Description of the study population
The sample consisted of 634 males and 20,648 females ranging in age from 10 to 89 years, with an average age of 41.177 ± 11.173 years. Table 1 shows the correlations between various age groups and different HPV types based on a total of 21,282 cases. The clinical manifestations of HPV infection are abdominal pain, abdominal tumours, allergic dermatitis, cervicitis, colpitis, cervical intraepithelial dysplasia (CIN)-I, CIN-II, CIN-III, common warts, eczema, erythema, genital warts, herpes, cervical cancer, ovarian cysts, and other diseases.
Table 1 Description of the study population for the association of different HPV infections in age groups
The sample included 126 cases of CIN-I, 78 cases of CIN-II, 130 cases of CIN-III and 101 cases of cervical cancer. A total of 27 HPV types were detected, including HPV6, 11, 15, 16, 18, 23, 31, 33, 35, 36, 38, 39, 42, 43, 44, 45, 51, 52, 53, 56, 58, 59, 61, 66, 68, 81, and 86. Among them, HPV16 infection was the most common and accounted for 7.65% of the total number of infections, followed by HPV52, 58, 53, 51, 39 and 18.
The data provided in the table indicate a notable disparity (p < 0.01, Table 1) between the distributions of high- and low-risk HPV positivity in different age groups, which, in combination with the division into age groups, facilitates a precise analysis of the changes in the prevalence of HPV infection at different stages of life.
Among the high-risk HPV types, HPV16, HPV18, HPV31, HPV33, HPV35, HPV39, HPV51, HPV56, HPV58, and HPV59 showed relatively high prevalences of infection during puberty, followed by a gradual decrease in the prevalence of infection with age. For example, HPV16 had the highest prevalence of 25.00% during adolescence, whereas the prevalence decreased significantly to 13.04% in old age. This difference may reflect the higher level of sexual activity in the younger population, which increases the risk of infection with high-risk HPV (Table 1).
In contrast, the prevalence of HPV45, HPV52 and HPV68 infections did not significantly differ by age group, suggesting that these types of infections may be less related to age and may be associated with other factors, such as sexual behaviour and immune status (Table 1).
Among the low-risk HPV types, the prevalence of HPV66, HPV6, HPV11, HPV43, HPV44, HPV15, and HPV81 significantly differed among the age groups. In particular, HPV6 and HPV11were more prevalent during adolescence, which may be related to the onset of sexual behaviour and the increase in the number of sexual partners during puberty. The prevalence of these HPV types decreases with age, which may be related to the maturation of the immune system and stabilization of sexual behaviour patterns.
The prevalence of HPV53, HPV42, HPV23, HPV36, HPV38, HPV61 and HPV86 did not differ significantly across age groups, suggesting that these types of infections may be influenced by other nonage-related factors (Table 1).
Comparison of sex ratios for HPV infection in different age subgroups
The distribution of HPV among males and females in different age groups is shown in Table 2. The sex ratio varied significantly across all age subgroups (P < 0.001, Table 2), with women being more prevalent than men. We found that during adolescence, the prevalence of HPV infection was significantly greater in females (87.50%) than in males (12.50%). During adolescence and middle age, the infection rates of females remained high at 95.66% and 98.45%, respectively, whereas those of males were relatively low. In pre- and old-age, the infection rate in females decreased slightly but remained higher than that in males. The data revealed that women had higher HPV infection rates than men across all age subgroups, emphasizing the importance of HPV prevention and screening for women. This study also highlights the need for HPV prophylaxis in men of different ages, and the results support the public health strategy of HPV vaccination for all age groups.
Table 2 Comparison of sex ratios for HPV infection in different age subgroups(N,%)Association between high- and low-risk HPV types and high-grade squamous intraepithelial lesions of the cervix or cervical cancer
According to the unadjusted model, most high-risk HPV types (e.g., HPV16, HPV18, HPV33, and HPV58) were significantly positively associated with high grade cervical squamous intraepithelial lesion (HSIL) or cervical cancer. For example, the ratio for HPV16 positivity was 8.38, indicating a significantly increased risk of HSIL or cervical cancer associated with HPV16 positivity. After adjusting for age (adjusted I) and further adjusting for combined HPV16 and/or HPV18 infection and age (adjusted II), the strength of the association changed for most HPV types but remained statistically significant, suggesting that the associations of these HPV types with high-grade cervical lesions are independent and may not be affected by confounding by age and other HPV types (Table 3).
Table 3 Association between high-risk HPV types and high-grade squamous intraepithelial lesions of the cervix or cervical cancer
Moreover, we focused on the associations of low-risk HPV types with HSIL or cervical cancer. Compared with high-risk HPV types, low-risk HPV types (e.g., HPV6 and HPV11) are usually associated with a lower severity of cervical lesions. According to the unadjusted model, the ratios of some low-risk HPV types did not significantly correlate with HSIL or cervical cancer. However, HPV38 was highly prevalent among low-risk HPV types and remained significantly associated with cervical cancer after multiple adjustments, which may indicate that the potential role of HPV38 in the development of cervical lesions needs to be further investigated (Table 4).
Table 4 Association between low-risk HPV types and high-grade squamous intraepithelial lesions of the cervix or cervical cancer
These data emphasize the importance of high-risk HPV types in high-grade malignancies of the cervix and suggest that the detection of high-risk HPV types is critical in cervical cancer screening and prevention strategies. Moreover, more attention and research may be needed for certain low-risk HPV types, such as HPV38, to better understand their role in cervical cancer development. These findings have important implications for guiding clinical practice, vaccination strategies, and public health policies.
Association between HPV infection and age in women
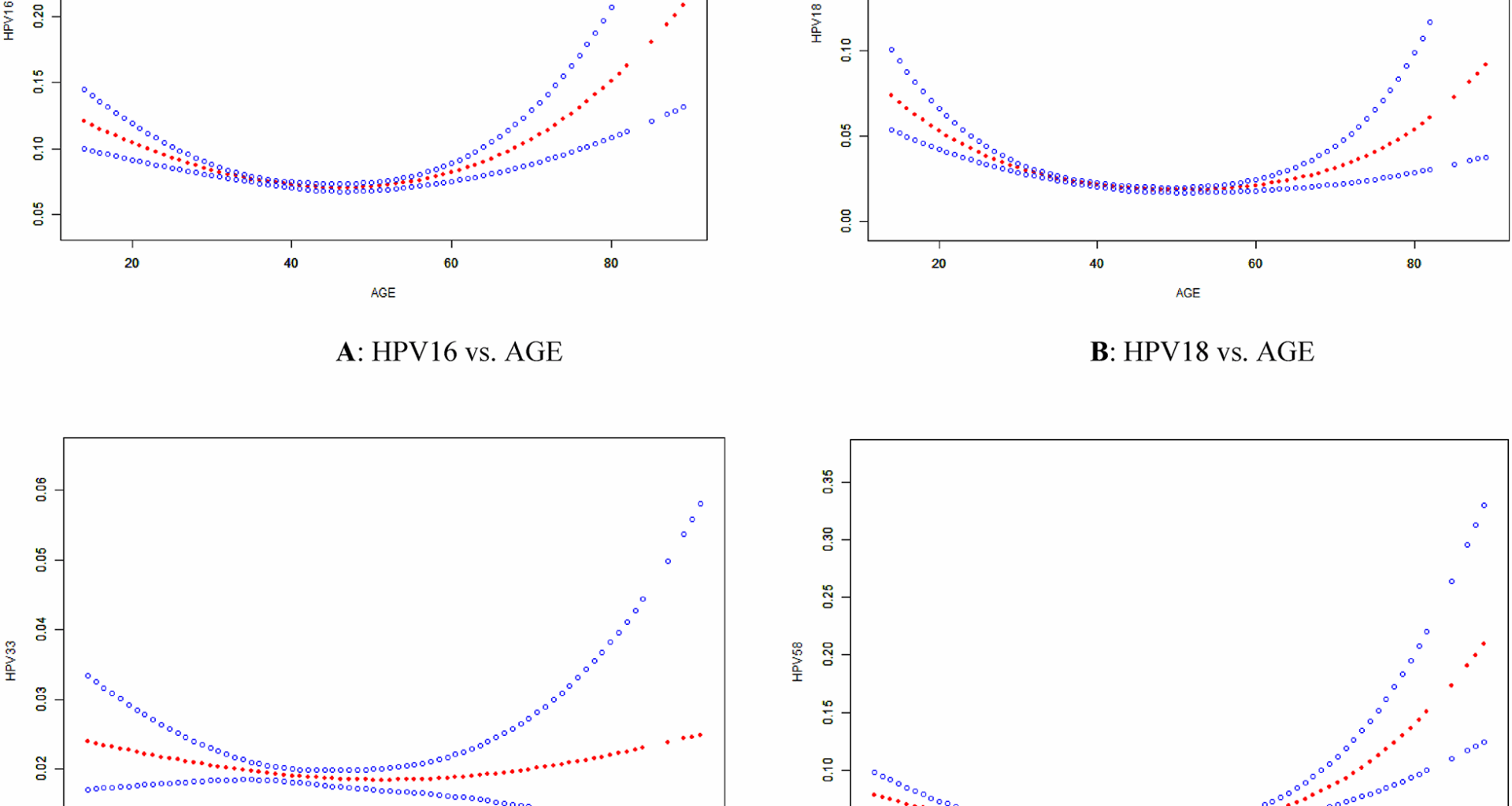
Model I and Model II show the correlations between age and HPV infection for the exposure variable age and the outcome variables HPV16, HPV18, HPV33, and HPV58 (different types of HPV) (Fig. 1).
A:Threshold nonlinear association between HPV16 and age observed in a generalized additive model (GAM). The red dashed line represents a smooth curve fit between the variables. The blue band represents the 95% confidence interval of the fit; 26 is its inflection point (K). B: A similar curve was found between HPV18 and age, where 42 was identified as the inflection point (K). C:A similar curve was found between HPV33 and age, where 30 was identified as the inflection point (K). D: A similar curve was found between HPV58 and age, where 37 was identified as the inflection point (K)
Model I represents the association between age and infection with different HPV types as a linear impact. Nevertheless, all p values exceeded 0.05, indicating the absence of a noteworthy linear correlation between age and HPV infection (Table 5).
Table 5 Association between HPV infection and age analyzed by threshold effect
Model II incorporates a fold point K to establish a threshold for age and divided the correlation between age and HPV infection into two stages, namely, 26, 42, 30, and 37 years, for the fold points (K) for HPV16, HPV18, HPV33, and HPV58, respectively. For all types of HPV, increasing age significantly correlated with a reduction in HPV infections among individuals younger than K years old (all p values were less than 0.0001). Nevertheless, once the age exceeded this limit, older age was strongly linked to an increase in HPV infections (all P values were less than 0.05) (Fig. 1).
The age threshold effect was statistically significant for all HPV types, as indicated by the p value for the difference between the effects of 2 and 1 (all p values < 0.0001). The impact of age on HPV16, HPV18, HPV33, and HPV58 infections varied significantly before and after the threshold was reached (Table 5).
In conclusion, all the p values from the log-likelihood ratio tests were less than 0.001, suggesting that Model II provided a superior fit than Model I. Table 5 below provides a summary of the findings from this study. Specifically, the table shows that the model that accounted for the age limit provided a more precise depiction of the impact of age on HPV16, HPV18, HPV33, and HPV58 infection.
To summarize, the findings from the analysis of Model II indicated that prior to the fold point, the impact of age on HPV16, HPV18, HPV33, and HPV58 infection first weakened and then became statistically significant, suggesting that the likelihood of having HPV may decrease with increasing age. Following the fold points, the impact of age on HPV16, HPV18, HPV33, and HPV58 infection intensified and became statistically significant, potentially leading to a greater likelihood of acquiring HPV as age increased. The existence of these fold points indicated a nonlinear correlation between age and HPV16, HPV18, HPV33, and HPV58 infection (Table 5).