Baseline characteristics of studies included in the meta-analysis
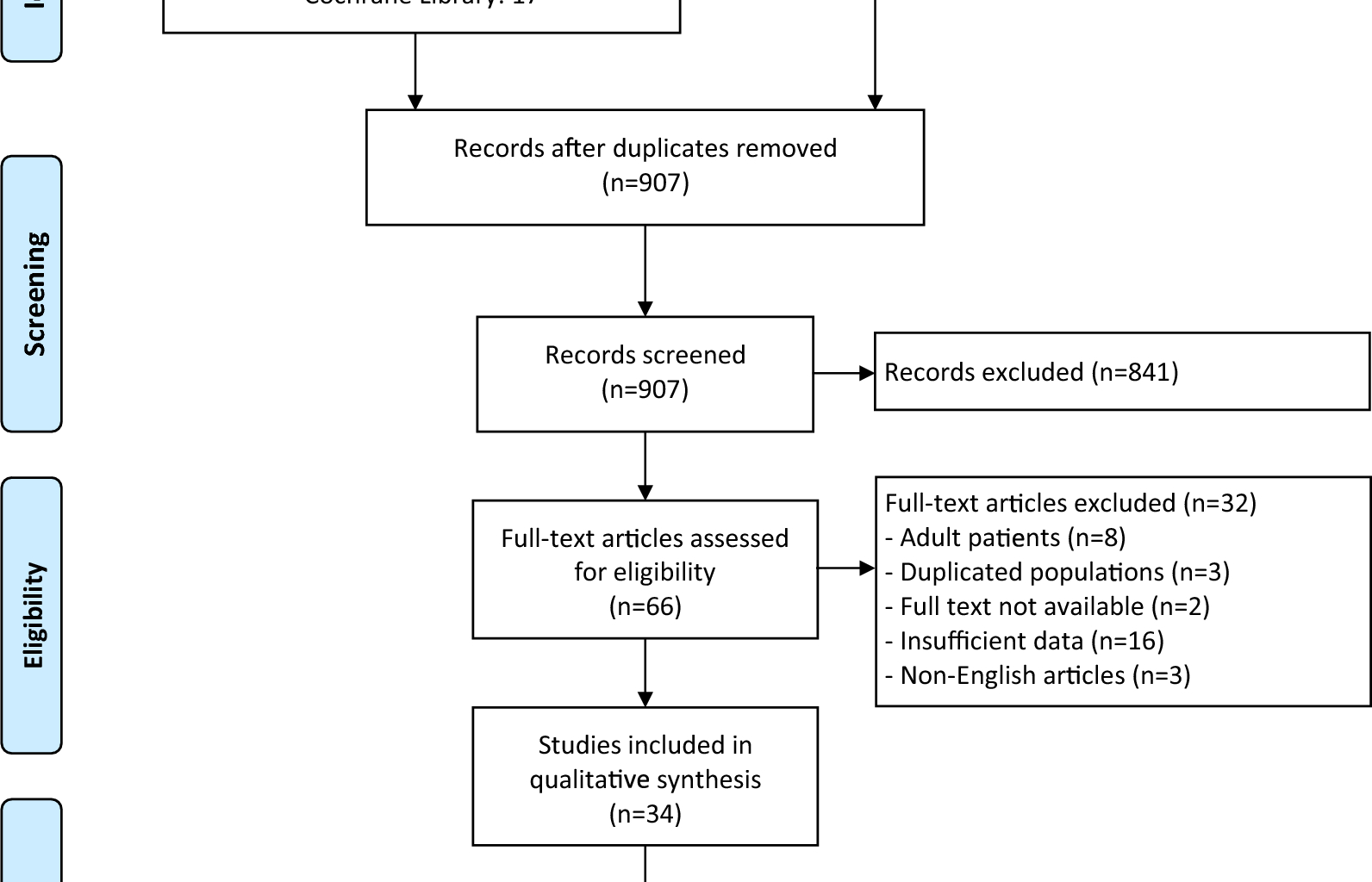
The comprehensive literature search identified 1698 articles, of which 907 unique article remained after removing duplicates (Fig. 1). Following title and abstract screening, 841 irrelevant articles were excluded, and 32 full-text articles were further excluded based on eligibility criteria (Additional file 1: Table S2). The kappa coefficient was 0.819 at title/abstract screening stage and 0.909 at full-text reviewing stage, indicating a high level of inter-reviewer agreement. Ultimately, 34 studies involving 1332 pediatric patients (1340 fractured hips) were included in the meta-analysis [4, 5, 13,14,15,16, 22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49]. Sample sizes ranged from 8 to 241. The included studies were conducted across various countries: the United States (n = 9), China (n = 6), India (n = 6), Turkey (n = 6), Austria (n = 1), Canada (n = 1), Saudi Arabia (n = 1), Serbia (n = 1), Egypt (n = 1), Germany (n = 1), and the United Kingdom (n = 1). Five studies were published before 2000, 11 between 2000 and 2010, and 18 after 2010. There were 20 case–control studies and 14 case-series studies [4, 22,23,24, 28, 31,32,33,34, 36, 37, 40, 45, 46].
Flowchart of literature search and selection
Across all studies, the number of AVN cases ranged from 1 to 59, which summed up to 372. The incidence of AVN varied from 5.6 to 64.4%. The incidence ranged from 5.6% to 52.9% in case-series studies and from 11.4 to 64.4% in case–control studies, without significant difference between these two study types. According to the Delbet classification, the distribution of fracture types was as follows: type I (n = 60), type II (n = 700), type III (n = 454), and type IV (n = 125). Mean follow-up durations ranged from 1 to 17 years. Eight potential risk factors were analyzed for their association with AVN: gender, age, Delbet classification, initial displacement, injury mechanism, time to reduction, reduction method, and reduction quality. All included case–control studies were deemed high quality based on NOS assessment. The mean IHE checklist point for case-series studies was 10.6 (range: 8–14), suggesting a fair methodological quality. Detailed baseline characteristics, analyzed risk factors, and quality assessments are summarized in Table 1.
Table 1 Baseline characteristics of studies included in the meta-analysisGender
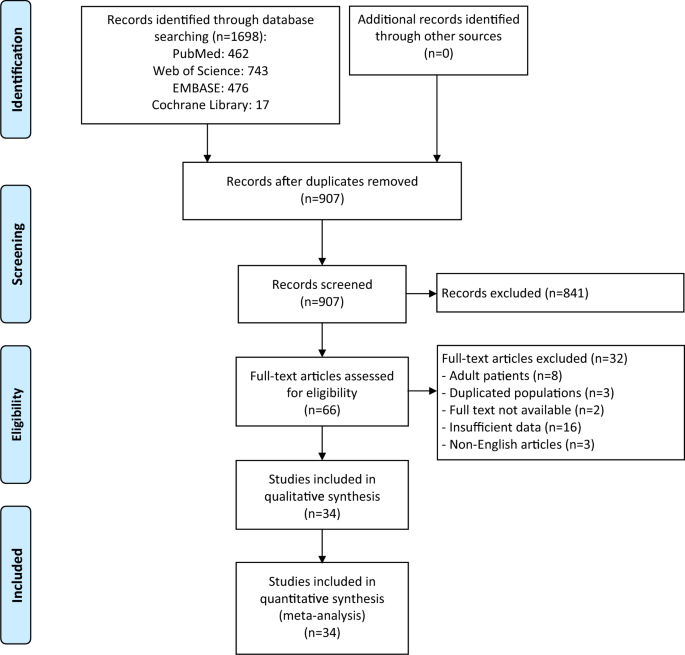
Twenty-two studies involving 646 fractures evaluated the association between gender and AVN risk. No heterogeneity was observed (I2 = 0%, P = 0.714), allowing the use of a fixed-effects model. The risk of AVN did not differ significantly between male and female patients (RR = 0.79, 95% CI 0.61–1.03, Fig. 2).
Forest plot of meta-analysis of association between gender and risk of avascular necrosis in pediatric femoral neck fractures
Age
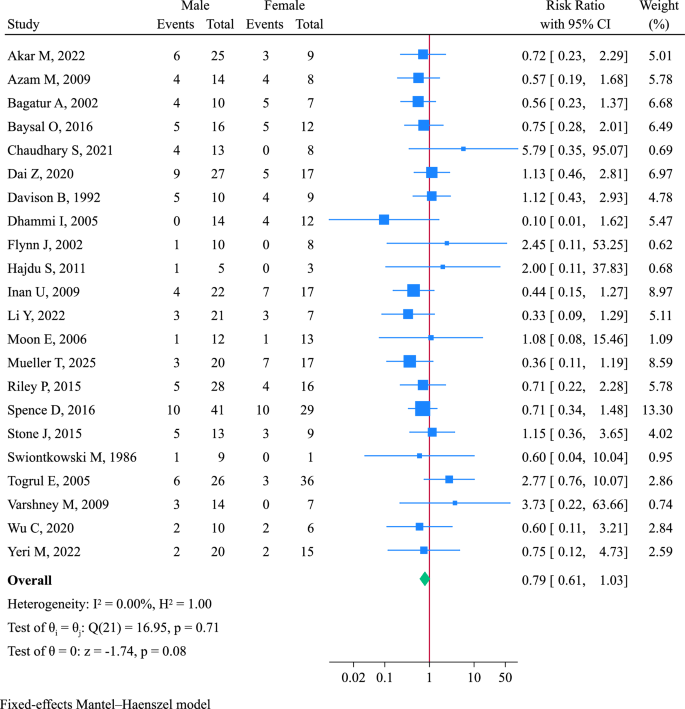
Seventeen studies (660 fractures) assessed the impact of age on AVN risk. Pooled analysis using a fixed-effects model indicated that patients aged ≥ 12 years had a significantly higher risk of AVN than those aged < 12 years (RR = 1.40, 95% CI 1.09–1.82, Fig. 3).
Forest plot of age associated with avascular necrosis in pediatric femoral neck fractures
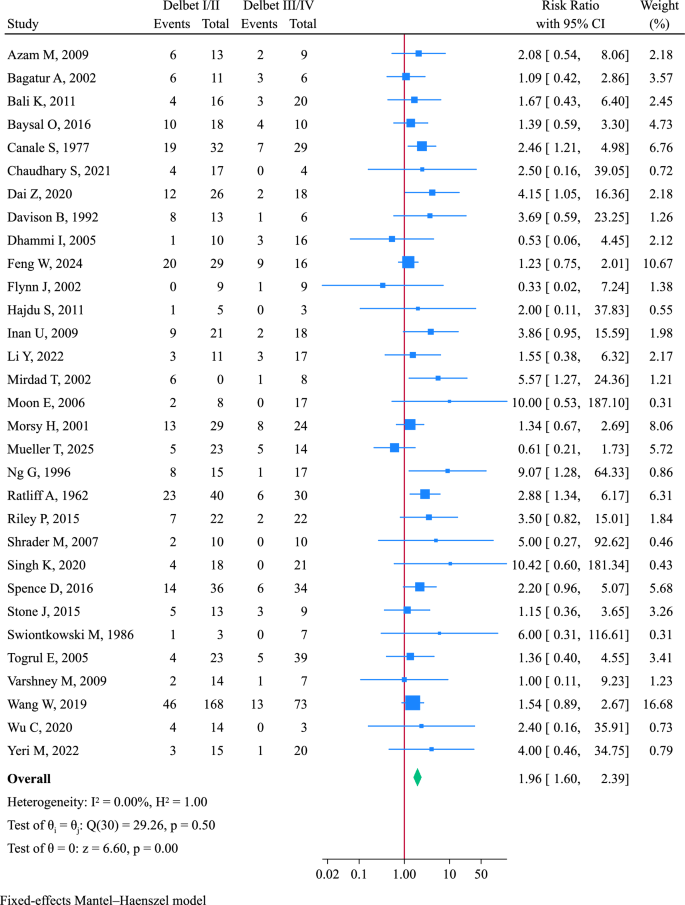
Delbet classification
A total of 31 studies (1224 fractures) compared AVN risk between Delbet type I/II and type III/IV fractures. Type I/II fractures were associated with a significantly higher risk of AVN (RR = 1.96, 95% CI 1.60–2.39, I2 = 0, Fig. 4). Further comparison between Delbet type II and III fractures was performed using data from 28 studies (802 fractures). Type II fractures carried a significantly higher AVN risk than type III fractures (RR = 1.73, 95% CI 1.38–2.18, Additional file 2: Fig. S1).
Forest plot of Delbet classification associated with avascular necrosis in pediatric femoral neck fractures
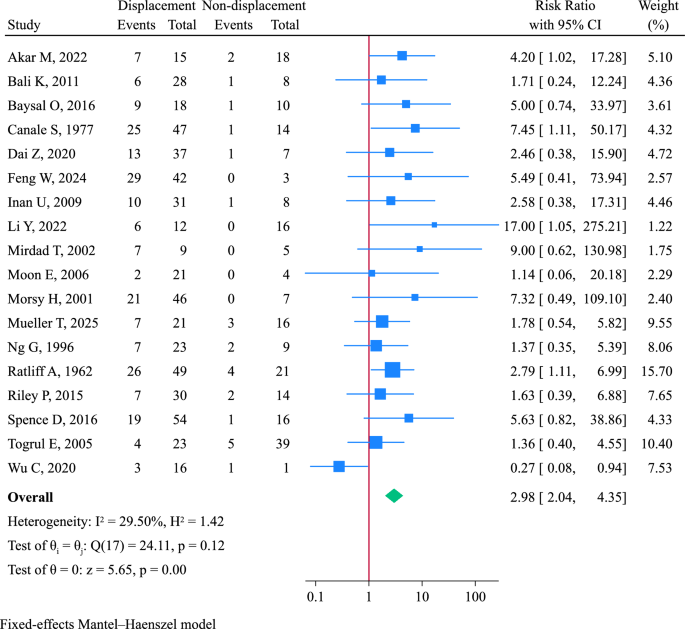
Initial displacement status
Eighteen studies involving 738 fractures analyzed the association between initial displacement and AVN. A fixed-effects model was used (I2 = 29.5%, P = 0.116). Displaced fractures had a significantly increased risk of AVN compared to non-displaced ones (RR = 2.98, 95% CI 2.04–4.35, Fig. 5).
Forest plot of initial displacement status associated with avascular necrosis in pediatric femoral neck fractures
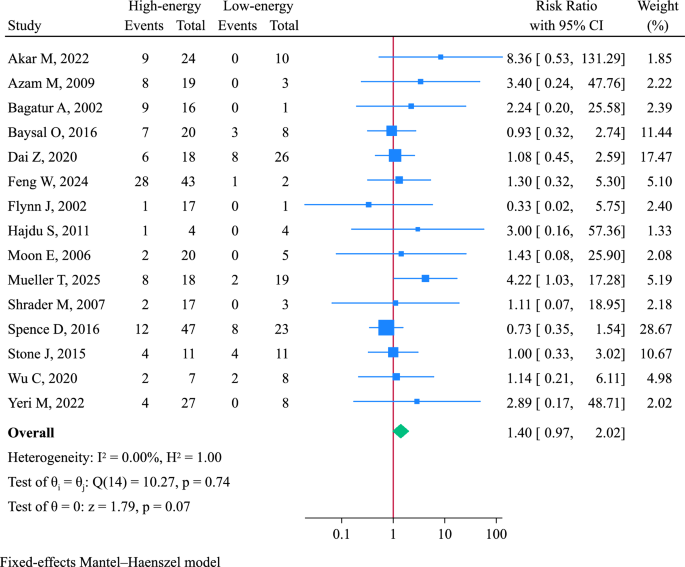
Injury mechanism
Fifteen studies (440 fractures) assessed the impact of injury mechanism. Mechanisms were categorized as high-energy (e.g., motor vehicle accidents, falls from height) or low-energy (e.g., sports injuries, falls during daily activities). No significant difference in AVN risk was found between the two groups (RR = 1.40, 95% CI 0.97–2.02, Fig. 6).
Forest plot of injury mechanism associated with avascular necrosis in pediatric femoral neck fractures
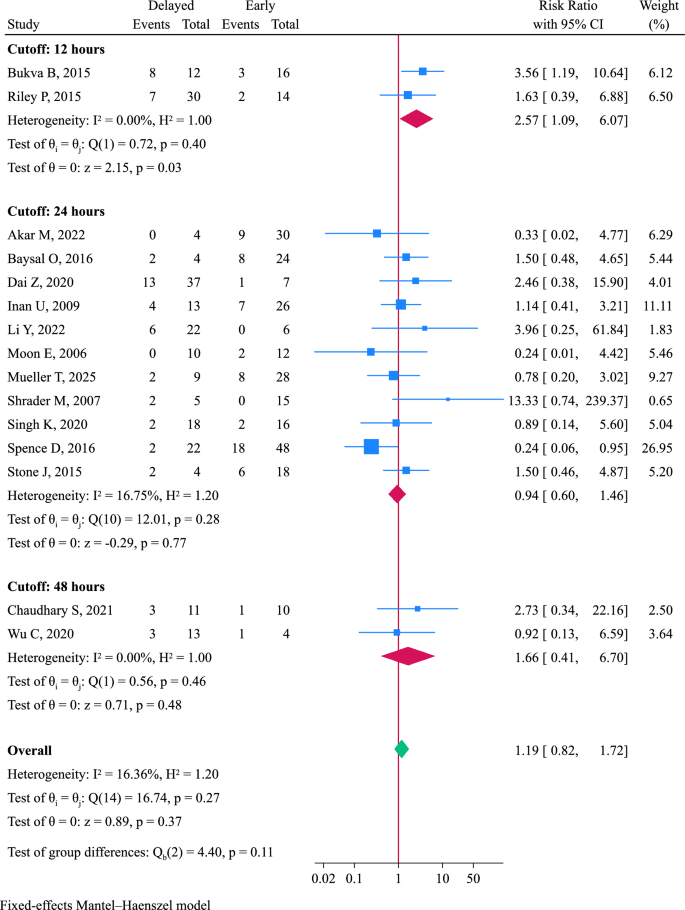
Time to reduction
Time to reduction was analyzed using three cutoffs: 12 h (n = 2), 24 h (n = 11), and 48 h (n = 2). Overall, pooled analysis with a fixed-effects model found no significant difference in AVN risk between delayed and early reduction (RR = 1.19, 95% CI 0.82–1.72, Fig. 7).
Forest plot of time to reduction associated with avascular necrosis in pediatric femoral neck fractures
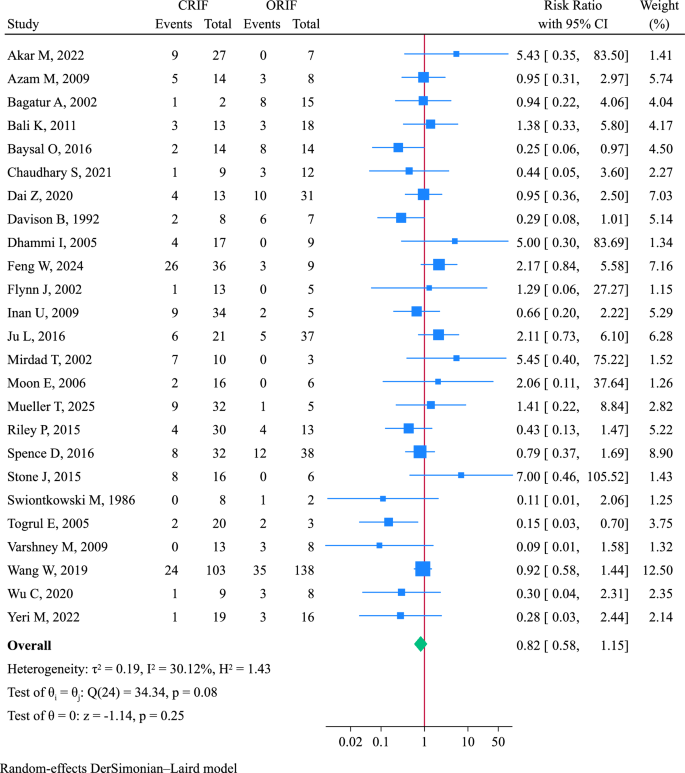
Reduction method
Twenty-five studies compared closed reduction and internal fixation (CRIF, n = 529) to open reduction and internal fixation (ORIF, n = 423). A random-effects model was employed for meta-analysis (I2 = 30.1%, P = 0.079). No significant difference in AVN risk was found between the two methods (RR = 0.82, 95% CI 0.58–1.15, Fig. 8).
Forest plot of reduction method associated with avascular necrosis in pediatric femoral neck fractures. CRIF: closed reduction and internal fixation; ORIF: open reduction and internal fixation
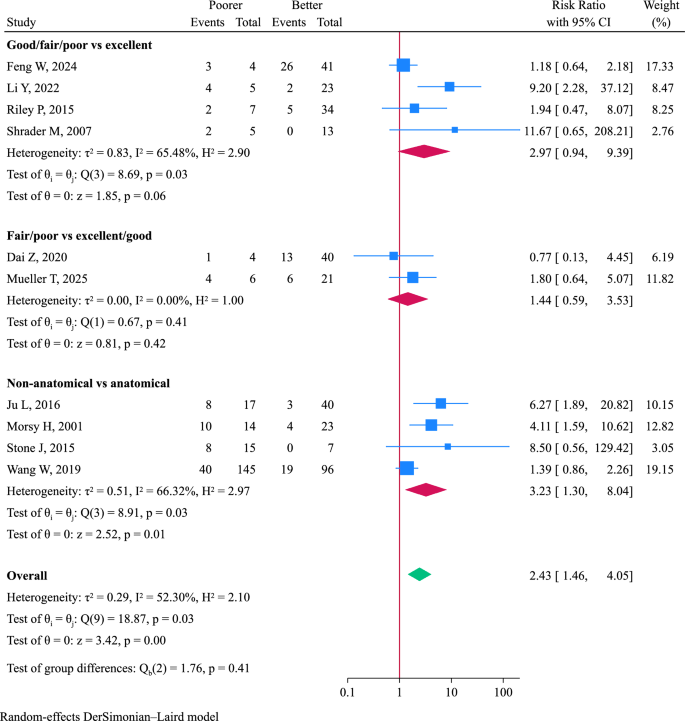
Reduction quality
Ten studies assessed the association between reduction quality and AVN, using either anatomical versus non-anatomical classification or the Haidukewych criteria (excellent/good/fair/poor) [50]. Meta-analysis with a random-effect model (I2 = 52.3%, P = 0.020) showed that poorer reduction quality was significantly associated with increased AVN risk (RR = 2.43, 95% CI 1.46–4.05, Fig. 9).
Forest plot of reduction quality associated with avascular necrosis in pediatric femoral neck fractures
Sensitivity analysis
Sensitivity analysis using a leave-one-out approach indicated that pooled results for gender, age, injury mechanism, and time to reduction lacked robustness. Exclusion of Wang W et al. rendered the association between age and AVN non-significant (RR = 1.25, 95% CI 0.91–1.71, Additional file 2: Fig. S2) [13]. Conversely, excluding Chaudhary et al. or Togrul et al. resulted in a significant association between gender and AVN risk (Additional file 2: Fig. S3) [29, 46]. Omitting Spence et al. also changed the results for injury mechanism and time to reduction from non-significant to significant (Additional file 2: Figs. S4 and S5) [43].
Meta-regression and subgroup analysis
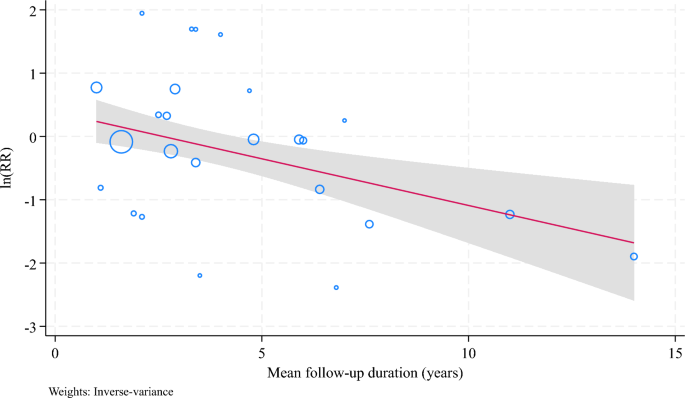
Meta-regression was conducted to identify moderators of risk factor–AVN associations, including publication year, sample size, mean age, follow-up duration, and proportions of male patients, Delbet type I/II fractures, displaced fractures, CRIF procedures, high-energy injuries, and early reduction (Additional file 1: Table S3. Publication year was negatively associated with the effect size for Delbet classification (P = 0.031). Follow-up duration emerged as a significant moderator for gender (P = 0.046, Additional file 2: Fig. S6), time to reduction (P = 0.047, Additional file 2: Fig. S7), and reduction method (P = 0.001, Fig. 10).
Meta-regression of mean follow-up duration modulating the association of reduction method with avascular necrosis in pediatric femoral neck fractures. RR: risk ratio
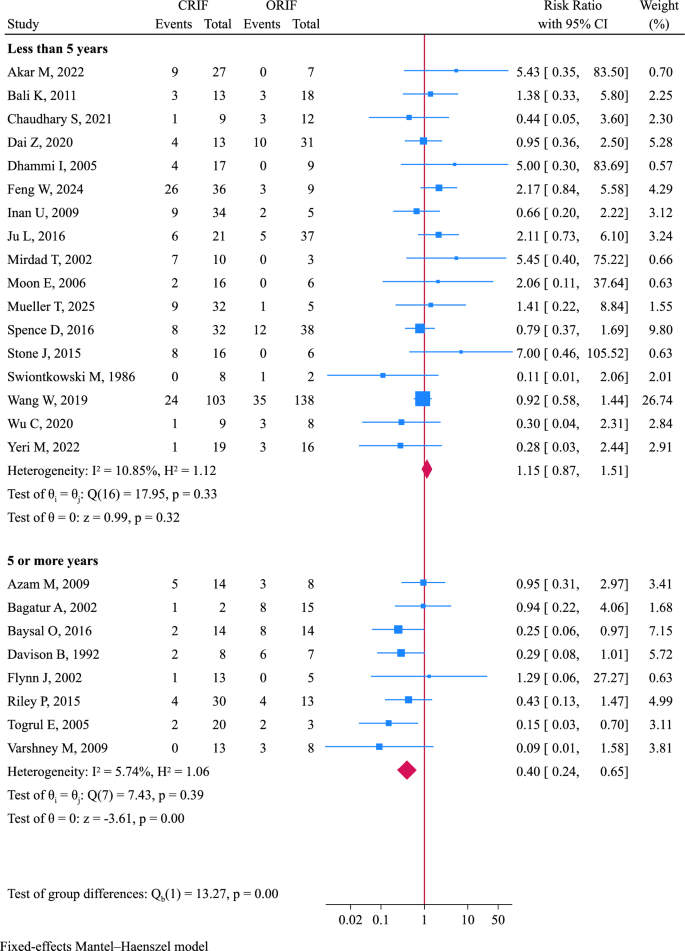
Studies were divided into short-term (< 5 years) and long-term (≥ 5 years) follow-up (Additional file 1: Table S4). In the long-term subgroup, delayed reduction significantly increased AVN risk (RR = 2.63, 95% CI 1.35–5.11, Additional file 2: Fig. S8), and CRIF was associated with lower AVN risk compared to ORIF (RR = 0.40, 95% CI 0.24–0.65, Fig. 11). These effects were not observed in short-term follow-up. The subgroup differences were statistically significant for both factors (P = 0.007 and P < 0.001, respectively). No significant subgroup effects was observed for gender (P = 0.175).
Forest plot of subgroup analysis of reduction method associated with avascular necrosis stratified by mean follow-up duration. CRIF: closed reduction and internal fixation; ORIF: open reduction and internal fixation
Publication bias
Potential publication bias was suggested by Egger’s test for Delbet classification, initial displacement, and reduction quality (P < 0.05, Additional file 1: Table S5). Trim-and-fill analysis showed that the results remained significant for Delbet classification (RR = 1.60, 95% CI 1.32–1.94, Additional file 2: Fig. S9) and reduction quality (RR = 2.05, 95% CI 1.22–3.42, Additional file 2: Fig. S10). However, the effect size for initial displacement was reduced from RR = 2.98 to RR = 1.76 (95% CI 1.24–2.51) after trim-and-fill analysis (Additional file 2: Fig. S11).
Certainty of evidence
The evidence starts at low certainty since all included studies were observational studies. The final judgement was low certainty of evidence for gender, age, Delbet classification (II vs. III), injury mechanism, and time to reduction, and very low certainty of evidence for Delbet classification (I/II vs. III/IV), initial displacement, reduction method, and reduction quality (Additional file 1: Table S6).