Theme 1: deficiencies in hospital-provided management (ABM-contextual characteristics)
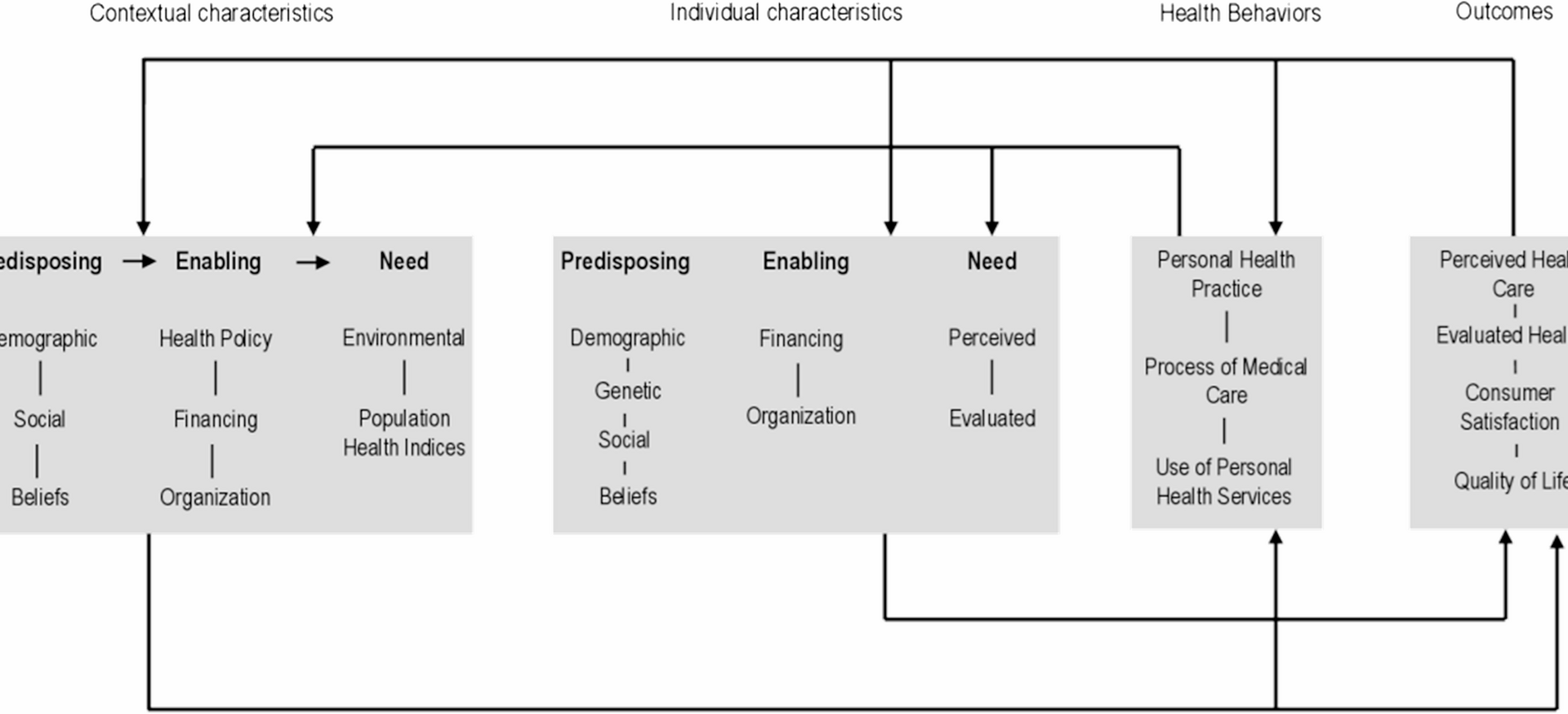
This theme reflects the institutional barriers embedded in hospital-provided oral care. Although patients were receiving treatment in psychiatric wards, oral health was not prioritized (predisposing factor), and specialized oral health services were absent (enabling factor). Furthermore, there was a need for more effective OHM (need factor), which remained unmet in the current service context. Together, these factors compromised patients’ health behaviors and further led to patients’ dissatisfaction with oral health management and the emergence of unmet needs in oral health care.
Low priority of oral health (predisposing factor)
Some of the patients with LLD mentioned that oral health issues were consistently deprioritized in psychiatric wards. When dental problems such as toothaches occurred, psychiatrists typically provided superficial treatment or observational monitoring without offering appropriate intervention, which failed to address the underlying causes of these conditions.
A4: “…It seems that the hospital doesn’t pay much attention to oral health either, so we can only take care of our own teeth. When I have a toothache, they just prescribe a bottle of mouthwash, but I feel this only treats the symptom rather than the root cause.”
A6: “…a few days ago, I told them (psychiatric nurses) my teeth were feeling off. Someone came to check them out, but didn’t really do anything about it. And when they don’t hurt or nothing, nobody pays them any mind.”
Lack of oral health services (enabling factor)
Some participants reported that specialized oral health services were absent in psychiatric hospitals, along with a lack of dental professionals to carry out oral examinations, treatments and guidance.
A2: “It (The hospital) doesn’t do enough in this aspect. There is no dental department here, and no professional staff to examine and help cleaning our teeth.”
A16: “It would be great if the hospital could have specialized dentists or nurses to help us with examination, treatment, and guidance.”
Patients’ need for effective oral health management (need factor)
The majority of patients with LLD expressed that although they had existing dental problems, these needs were neither adequately recognized nor systematically addressed in psychiatric wards. The existing oral health management still needs to be improved, which mainly includes oral assessment and care, management of special oral conditions, denture and daily life management.
A2: “Here, the doctors and nurses rarely check my teeth. After all, their daily work almost occupies most of their time.”
A3: “…My teeth always have tartar. It is more useful to brush my teeth properly by myself than the oral care provided by the hospital. All they do is wipe them with cotton—just a little wipe, you know? How clean can that really get them?”
A15: “Right now, the caregiver helps me clean my dentures, but since she has no prior experience with denture care… it takes a lot of effort and time each time to put the dentures back in place.”
A16: “It would be nice to have someone to teach us how to brush our teeth correctly and help us check our teeth after brushing.”
Theme 2: a positive attitude towards oral health coexists with undesirable situations (ABM-individual characteristics)
This theme highlights a paradox within individual characteristics. Although many patients acknowledged the significance of oral health (predisposing factor), this recognition coexisted with adverse conditions that undermined effective OHM. Specifically, inappropriate oral health beliefs, psychological challenges (predisposing factors), financial burdens, a lack of self-management capacity, and restrictive environmental constraints (enabling factors) contributed to poor oral health status (need factor, outcome) and poor health behaviors (health behaviors).
Positive attitudes (predisposing factor)
All of the participants emphasized the significant role of oral health in daily life and well-being. Some patients considered that oral health was essential to maintain a normal life.
A2: “Oral health is certainly important. Whether it’s eating, chewing or speaking, it just can’t be done without our teeth.”
Others were aware of the negative impact of poor oral health to overall health, such as nutrition and depression.
A1: “…It’s hard to eat whatever I want without teeth. My sister is ten years younger than me, but she only has a few teeth left and emaciated body. Although I’m suffering from this illness, my overall condition is better than hers.”
A7: “…If your oral health is poor, you will suffer from toothache, and the pain can be sheer torture. It is so painful that you can neither eat will nor sleep well, making you extremely anxious, and it’s very likely to get the illness(depression).”
Poor oral health awareness (predisposing factor)
Although all patients acknowledged the importance of oral health, the majority perceived their oral status as healthy despite experiencing untreated dental problems. A few patients tended to believe that these issues were common and inevitable consequences caused by ageing or mental disorders, which in turn led to poor oral health behaviors.
A5: “Right now I think my oral is fairly healthy. Sometimes there’s a blood mark when I eat an apple, but it’s not a big deal. This situation will disappear anyway.”
A13: “…I guess it has something to do with my illness. If my mental condition gets better, these oral problems should heal on their own, so I’m just going to leave them be.”
Reduced motivation induced by depression (predisposing factor)
Many patients with LLD reported a noticeable decline in willpower and daily functioning during depressive episodes, which often led to neglect of basic self-care behaviors, such as reduced frequency of tooth brushing or reluctance to brush their teeth at all. Moreover, these patients commonly exhibited a decreased sense of self-worth, which frequently resulted in a lack of initiative to seek professional dental care.
A10: “…My teeth have never been good, I’d rather lie in bed all day than even bother to brush them when I’m in a bad mood…But I can’t be bothered to go to the hospital for check-ups or treatment. Anyway, they don’t hurt, so I just leave them be. Don’t wanna mess with it.”
A13: “No need. I Don’t wanna bother them(medical staffs). I’m this old already, lost quite a few teeth. There is no point in getting checked or treated, because it won’t do no good. And my teeth are in such a mess.It is just way too embarrassing to let someone check them out…”.
Financial burden (enabling factor)
Most patients with LLD had already retired and no longer had a stable source of income. As a result, many of them expressed concerns about the cost of dental services. These financial worries often contributed to hesitation or avoidance in seeking necessary oral health care.
A5: “There is a charge for the oral care provided by the hospital, isn’t there? Is it covered by medical insurance if it is charged? That is exactly what I worry about.”
Lack of oral health management capacity (enabling factor)
A proportion of elderly patients with depression had difficulties in oral health self-management due to lack of oral care knowledge and skills, negative perceptions toward oral care, and physical frailty.
A4: “…I have been brushing my teeth under the guidance of Instructional videos, but I still feel that the effect is not ideal.”
A7: “ Only when I feel uncomfortable will I need to have my teeth examined and treated…”.
A15: “… However because of physically weakness, I may not be able to apply enough force with my hands, and that results in incomplete cleaning and difficulty in brushing”.
Limitations of the inpatient environment (enabling factor)
During hospitalization, some patients reported that it was inconvenient to carry dentures and oral cleaning aids, such as dental floss. Furthermore, due to the limited facilities in some wards, patients found it less convenient to brush their teeth in the ward, which compromised the effectiveness of their oral health self-management.
A2: “The mirror here doesn’t work well, and I can only brush my teeth casually since I can’t even see if I’ve done a good job or not.”
A4: “At home, I used to floss after meals, but it’s not convenient to bring dental floss or toothpicks here, so I’ve stopped using them for now.”
A9: “Of course it’s not as convenient to brush my teeth in the hospital as it is at home. Besides I didn’t bring much with me, including my dentures, so I was relatively casual about oral care in the hospital.”
Poor oral health status (need factor)
Most of the interviewees mentioned that they experienced multiple oral health problems, including halitosis, dental caries, toothache, bleeding gums, loose teeth, missing teeth or loose denture.
A4: “I think I have a rather serious problem with bad breath. Sometimes my gums bleed when I brush my teeth…”.
A8: “…You can see there are several decayed teeth right here, and some of my teeth have fallen out. I also feel that the gaps between my teeth are quite big. I guess that’s just how it is when one gets old.”
Theme 3: difficulties in self-management (ABM-health behaviors)
This theme reflects the challenges faced by elderly patients with late-life depression in maintaining their oral health behaviors during hospitalization. It includes two subthemes: negative changes in daily behavior (personal health practices) and hesitation or refusal of access to care (use of health services). These behavioral barriers further contributed to unfavorable oral health outcomes.
Negative changes in daily behaviour (personal health practices)
About two-thirds of the patients reported that they maintained relatively regular oral health practices, such as brushing at least once a day and using toothpicks or dental floss for interdental cleaning before hospitalization. However, most of them reflected that since hospitalization, their oral health care had deteriorated because of laziness, changes in the hospital environment or limited facilities. The changes in oral health care were mainly in reduced frequency and duration of brushing.
A2: “I used to brush my teeth at least once in the morning and once in the evening, but after coming here, sometimes I don’t want to brush my teeth at night because of laziness.”
A17: “I’ve become lazier than ever before. Now I just rinse my mouth, and sometimes I brush my teeth casually.”
Hesitation, delay or refusal of access to care (use of health services)
Several patients expressed hesitation or even refusal to seek professional dental care. Their hesitation was often related not only to financial concerns but also to emotional and attitudinal barriers. Some patients emphasized feelings of embarrassment about the state of their teeth, doubts about the effectiveness of dental treatments at their age or a diminished sense of self-worth. Others reported a tendency to delay care unless pain or acute problems occurred, reflecting a reactive rather than preventive approach to oral health.
A15: “…I think oral care is my own business and a small thing, too. And I’m a bit worried about being examined and told that my oral condition is a whole mess. So I don’t bother the doctors and nurses to do it for us.”
A6: “I’m already at this age and have hypertension. It (dental treatment) can’t make my teeth grow back…”.
A17: “I Don’t need them (medical staffs) to provide the oral health management, it’s too much trouble for others. See, I’m already an old people.”
Theme 4: patients’ demand for oral health management (ABM-outcomes)
Patients reported dissatisfaction with OHM, perceiving little improvement or even deterioration in their oral condition, which discouraged positive oral health behaviors. At the same time, multiple unmet needs were identified, including access to oral health knowledge, services, daily care support, and environmental improvements. While negative experiences undermined motivation, patients would be more likely to engage in proactive oral health practices with more comprehensive support.
Dissatisfaction with oral health management
The majority of patients expressed dissatisfaction with OHM as the absence of adequate support and guidance diminished their motivation to maintain proper oral hygiene. In particular, patients highlighted the lack of systematic support at the institutional level, insufficient involvement of medical staff, and limited access to appropriate facilities, resources, and knowledge.
A5: “I ain’t doing too good with taking care of my own teeth. After all, I ain’t no professional in dentistry…”.
A12: “I’m not too happy with the hospital’s oral health care. I currently have some oral problems, but they still cannot be resolved in time….”
Unmet needs
Deterioration or unchange in oral condition
The majority of patients reported that their oral health condition did not show noticeable improvement during hospitalization, and in some cases, it was perceived to have worsened.
A9: “I haven’t seen much improvement, maybe even got a bit worse. One of my teeth has started wiggling lately.”
Access to oral health knowledge
Many patients with LLD lack oral health knowledge and optimal oral hygiene practices, which to some extent owes to limited access to knowledge. Therefore, they wish to participate in oral health educational activities during hospitalization.
A3: “…I also hope someone can teach me some knowledge about oral health. After all, as an elderly people, I don’t know where to learn such information. I just brush our teeth in the ways I am familiar with, and I am not sure if it’s correct, let alone how to better protect our teeth.”
A12: “It is also advisable to carry out more oral health educational activities in hospital. Many people still do not know how to brush their teeth correctly, and some even damage their teeth due to improper brushing technique. It is ineffective and in vain to use incorrect brushing techniques even if they brush their teeth every day.”
Demand for oral health services
The interview results show that some patients hope to receive regular oral examinations and timely access to professional medical assistance when experiencing oral discomfort.
A3: “…I need doctors and nurses to regularly check and assess our oral conditions, and provide more effective oral care.”
A12: “It would be best to have regular oral examinations and timely repair treatments for dental caries, since it is often too late and causes unnecessary suffering when toothache occurs.”
Daily support and improvement of inpatient conditions
Some of the patients felt that there were many aspects of current oral health management that need to be improved, such as oral care skills, environment, and materials.
A3: “Oral care should be as thorough as actual tooth-brushing. I feel that wiping with cotton balls isn’t enough.”
A16: “…I think the environment of restrooms in hospital can still be improved. It would be best to add all the necessary facilities, especially adjust the water temperature of the faucets, as it’s extremely cold in winter otherwise. Additionally, there’s the issue of toothpicks. It is quite uncomfortable when you have food stuck in your teeth and there are no toothpicks available.”