In Northern Europe, the empirical antibiotic strategy for treating non-severe CAP in hospitalized patients is a ß-lactam antibiotic, with the addition of a macrolide or fluoroquinolone reserved only for severe cases or when there is a clinical suspicion of atypical pneumonia [10, 19]. Our objective was to determine when to suspect the most common atypical pneumonia: Mycoplasma pneumoniae CAP by comparing it to pneumococcal CAP. Most importantly, M. pneumoniae was overrepresented in patients below 50 years of age and more frequently associated with experienced antibiotic failure before hospital admission. Clinical symptoms and radiographic findings were insufficient to discriminate between the two pathogens, but inflammatory laboratory results, especially WBC count, could provide guidance.
The strengths of our study are its prospective design and comprehensive testing, which made missed M. pneumoniae cases unlikely in the cohort. One limitation, however, was the difficulty in including critically ill patients, which may have led to their underrepresentation. In addition, the requirement to provide a urine sample as an inclusion criterion excluded anuric patients with acute kidney injury or end-stage renal disease. We chose to exclude cases that were only positive for S. pneumoniae in upper respiratory tract samples due to the difficulty to discriminate between colonization and infection. This may have led to an underrepresentation of S. pneumoniae cases. Finally, despite extensive testing, the number of detected M. pneumoniae cases was low, suggesting an endemic setting in which selecting patients for sampling from a resource-saving perspective can be more challenging.
Streptococcus pneumoniae was as expected, a far more common finding, with M. pneumoniae accounting for only 6% of all hospitalized CAP cases during a non-epidemic period, in line with other studies [7,8,9]. The most prominent difference between the two pathogens was the age disparity, with a median age of 36 years for M. pneumoniae and 70 years for pneumococcal CAP. Similar median ages of 39–43 years were reported in four European studies on M. pneumoniae CAP [20,21,22,23]. However, Dumke et al. included out-patients, and Metsälä et al. included children, both of which would lower the median age [21, 24]. In addition, three of these studies were retrospective, potentially leading to missed cases. In our cohort, 97% of all CAP patients were tested for M. pneumoniae and only two cases (6%) were detected in patients over 65 years, one of whom improved despite inadequate treatment. A prospective Japanese study using serology found that 15% of patients with detected M. pneumoniae were over 60 years old, while a retrospective Israeli study on PCR-positive patients reported that 17% of patients were over 65 years old [6, 25]. Both studies covered long time periods (6–15 years), likely including epidemic years, which could explain these findings. Further, relying on serology has limitations especially if only a single measurement of IgG or IgM is made, in the cited study however, both acute and convalescent sera were taken.
Fever, malaise, cough and dyspnoea were the most common symptoms of M. pneumoniae CAP. Dyspnoea and pleuritic pain were the only symptoms significantly more common in M. pneumoniae patients than in those with pneumococcal CAP, and also more common compared to all-cause CAP, interestingly since pleuritic pain has been considered a more specific sign of pneumococcal CAP [26]. Laboratory findings showed differences between the two pathogens with significantly lower CRP and WBC levels for M. pneumoniae compared to CAP caused by S. pneumoniae. Despite this, the CRP level in M. pneumoniae cases was still elevated with a median value of 178 mg/L at admission, similar to findings from a retrospective study on hospitalized CAP patients [22], suggesting that CRP-levels alone have limited value for diagnosing M. pneumoniae. In 75% of M. pneumoniae cases, WBC levels at admission were below 12.5 × 109/L, whereas in 75% of pneumococcal CAP, WBC levels exceeded 12.1 × 109/L at admission.
Radiographic findings in our cohort of hospitalized patients suggest that M. pneumoniae can present with a variety of appearances. Unilateral lobar consolidation was the most common finding, while patchy, interstitial, and vague opacities as well as bilateral abnormalities, were also observed. Studies focusing on radiology have found that bronchial wall thickening and centrilobular nodes are more indicative of M. pneumoniae than pneumococcal pneumonia [27]. However, this was not noted in our study as chest X-rays, rather than computed tomography, were used in most cases, further, a large retrospective French study also found that the radiographic imaging in M. pneumoniae CAP was highly polymorphic [23]. The most common radiographic finding in our study for pneumococcal CAP was unilateral consolidation; however, bilateral findings, interstitial patterns, and vague or small opacities were also observed, as previously described [28].
In this study, M. pneumoniae patients had significantly lower CRB scores and PSI grades. The majority of hospitalized patients with M. pneumoniae CAP required oxygen, and those in the M. pneumoniae group were treated with significantly higher oxygen levels than patients with pneumococcal pneumonia. Few patients in either group underwent HFNC-therapy, likely due to data collection occurring before the COVID-19 pandemic, after which HFNC usage has increased. It is expected that this therapy would now be more prevalent in both patient groups.
Only few patients with CAP caused by S. pneumoniae underwent mechanical ventilation or non-invasive ventilation, and none of the M. pneumoniae patients did. Previous studies have shown varying results regarding disease severity: three studies reported no mortality in analogy with our results [20, 21, 27], while two studies found two cases of death [22, 29]. Another investigation showed 6% mortality, with 16% of patients admitted to the ICU and 9% requiring mechanical ventilation [6]. In a retrospective Swedish study involving 388 patients, 8% of PCR-positive M. pneumoniae patients were admitted to the ICU, and one person died [22], and in a French recent observational report more than 30% were admitted to the ICU, and a total in hospital mortality of 2%, it was however noted that HFNC-treatment were only administered in the ICU which likely explained the high ICU-admission rates [23].
Patients with M. pneumoniae CAP had a longer duration of illness before hospitalization and were more likely to have been prescribed antibiotics within two weeks of admission. This frequent prescription of antimicrobial drugs was anticipated, as the first line treatment for CAP in Sweden for outpatients is penicillin V, which targets pneumococci but is ineffective against M. pneumoniae, which lacks a cell wall [10]. Viral co-detection was significantly more common in pneumococcal CAP compared to M. pneumoniae CAP. A study by Diaz et al. had a similar rate of 10% viral co-detections [30], suggesting that M. pneumoniae as an etiology is not a common cause of superinfection.
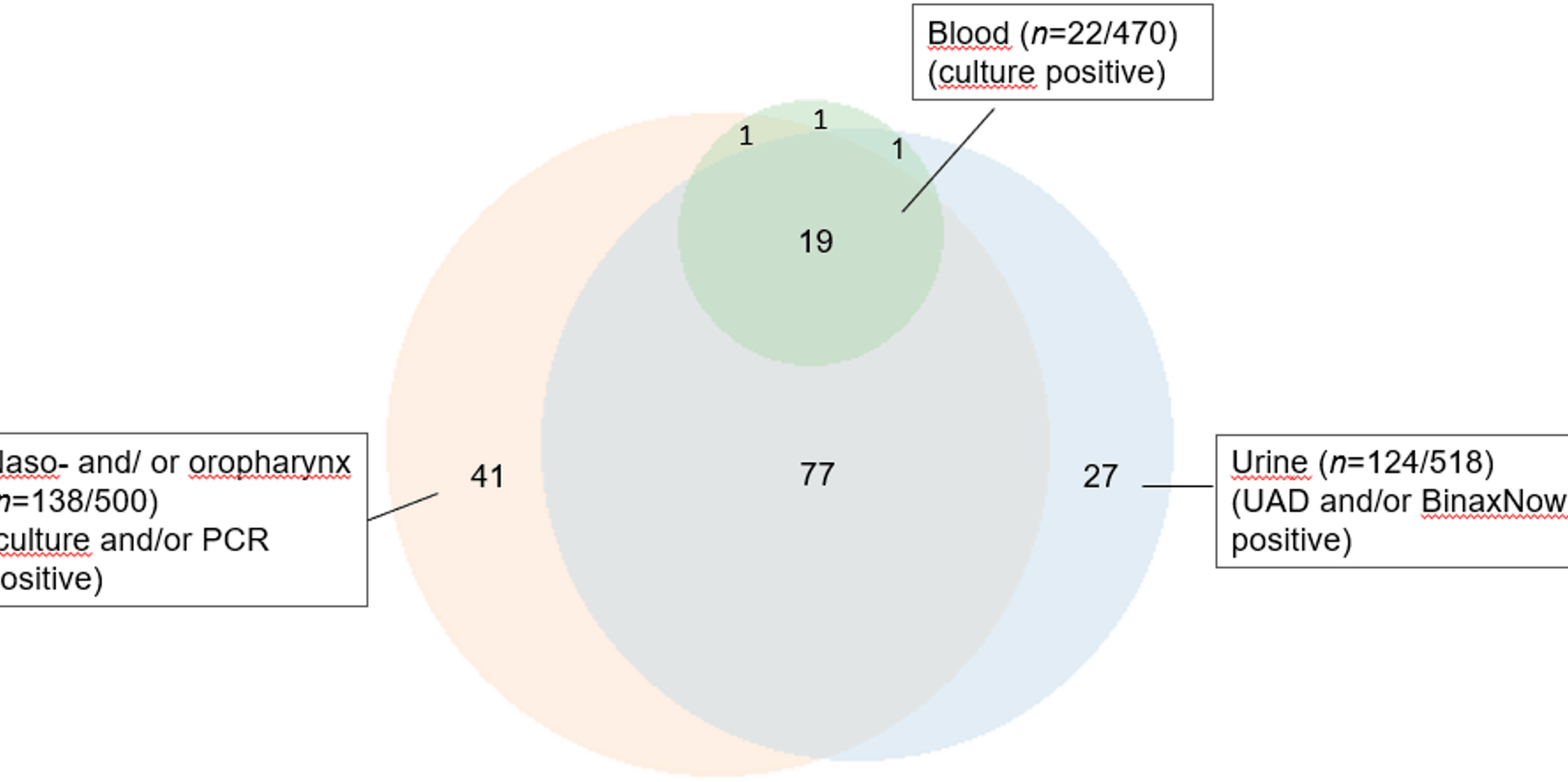
We found that during an endemic period, 27% of all hospitalized CAP patients underwent testing for M. pneumoniae based on clinical suspicion. When the entire cohort was tested, only two additional cases were confirmed in the previously untested group. However, three cases from routine sampling were false negative, while one patient tested positive in routine sampling but negative in the per protocol sampling, emphasizing that a test is only as reliable as the quality of the sample. The delay in effective treatment, however, did not affect the outcome. While a carrier state is not uncommon in children [31], we have previously found that M. pneumoniae is a rare finding in asymptomatic adults [14].