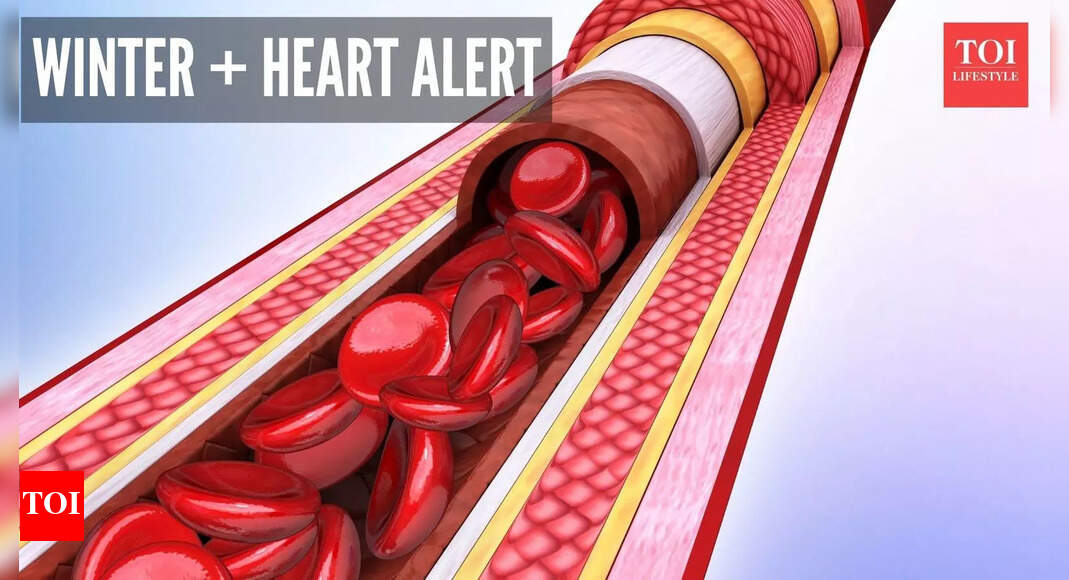
 When the temperature drops, the body uses a clever survival trick: it narrows its blood vessels to conserve heat, as per a 2019 study. That natural response sounds harmless, but inside the arteries, it can raise blood pressure and increase the risk for heart trouble in older people, those with high BP and underlying heart condition, As the cold hits and arteries tighten, the heart must pump harder to push blood through narrower passages.This extra load can pinch off that safe “normal” circulation and create strain. In winter, factors like less daylight, fewer outdoor steps and warmer (often heavier) meals tend to add to the mix, and for those already managing high blood pressure or heart conditions, this season brings a hidden danger. Understanding how and why arteries behave this way during the cold months, and taking clear, practical steps, can make the difference between a cosy winter and a risky one. Here’s the science of seasonal artery constriction, why it boosts risk, and 5 ways to stay safe as the mercury falls.What happens when arteries constrict in the coldWhen cold weather hits, the body triggers reflexes to maintain core temperature, as mentioned by the American Heart Association. One key reaction: smooth muscle in arterial walls tightens, causing vasoconstriction. The result: smaller vessel diameter, increased vascular resistance, and higher blood pressure. Studies show arterial constriction in cold conditions helps maintain body heat but also raises heart workload. Why this matters for blood pressureBecause vessels are narrower, the same volume of blood must be forced through more tightly. That elevates systolic and diastolic pressures, even in people without previously diagnosed hypertension. For example, experts note that low temperatures cause blood vessels to temporarily narrow, forcing more pressure. Seasonal studies show measurable increases in blood pressure during winter months.
When the temperature drops, the body uses a clever survival trick: it narrows its blood vessels to conserve heat, as per a 2019 study. That natural response sounds harmless, but inside the arteries, it can raise blood pressure and increase the risk for heart trouble in older people, those with high BP and underlying heart condition, As the cold hits and arteries tighten, the heart must pump harder to push blood through narrower passages.This extra load can pinch off that safe “normal” circulation and create strain. In winter, factors like less daylight, fewer outdoor steps and warmer (often heavier) meals tend to add to the mix, and for those already managing high blood pressure or heart conditions, this season brings a hidden danger. Understanding how and why arteries behave this way during the cold months, and taking clear, practical steps, can make the difference between a cosy winter and a risky one. Here’s the science of seasonal artery constriction, why it boosts risk, and 5 ways to stay safe as the mercury falls.What happens when arteries constrict in the coldWhen cold weather hits, the body triggers reflexes to maintain core temperature, as mentioned by the American Heart Association. One key reaction: smooth muscle in arterial walls tightens, causing vasoconstriction. The result: smaller vessel diameter, increased vascular resistance, and higher blood pressure. Studies show arterial constriction in cold conditions helps maintain body heat but also raises heart workload. Why this matters for blood pressureBecause vessels are narrower, the same volume of blood must be forced through more tightly. That elevates systolic and diastolic pressures, even in people without previously diagnosed hypertension. For example, experts note that low temperatures cause blood vessels to temporarily narrow, forcing more pressure. Seasonal studies show measurable increases in blood pressure during winter months. From higher pressure to heart-attack riskElevated blood pressure itself is a major risk factor for a heart attack. But during winter, it’s the combination of increased vessel resistance, possibly higher sympathetic nervous activity (stress-hormone driven), and reduced physical activity that creates a perfect storm. Some research links sudden cold exposure with triggering cardiovascular events. When the heart works harder over time, plaque instability, increased shear stress and oxygen demand may push vulnerable vessels into failure.Who’s especially vulnerablePeople with existing hypertension, heart disease, older age, and those whose bodies struggle to adapt to cold (for instance, people with poor circulation or diabetes) are at higher risk. It’s especially important for these groups to treat winter not just as a time of “more layers” but as a cardiovascular risk period. Moreover, habits like staying indoors, less exercise and weight gain add to risk.
From higher pressure to heart-attack riskElevated blood pressure itself is a major risk factor for a heart attack. But during winter, it’s the combination of increased vessel resistance, possibly higher sympathetic nervous activity (stress-hormone driven), and reduced physical activity that creates a perfect storm. Some research links sudden cold exposure with triggering cardiovascular events. When the heart works harder over time, plaque instability, increased shear stress and oxygen demand may push vulnerable vessels into failure.Who’s especially vulnerablePeople with existing hypertension, heart disease, older age, and those whose bodies struggle to adapt to cold (for instance, people with poor circulation or diabetes) are at higher risk. It’s especially important for these groups to treat winter not just as a time of “more layers” but as a cardiovascular risk period. Moreover, habits like staying indoors, less exercise and weight gain add to risk.
In winter, the blood vessels usually constrict due to the cold; this may elevate blood pressure and increase the risk of heart attacks, especially in cases of pre-existing heart disease or hypertension, the fall in temperature can increase the workload on the heart to pump blood. Lower levels of physical activity, heavier food intake, and dehydration in winter add to the load on the cardiovascular system. People with diabetes, high cholesterol, or leading a sedentary life should be more cautious. The tips to be safe are keeping warm, dressing in layers, and avoiding sudden exposure to cold air. Consume a balanced diet high in fruits, vegetables, and omega-3 fats, with minimal overeating or excessive alcohol intake. Lastly, indoor light exercises, adequate hydration, and blood pressure monitoring play their part. The medication should be taken as prescribed and the doctor consulted if any symptoms like chest discomfort, shortness of breath, or dizziness appear. A little precaution and awareness can go a long way in reducing the burden of winter cardiac events.
Dr Varun Bansal, consultant cardiac surgeon at Indraprastha Apollo Hospitals
Tip: Warm-up transitions when you go outsideInstead of stepping straight from a heated room into bitter cold, pause for a brief “transition” indoors: open a window slightly, stand in a cooler corner, drink a warm non-caffeinated beverage. This gives the body a chance to adjust and reduces the shock to the vessels. The sharper the temperature drop, the stronger the vasoconstriction effect. Research from 2018 shows skin cooling rapidly causes immediate blood pressure responses. Find your indoor rhythm: gentle movement + layeringWhen it’s cold out, skip the standard gym slog outside. Instead build mini-movement into your indoor routine: a 5-minute brisk walk in place, arm swings while heating up, some dynamic stretches in the living room. Pair this with dressing in layers so you avoid heavy outerwear that hampers movement, aim for outfits that keep you comfortably mobile. Being active helps keep vessels more dilated and reduces the hold of vasoconstriction.Choose winter-smart nutrition for your vesselsInstead of just “eat healthy”, pick foods that help resist the cold-triggered pressure rise. For example, foods rich in nitrate (like beetroot), potassium-rich winter veggies (sweet potato, squash) and fair amounts of magnesium (nuts/seeds) help vascular relaxation. Also, avoid over-salting just because festive meals and winter comfort food invite it; salt heightens fluid retention and vascular load, which compounds the constriction effect.Monitor more frequently, and tweak habits nowBecause seasonal blood-pressure rises are real, using a home BP monitor during winter is wise. Many clinics note that BP tends to rise in colder months and may need medication adjustment. Keep a log, note readings after being outdoors or after heavy meals, and if you see consistent upticks, talk to your doctor. It’s not about panic, but about catching subtle shifts so you don’t end up in “surprise spike” territory.Disclaimer: This article is for informational purposes only and does not replace medical advice. If you have high blood pressure, heart disease or related conditions, consult a qualified healthcare professional before making changes to your diet, exercise, or medication.
Find your indoor rhythm: gentle movement + layeringWhen it’s cold out, skip the standard gym slog outside. Instead build mini-movement into your indoor routine: a 5-minute brisk walk in place, arm swings while heating up, some dynamic stretches in the living room. Pair this with dressing in layers so you avoid heavy outerwear that hampers movement, aim for outfits that keep you comfortably mobile. Being active helps keep vessels more dilated and reduces the hold of vasoconstriction.Choose winter-smart nutrition for your vesselsInstead of just “eat healthy”, pick foods that help resist the cold-triggered pressure rise. For example, foods rich in nitrate (like beetroot), potassium-rich winter veggies (sweet potato, squash) and fair amounts of magnesium (nuts/seeds) help vascular relaxation. Also, avoid over-salting just because festive meals and winter comfort food invite it; salt heightens fluid retention and vascular load, which compounds the constriction effect.Monitor more frequently, and tweak habits nowBecause seasonal blood-pressure rises are real, using a home BP monitor during winter is wise. Many clinics note that BP tends to rise in colder months and may need medication adjustment. Keep a log, note readings after being outdoors or after heavy meals, and if you see consistent upticks, talk to your doctor. It’s not about panic, but about catching subtle shifts so you don’t end up in “surprise spike” territory.Disclaimer: This article is for informational purposes only and does not replace medical advice. If you have high blood pressure, heart disease or related conditions, consult a qualified healthcare professional before making changes to your diet, exercise, or medication.