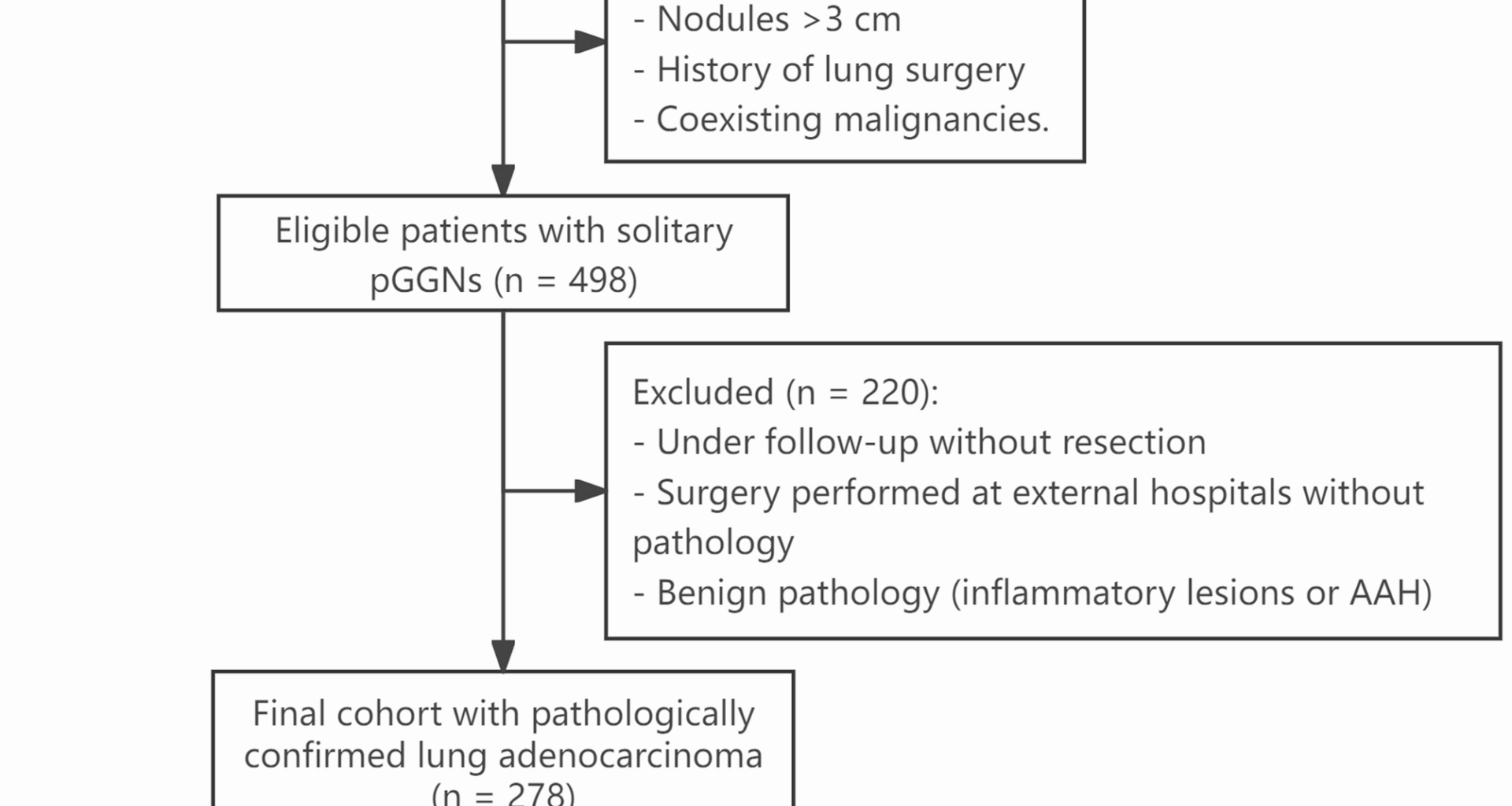
In this retrospective analysis of 278 individuals with solitary pGGNs pathologically verified as lung adenocarcinoma following surgery, an elevated TyG index was associated with invasive tumor features. Although the overall crude comparison of ILA prevalence across tertiles did not reach statistical significance (P = 0.190, Table 1), regression analyses revealed that participants in the highest TyG tertile had increased odds of ILA compared with those in the lowest tertile, particularly after multivariable adjustment (OR = 2.9, 95% CI: 1.16–7.23, Table 2). Subgroup analyses indicated that this association was generally consistent across clinical strata. Nonetheless, given the modest sample size and reliance on retrospective data, these results should be interpreted as exploratory and require confirmation in larger, prospective cohorts. As this study aimed to assess associations rather than to construct predictive models, we did not conduct calibration or decision-curve analyses, which will be valuable in future predictive modeling efforts.
Table 2 Associations between TyG and ILA in the multiple regression model
Our findings align with those of prior research, highlighting the role of IR and metabolic dysfunction in tumor development and progression. In addition to the TyG index’s association with NSCLC risk demonstrated by Yan et al. [10], similar associations have been observed in other cancer types. For instance, high TyG levels have been linked to an increased risk of colorectal [9, 17] and breast cancers [18], underscoring the broader oncogenic potential of IR-related markers. IR can enhance cell proliferation and suppress apoptosis via hyperinsulinemia, inflammatory cytokines, and IGF-1 signaling pathways, creating a pro-tumorigenic microenvironment [19, 20]. Notably, the null association reported by Wang et al. [11] in the UK Biobank pertains to incident lung cancer risk in a predominantly Caucasian community cohort that excluded participants with diabetes or dyslipidemia and did not stratify by histological subtype or invasiveness. In contrast, our study addresses pathological invasiveness among surgically resected pGGNs—a clinically selected population in which metabolic profiles may differentially relate to tumor behavior rather than disease initiation. Furthermore, studies in patients undergoing screening or surgery have suggested that metabolic status could influence tumor phenotype, although few have specifically addressed pGGNs [4]. By focusing on early stage lung adenocarcinoma with ground-glass opacity, our study provides novel evidence suggesting that elevated TyG may not only reflect systemic metabolic dysfunction but also be associated with greater tumor invasiveness.
This study had several methodological strengths that enhanced the reliability and relevance of its findings. First, by focusing exclusively on patients with solitary pGGNs confirmed as lung adenocarcinoma through surgical pathology, we minimized histological heterogeneity and ensured accurate classification of invasiveness. This strict case definition contrasts with that of prior large-scale population studies, which typically rely on cancer registries or radiologic suspicion, potentially leading to misclassification [21]. Second, the use of multiple logistic regression models with progressive adjustments allowed us to rigorously account for key confounders, including tumor size, laterality, and circulating tumor markers such as carcinoembryonic antigen (CEA) and CA-125, which have been linked to tumor aggressiveness [22,23,24]. Third, subgroup analysis demonstrated the robustness of the TyG-ILA association across clinical strata, suggesting that the finding was not driven by a specific subgroup. Furthermore, missing data were addressed using multiple imputation via chained equations (MICE) in Python, a validated statistical method that preserves the integrity of the variable associations without introducing selection bias [25]. Taken together, these methodological elements lend confidence to our conclusion that the TyG index is independently associated with histological invasiveness in early stage lung adenocarcinoma presenting as pGGNs.
The TyG index serves as an indirect indicator of IR, capturing abnormalities in glucose metabolism and lipid profiles. These metabolic disturbances may contribute to tumor-promoting conditions by enhancing inflammatory responses, increasing oxidative damage, and disrupting key cell signaling pathways [26, 27]. Hyperinsulinemia and elevated free fatty acids, frequently observed in insulin-resistant states, have been shown to promote epithelial-mesenchymal transition (EMT) and angiogenesis, both of which are critical for tumor invasion and metastasis [28,29,30,31]. Mechanistically, hyperinsulinemia can activate insulin receptor and IGF-1 receptor signaling, engaging PI3K/AKT and MAPK cascades that drive proliferation, inhibit apoptosis, and facilitate matrix degradation and cell motility [32]. In addition, increased uptake of free fatty acids through transporters such as CD36 has been implicated in fueling EMT-like changes that enhance tumor cell invasiveness [33, 34]. Hyperinsulinemia has also been associated with endothelial activation and upregulation of angiogenic mediators such as Angiopoietin-2 and VEGF, which remodel the tumor vasculature and promote stromal invasion [35]. In lung tissue, IR may activate oncogenic pathways, such as PI3K/Akt and MAPK, enhancing cellular proliferation and resistance to apoptosis [36, 37]. Additionally, metabolic dysregulation can influence the tumor microenvironment by modulating immune cell infiltration and cytokine release [38, 39], thereby facilitating the invasive transformation of early stage lesions. These mechanisms may partly explain the stronger association between the TyG index and ILA observed in our cohort, although further mechanistic studies are needed to substantiate these hypotheses.
This study has several limitations. First, its retrospective and cross-sectional design limits the ability to infer causality between the TyG index and tumor invasiveness, and prospective studies are needed to confirm this association. Second, This study was conducted at a single center in an East Asian population, which may limit generalizability. However, given that East Asian lung adenocarcinoma exhibits a higher prevalence of ground-glass nodules and EGFR mutations—features less common in Western cohorts [40], suggesting that our findings remain clinically relevant in this specific context, although multicenter and multiethnic validation is warranted. Third, although adjustments were made for major clinical and metabolic covariates, residual confounding due to unmeasured factors—such as medication use (e.g., statins, metformin), physical activity, nutritional status, or direct measures of insulin resistance (HOMA-IR, fasting insulin)—may still exist. In particular, while C-reactive protein (CRP) would have been an informative inflammatory marker, more than half of these data were missing, making it unsuitable for inclusion. Similarly, although smoking status was incorporated, detailed pack-year history was not available due to the retrospective nature of the study. These limitations highlight the need for more comprehensive data collection in future prospective investigations. Finally, this study focused on surgically resected lung adenocarcinomas, potentially introducing selection bias by excluding indolent nodules under active surveillance.
From a clinical perspective, the TyG index is readily obtainable from routine laboratory data and incurs no additional cost or testing burden. In the context of pulmonary nodules—particularly pGGNs with indeterminate invasive potential—TyG may serve as a supplementary biomarker during the preoperative evaluation phase. Although not currently a standard component of oncologic risk assessment, its potential utility lies in refining malignancy risk stratification, especially in metabolic at-risk populations such as individuals with obesity, prediabetes, or metabolic syndrome. At present, we suggest that TyG testing may be selectively informative in patients undergoing work-up for pGGNs where radiologic findings are equivocal. However, before clinical implementation, prospective studies are needed to establish reproducibility, define optimal thresholds, and determine whether TyG provides incremental value beyond existing clinical and imaging tools.