich MP, Filippov AA. Correlation of Pseudomonas aeruginosa phage resistance with the numbers and types of antiphage systems. Int J Mol Sci. 2024;25(3):1424. https://doi.org/10.3390/ijms25031424.
Gaborieau B, Vaysset H, Tesson F, et al. Prediction of strain level phage–host interactions across the Escherichia genus using only genomic information. Nat Microbiol. 2024;9(11):2847–61. https://doi.org/10.1038/s41564-024-01832-5.
Moller AG, Winston K, Ji S, et al. Genes influencing phage host range in Staphylococcus aureus on a species-wide scale. mSphere. 2021;6(1):e01263-20. https://doi.org/10.1128/mSphere.01263-20.
Moller AG, Lindsay JA, Read TD. Determinants of Phage Host Range in Staphylococcus Species. Appl Environ Microbiol., Walsh SK, Imrie RM, Matuszewska M et al. The host phylogeny determines viral infectivity and replication across Staphylococcus host species. PLOS Pathogens. 2023;19(6):e1011433. doi:10.1371/journal.ppat.1011433.
Botka T, Pantůček R, Mašlaňová I, et al. Lytic and genomic properties of spontaneous host-range kayvirus mutants prove their suitability for upgrading phage therapeutics against Staphylococci. Sci Rep. 2019;9(1):5475. https://doi.org/10.1038/s41598-019-41868-w.