Meis, J. F. & Chowdhary, A. Candida auris: a global fungal public health threat. Lancet Infect. Dis. 18, 1298–1299 (2018).
WHO. World Health Organization (WHO) fungal priority pathogens list to guide research, development and public health action. https://www.who.int/publications/i/item/9789240060241 (2022).
Lee, W. G. et al. First three reported cases of nosocomial fungemia caused by Candida auris. J. Clin. Microbiol. 49, 4 (2011).
Satoh, K. et al. Candida auris sp. Nov., a novel ascomycetous yeast isolated from the external ear canal of an inpatient in a Japanese hospital. Microbiol. Immunol. 53, 41–44 (2009).
Eyre, D. W. et al. A Candida auris outbreak and its control in an intensive care setting. N. Engl. J. Med. 379, 1322–1331 (2018).
Taori, S. K. et al. Candida auris outbreak: mortality, interventions and cost of sustaining control. J. Infect. 79, 601–611 (2019).
Shuping, L. et al. High prevalence of Candida auris colonization during protracted neonatal unit outbreak, South Africa. Emerg. Infect. Dis. https://doi.org/10.3201/eid2909.230393 (2023).
Adam, R. D. et al. Analysis of Candida auris fungemia at a single facility in Kenya. Int. J. Infect. Dis. 85, 182–187 (2019).
Prayag, P. S., Patwardhan, S., Panchakshari, S., Rajhans, P. A. & Prayag, A. The dominance of Candida auris: a single-center experience of 79 episodes of candidemia from western India. Indian J. Crit. Care Med. 26, 560–563 (2022).
Chen, J. et al. Is the superbug fungus really so scary? A systematic review and meta-analysis of global epidemiology and mortality of Candida auris. BMC Infect. Dis. 20, 827 (2020).
Lyman, M. Notes from the field: transmission of pan-resistant and echinocandin-resistant Candida auris in health care facilities—Texas and the District of Columbia, January-April 2021. Morb. Mortal. Wkly. Rep. 70, 1022–1023 (2021).
Khan, T. et al. Emergence of the novel sixth Candida auris clade VI in Bangladesh. Microbiol. Spectr. 12, e03540–23 (2024).
Suphavilai, C. et al. Detection and characterisation of a sixth Candida auris clade in Singapore: a genomic and phenotypic study. Lancet Microbe 5, 100878 (2024).
Lockhart, S. R. et al. Simultaneous emergence of multidrug-resistant Candida auris on 3 continents confirmed by whole-genome sequencing and epidemiological analyses. Clin. Infect. Dis. 64, 134–140 (2017).
Gifford, H., Rhodes, J. & Farrer, R. A. The diverse genomes of Candida auris. Lancet Microbe 5, 100903 (2024).
Byun, S. A. et al. Virulence traits and azole resistance in Korean Candida auris Isolates. J. Fungi 9, 979 (2023).
Santana, D. J., Zhao, G. & O’Meara, T. R. The many faces of Candida auris: phenotypic and strain variation in an emerging pathogen. PLoS Pathog. 20, e1012011 (2024).
Wang, T. W. et al. Functional redundancy in Candida auris cell surface adhesins crucial for cell-cell interaction and aggregation. Nat. Commun. 15, 9212 (2024).
Allert, S. et al. From environmental adaptation to host survival: attributes that mediate pathogenicity of Candida auris. Virulence 13, 191–214 (2022).
Fayed, B. et al. Transcriptome analysis of human dermal cells infected with Candida auris identified unique pathogenesis/defensive mechanisms particularly ferroptosis. Mycopathologia 189, 65 (2024).
Yang, B. et al. A correlative study of the genomic underpinning of virulence traits and drug tolerance of Candida auris. Infect. Immun. 0, e00103–e00124 (2024).
Balakumar, A. et al. Single-cell transcriptomics unveils skin cell specific antifungal immune responses and IL-1Ra- IL-1R immune evasion strategies of emerging fungal pathogen Candida auris. PLoS Pathog. 20, e1012699 (2024).
Bruno, M. et al. Transcriptional and functional insights into the host immune response against the emerging fungal pathogen Candida auris. Nat. Microbiol. 5, 1516–1531 (2020).
Wang, Y. et al. Innate immune responses against the fungal pathogen Candida auris. Nat. Commun. 13, 3553 (2022).
Yue, H. et al. Filamentation in Candida auris, an emerging fungal pathogen of humans: passage through the mammalian body induces a heritable phenotypic switch. Emerg. Microbes Infect. 7, 1–13 (2018).
Chadwick, C., Jesus, M. D., Ginty, F. & Martinez, J. S. Pathobiology of Candida auris infection analyzed by multiplexed imaging and single cell analysis. PLoS ONE 19, e0293011 (2024).
Santana, D. J. et al. A Candida auris-specific adhesin, Scf1, governs surface association, colonization, and virulence. Science 381, 1461–1467 (2023).
Pelletier, C., Shaw, S., Alsayegh, S., Brown, A. J. P. & Lorenz, A. Candida auris undergoes adhesin-dependent and -independent cellular aggregation. PLoS Pathog. 20, e1012076 (2024).
Muñoz, J. F. et al. Genomic insights into multidrug-resistance, mating and virulence in Candida auris and related emerging species. Nat. Commun. 9, 5346 (2018).
Richardson, J. P. et al. Candidalysins are a new family of cytolytic fungal peptide toxins. mBio 13, e03510–e03521 (2022).
Kim, J.-S., Lee, K.-T. & Bahn, Y.-S. Secreted aspartyl protease 3 regulated by the Ras/cAMP/PKA pathway promotes the virulence of Candida auris. Front. Cell. Infect. Microbiol. 13, 1257897 (2023).
Horton, M. V. et al. Candida auris cell wall mannosylation contributes to neutrophil evasion through pathways divergent from Candida albicans and Candida glabrata. mSphere 6, e00406–e00421 (2021).
Weerasinghe, H. et al. Candida auris uses metabolic strategies to escape and kill macrophages while avoiding robust activation of the NLRP3 inflammasome response. Cell Rep. 42, 112522 (2023).
Wang, X. et al. The first isolate of Candida auris in China: clinical and biological aspects. Emerg. Microbes Infect. 7, 1–9 (2018).
Fan, S., Li, C., Bing, J., Huang, G. & Du, H. Discovery of the diploid form of the emerging fungal pathogen Candida auris. ACS Infect. Dis. 6, 2641–2646 (2020).
Fan, S. et al. A biological and genomic comparison of a drug-resistant and a drug-susceptible strain of Candida auris isolated from Beijing, China. Virulence 12, 1388–1399 (2021).
Wurster, S., Albert, N. D. & Kontoyiannis, D. P. Candida auris bloodstream infection induces upregulation of the PD-1/PD-L1 immune checkpoint pathway in an immunocompetent mouse model. mSphere 7, e00817–e00821 (2022).
Bing, J. et al. Rapid evolution of an adaptive multicellular morphology of Candida auris during systemic infection. Nat. Commun. 15, 2381 (2024).
Ben-Ami, R. et al. Multidrug-resistant Candida haemulonii and C. auris, Tel Aviv, Israel. Emerg. Infect. Dis. 23, 195–203 (2017).
Hager, C. L., Larkin, E. L., Long, L. A. & Ghannoum, M. A. Evaluation of the efficacy of rezafungin, a novel echinocandin, in the treatment of disseminated Candida auris infection using an immunocompromised mouse model. J. Antimicrobial. Chemother. 73, 2085–2088 (2018).
Zhao, M. et al. In vivo pharmacokinetics and pharmacodynamics of APX001 against Candida spp. In a neutropenic disseminated candidiasis mouse model. Antimicrobial. Agents Chemother. 62, e02542–17 (2018).
Singh, S. et al. The NDV-3A vaccine protects mice from multidrug resistant Candida auris infection. PLoS Pathog. 15, e1007460 (2019).
Zhang, F. et al. A marine microbiome antifungal targets urgent-threat drug-resistant fungi. Science 370, 974–978 (2020).
Muñoz, J. E. et al. Pathogenicity levels of Colombian strains of Candida auris and Brazilian strains of Candida haemulonii species complex in both murine and Galleria mellonella experimental models. J. Fungi 6, 104 (2020).
Abe, M. et al. Potency of gastrointestinal colonization and virulence of Candida auris in a murine endogenous candidiasis. PLoS ONE 15, e0243223 (2020).
Forgács, L. et al. Comparison of in vivo pathogenicity of four Candida auris clades in a neutropenic bloodstream infection murine model. Emerg. Microbes Infect. 9, 1160–1169 (2020).
Nagy, F. et al. In vitro and in vivo interaction of caspofungin with isavuconazole against Candida auris planktonic cells and biofilms. Med. Mycol. 59, 1015–1023 (2021).
Forgács, L. et al. In vivo efficacy of amphotericin B against four Candida auris clades. J. Fungi 8, 499 (2022).
Singh, S. et al. Protective efficacy of anti-Hyr1p monoclonal antibody against systemic candidiasis due to multi-drug-resistant Candida auris. J. Fungi 9, 103 (2023).
Salama, E. A. et al. Lansoprazole interferes with fungal respiration and acts synergistically with amphotericin B against multidrug-resistant Candida auris. Emerg. Microbes Infect. 13, 2322649 (2024).
Torres, S. R. et al. Impact of Candida auris infection in a neutropenic murine model. Antimicrobial. Agents Chemother. 64, e01625–19 (2020).
Xin, H., Mohiuddin, F., Tran, J., Adams, A. & Eberle, K. Experimental mouse models of disseminated Candida auris infection. mSphere 4, e00339–19 (2019).
Rosario-Colon, J., Eberle, K., Adams, A., Courville, E. & Xin, H. Candida cell-surface-specific monoclonal antibodies protect mice against Candida auris invasive infection. Int. J. Mol. Sci. 22, 6162 (2021).
Torres, S. R. et al. Assessment of environmental and occupational exposure while working with multidrug resistant (MDR) fungus Candida auris in an animal facility. J. Occup. Environ. Hyg. 16, 507–518 (2019).
Borman, A. M. Of mice and men and larvae: Galleria mellonella to model the early host-pathogen interactions after fungal infection. Virulence 9, 9–12 (2017).
Romera, D. et al. The Galleria mellonella infection model as a system to investigate the virulence of Candida auris strains. Pathog. Dis. 78, ftaa067 (2020).
García-Carnero, L. C. et al. Early virulence predictors during the Candida species–Galleria mellonella interaction. J. Fungi 6, 152 (2020).
Garcia-Bustos, V. et al. Characterization of the differential pathogenicity of Candida auris in a Galleria mellonella infection model. Microbiol. Spectr. 9, e00013–e00021 (2021).
Carvajal, S. K. et al. Pathogenicity assessment of Colombian strains of Candida auris in the Galleria mellonella invertebrate model. J. Fungi 7, 401 (2021).
Hernando-Ortiz, A. et al. Virulence of Candida auris from different clinical origins in Caenorhabditis elegans and Galleria mellonella host models. Virulence 12, 1063–1075 (2021).
Spettel, K. et al. Candida auris in Austria—what is new and what is different. J. Fungi 9, 129 (2023).
Wurster, S. et al. Drosophila melanogaster as a model to study virulence and azole treatment of the emerging pathogen Candida auris. J. Antimicrobial. Chemother. 74, 1904–1910 (2019).
Harpf, V., Rambach, G., Würzner, R., Lass-Flörl, C. & Speth, C. Candida and complement: new aspects in an old battle. Front. Immunol. 11, 1471 (2020).
Pechacek, J. & Lionakis, M. S. Host defense mechanisms against Candida auris. Expert Rev. Anti Infec. Ther. 21, 1087–1096 (2023).
Johnson, C. J., Davis, J. M., Huttenlocher, A., Kernien, J. F. & Nett, J. E. Emerging fungal pathogen Candida auris evades neutrophil attack. mBio 9, e01403–e01418 (2018).
Pharkjaksu, S., Boonmee, N., Mitrpant, C. & Ngamskulrungroj, P. Immunopathogenesis of emerging Candida auris and Candida haemulonii strains. J. Fungi 7, 725 (2021).
Shapiro, R. S. & Cowen, L. E. Uncovering cellular circuitry controlling temperature-dependent fungal morphogenesis. Virulence 3, 400–404 (2012).
Leach, M. D. et al. Hsf1 and Hsp90 orchestrate temperature-dependent global transcriptional remodelling and chromatin architecture in Candida albicans. Nat. Commun. 7, 11704 (2016).
Xiao, W. et al. Response and regulatory mechanisms of heat resistance in pathogenic fungi. Appl. Microbiol. Biotechnol. 106, 5415–5431 (2022).
Arora, P. et al. Environmental isolation of Candida auris from the coastal wetlands of Andaman Islands, India. mBio 12, e03181–20 (2021).
Escandón, P. Novel environmental niches for Candida auris: isolation from a coastal habitat in Colombia. J. Fungi 8, 748 (2022).
Uden, V. & Kolipinski, M. C. Torulopsis haemulonii nov. spec., a yeast from the Atlantic Ocean. Antonie Van. Leeuwenhoek 28, 78–80 (1962).
Bavia, L., Santiesteban-Lores, L. E., Carneiro, M. C. & Prodocimo, M. M. Advances in the complement system of a teleost fish, Oreochromis niloticus. Fish. Shellfish Immunol. 123, 61–74 (2022).
Buchmann, K., Karami, A. M. & Duan, Y. The early ontogenetic development of immune cells and organs in teleosts. Fish. Shellfish Immunol. 146, 109371 (2024).
Tian, H. et al. Cytokine networks provide sufficient evidence for the differentiation of CD4+ T cells in teleost fish. Dev. Comp. Immunol. 141, 104627 (2023).
Akbarzadeh, A. & Leder, E. H. Acclimation of killifish to thermal extremes of hot spring: transcription of gonadal and liver heat shock genes. Comp. Biochem. Physiol. Part A Mol. Integr. Physiol. 191, 89–97 (2016).
Hamied, A. et al. Identification and characterization of highly fluorescent pigment cells in embryos of the Arabian killifish (Aphanius Dispar). iScience 23, 101674 (2020).
Alsakran, A. et al. Stage-by-stage exploration of normal embryonic development in the Arabian killifish. Aphanius dispar. Dev. Dyn. 254, 380–395 (2024).
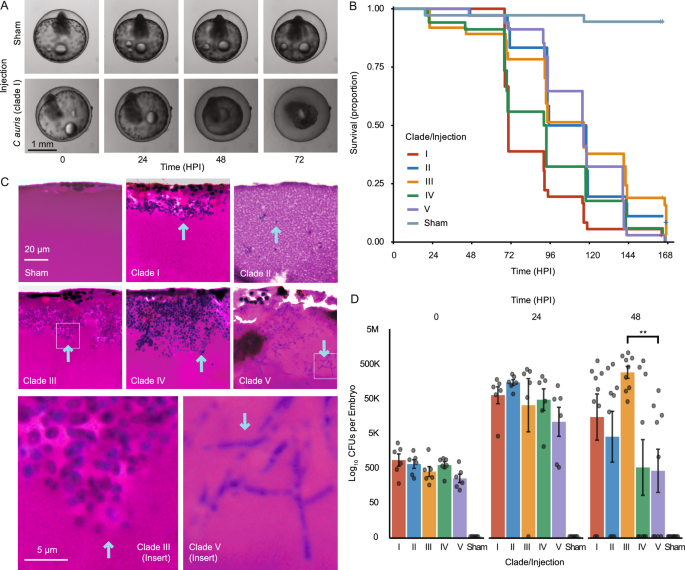
Minhas, R. et al. The thermotolerant Arabian killifish, Aphanius dispar, as a novel infection model for human fungal pathogens. https://doi.org/10.1101/2024.10.08.617174 (2024).
Gifford, H., Wilson, D., Rhodes, J. & Farrer, R. A. Seaside to bedside: assembly in research for emerging human fungal pathogen Candida auris. In Genome Assembly (ed. Farrer, R. A.) vol. 2955 263–291 (Springer US, 2025).
Burden, N., Chapman, K., Sewell, F. & Robinson, V. Pioneering better science through the 3Rs: an introduction to the national centre for the replacement, refinement, and reduction of animals in research (NC3Rs). J. Am. Assoc. Lab. Anim. Sci. 54, 198–208 (2015).
Skrzypek, M. S. et al. The Candida Genome Database (CGD): incorporation of assembly 22, systematic identifiers and visualization of high throughput sequencing data. Nucleic Acids Res. 45, D592–D596 (2017).
Potrykus, J. et al. Fungal iron availability during deep seated candidiasis is defined by a complex interplay involving systemic and local events. PLoS Pathog. 9, e1003676 (2013).
Kasper, L. et al. The fungal peptide toxin candidalysin activates the NLRP3 inflammasome and causes cytolysis in mononuclear phagocytes. Nat. Commun. 9, 4260 (2018).
Bonzi, L. C. et al. The time course of molecular acclimation to seawater in a euryhaline fish. Sci. Rep. 11, 18127 (2021).
Varma, A. et al. Molecular cloning and functional characterisation of a glucose transporter, CaHGT1, of Candida albicans. FEMS Microbiol. Lett. 182, 15–21 (2000).
Luo, L., Tong, X. & Farley, P. C. The Candida albicans gene HGT12 (Orf19.7094) encodes a hexose transporter. FEMS Immunol. Med. Microbiol. 51, 14–17 (2007).
Brown, V., Sexton, J. A. & Johnston, M. A glucose sensor in Candida albicans. Eukaryot. Cell 5, 1726–1737 (2006).
Larcombe, D. E. et al. Glucose-enhanced oxidative stress resistance-A protective anticipatory response that enhances the fitness of Candida albicans during systemic infection. PLoS Pathog. 19, e1011505 (2023).
Martin, R. et al. A core filamentation response network in Candida albicans is restricted to eight genes. PLoS ONE 8, e58613 (2013).
Schatzman, S. S. et al. Copper-only superoxide dismutase enzymes and iron starvation stress in Candida fungal pathogens. J. Biol. Chem. 295, 570–583 (2020).
Rybak, J. M. et al. Abrogation of triazole resistance upon deletion of CDR1 in a clinical isolate of Candida auris. Antimicrob. Agents and Chemother. 63, e00057–19 (2019).
Li, J., Coste, A. T., Bachmann, D., Sanglard, D. & Lamoth, F. Deciphering the Mrr1/Mdr1 pathway in azole resistance of Candida auris. Antimicrobial. Agents Chemother. 66, e00067–22 (2022).
Sun, S., Coelho, M. A., David-Palma, M., Priest, S. J. & Heitman, J. The evolution of sexual reproduction and the mating-type locus: links to pathogenesis of Cryptococcus human pathogenic fungi. Annu. Rev. Genet. 53, 417–444 (2019).
Wang, Y. & Xu, J. Population genomic analyses reveal evidence for limited recombination in the superbug Candida auris in nature. Comput. Struct. Biotechnol. J. 20, 3030–3040 (2022).
Chow, N. A. et al. Potential fifth clade of Candida auris, Iran, 2018. Emerg. Infect. Dis. 25, 1780–1781 (2019).
Louvet, M. et al. Ume6-dependent pathways of morphogenesis and biofilm formation in Candida auris. Microbiol. Spectr. 0, e01531–24 (2024).
Deng, Y., Li, S., Bing, J., Liao, W. & Tao, L. Phenotypic switching and filamentation in Candida haemulonii, an emerging opportunistic pathogen of humans. Microbiol. Spectr. 9, e00779–21 (2021).
Overy, D. P., Rämä, T., Oosterhuis, R., Walker, A. K. & Pang, K.-L. The neglected marine fungi, Sensu stricto, and their isolation for natural products’ discovery. Mar. Drugs 17, 42 (2019).
Seiser, S. et al. Native human and mouse skin infection models to study Candida auris-host interactions. Microbes Infect. 26, 105234 (2024).
Fan, S. et al. Filamentous growth is a general feature of Candida auris clinical isolates. Med. Mycol. 59, 734–740 (2021).
Bravo Ruiz, G., Ross, Z. K., Gow, N. A. R. & Lorenz, A. Pseudohyphal growth of the emerging pathogen Candida auris is triggered by genotoxic stress through the S phase checkpoint. mSphere 5, e00151–20 (2020).
Kim, S. H. et al. Genetic analysis of Candida auris implicates Hsp90 in morphogenesis and azole tolerance and Cdr1 in Azole Resistance. mBio 10, e02529–18 (2019).
Gao, J. et al. LncRNA DINOR is a virulence factor and global regulator of stress responses in Candida auris. Nat. Microbiol. 6, 842–851 (2021).
Chybowska, A. D., Childers, D. S. & Farrer, R. A. Nine things genomics can tell us about Candida auris. Front. Genet. 11, 351 (2020).
Ismail, A., Bedell, G. W. & Lupan, D. M. Siderophore production by the pathogenic yeast, Candida albicans. Biochem. Biophys. Res. Commun. 130, 885–891 (1985).
Heymann, P. et al. The Siderophore iron transporter of Candida albicans (Sit1p/Arn1p) mediates uptake of ferrichrome-type siderophores and Is required for epithelial invasion. Infect. Immun. 70, 5246–5255 (2002).
Boiteau, R. M. et al. Siderophore-based microbial adaptations to iron scarcity across the eastern Pacific Ocean. Proc. Natl. Acad. Sci. USA 113, 14237–14242 (2016).
Park, J. et al. Siderophore production and utilization by marine bacteria in the North Pacific Ocean. Limnol. Oceanogr. 68, 1636–1653 (2023).
Renshaw, J. C. et al. Fungal siderophores: structures, functions and applications. Mycol. Res. 106, 1123–1142 (2002).
Johnstone, T. C. & Nolan, E. M. Beyond iron: non-classical biological functions of bacterial siderophores. Dalton Trans. 44, 6320–6339 (2015).
Nakajima, Y. et al. Effect of disrupting the trichothecene efflux pump encoded by FgTri12 in the nivalenol chemotype of Fusarium graminearum. J. Gen. Appl. Microbiol. 61, 93–96 (2015).
Xue, P. et al. Heme sensing and trafficking in fungi. Fungal Biol. Rev. 43, 100286 (2023).
Fourie, R., Kuloyo, O. O., Mochochoko, B. M., Albertyn, J. & Pohl, C. H. Iron at the Centre of Candida albicans Interactions. Front. Cell. Infect. Microbiol. 8, 185 (2018).
Alselami, A. & Drummond, R. A. How metals fuel fungal virulence, yet promote anti-fungal immunity. Dis. Models Mech. 16, dmm050393 (2023).
Pradhan, A. et al. Non-canonical signalling mediates changes in fungal cell wall PAMPs that drive immune evasion. Nat. Commun. 10, 5315 (2019).
Weissman, Z. & Kornitzer, D. A family of Candida cell surface haem-binding proteins involved in haemin and haemoglobin-iron utilization. Mol. Microbiol. 53, 1209–1220 (2004).
Ding, C. et al. Conserved and divergent roles of Bcr1 and CFEM proteins in Candida parapsilosis and Candida albicans. PLoS ONE 6, e28151 (2011).
Sharma, P. & Pasrija, R. Iron chelators enhance the potency of Echinocandins against Candida auris. https://doi.org/10.21203/rs.3.rs-7042978/v1 (2025).
Simm, C. et al. Disruption of iron homeostasis and mitochondrial metabolism are promising targets to inhibit Candida auris. Microbiol. Spectr. 10, e00100–e00122 (2022).
Zhang, J. et al. Pyrvinium pamoate synergizes with azoles in vitro and in vivo to exert antifungal efficacy against Candida auris and other Candida species. Infect. Drug Resist. 18, 783–789 (2025).
Hoyer, L. L., Green, C. B., Oh, S.-H. & Zhao, X. Discovering the secrets of the Candida albicans agglutinin-like sequence (ALS) gene family—a sticky pursuit. Med. Mycol. 46, 1–15 (2008).
Smoak, R. A., Snyder, L. F., Fassler, J. S. & He, B. Z. Parallel expansion and divergence of an adhesin family in pathogenic yeasts. Genetics 223, iyad024 (2023).
Sert, N. P. du et al. Reporting animal research: explanation and elaboration for the ARRIVE guidelines 2.0. PLoS Biol. 18, e3000411 (2020).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. R. Stat. Soc. Ser. B Stat. Methodol. 57, 289–300 (1995).
Suvarna, S. K., Layton, C. & Bancroft, J. D. In Bancroft’s Theory and Practice of Histological Techniques (Churchill Livingstone Elsevier, 2013).
Chen, S., Zhou, Y., Chen, Y. & Gu, J. Fastp: an ultra-fast all-in-one FASTQ preprocessor. Bioinformatics 34, i884–i890 (2018).
Ewels, P., Magnusson, M., Lundin, S. & Käller, M. MultiQC: summarize analysis results for multiple tools and samples in a single report. Bioinformatics 32, 3047–3048 (2016).
Haas, B. J. et al. De novo transcript sequence reconstruction from RNA-seq using the Trinity platform for reference generation and analysis. Nat. Protoc. 8, 1494–1512 (2013).
Abastabar, M. et al. Candida auris otomycosis in Iran and review of recent literature. Mycoses 62, 101–105 (2019).
Muñoz, J. F. et al. Clade-specific chromosomal rearrangements and loss of subtelomeric adhesins in Candida auris. Genetics 218, iyab029 (2021).
Langmead, B. & Salzberg, S. L. Fast gapped-read alignment with Bowtie 2. Nat. Methods 9, 357–359 (2012).
Li, B. & Dewey, C. N. RSEM: accurate transcript quantification from RNA-Seq data with or without a reference genome. BMC Bioinforma. 12, 323 (2011).
Robinson, M. D., McCarthy, D. J. & Smyth, G. K. edgeR: a Bioconductor package for differential expression analysis of digital gene expression data. Bioinformatics 26, 139–140 (2010).
Li, H. et al. The sequence alignment/map format and SAMtools. Bioinformatics 25, 2078–2079 (2009).
Ritchie, M. E. et al. Limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 43, e47 (2015).
Gu, Z., Eils, R. & Schlesner, M. Complex heatmaps reveal patterns and correlations in multidimensional genomic data. Bioinformatics 32, 2847–2849 (2016).
Ashburner, M. et al. Gene ontology: tool for the unification of biology. Nat. Genet. 25, 25–29 (2000).
The Gene Ontology Consortium et al. The Gene Ontology knowledgebase in 2023. Genetics 224, iyad031 (2023).
Buchfink, B., Reuter, K. & Drost, H.-G. Sensitive protein alignments at tree-of-life scale using DIAMOND. Nat. Methods 18, 366–368 (2021).
Golden, C., Studholme, D. J. & Farrer, R. A. DIAMOND2GO: a rapid Gene Ontology assignment and enrichment tool for functional genomics. https://doi.org/10.1101/2024.08.19.608700 (2024).
Kanehisa, M., Furumichi, M., Sato, Y., Kawashima, M. & Ishiguro-Watanabe, M. KEGG for taxonomy-based analysis of pathways and genomes. Nucleic Acids Res. 51, D587–D592 (2022).
Kanehisa, M., Sato, Y. & Morishima, K. BlastKOALA and GhostKOALA: KEGG tools for functional characterization of genome and metagenome sequences. J. Mol. Biol. 428, 726–731 (2016).
Bateman, A. et al. The Pfam protein families database. Nucleic Acids Res. 32, D138–D141 (2004).
Eddy, S. R. Accelerated profile HMM searches. PLoS Comput. Biol. 7, e1002195 (2011).
Almagro Armenteros, J. J. et al. SignalP 5.0 improves signal peptide predictions using deep neural networks. Nat. Biotechnol. 37, 420–423 (2019).
Hallgren, J. et al. DeepTMHMM predicts alpha and beta transmembrane proteins using deep neural networks. https://doi.org/10.1101/2022.04.08.487609 (2022).
Gíslason, M. H., Nielsen, H., Almagro Armenteros, J. J. & Johansen, A. R. Prediction of GPI-anchored proteins with pointer neural networks. Curr. Res. Biotechnol. 3, 6–13 (2021).
Camacho, C. et al. BLAST+: architecture and applications. BMC Bioinforma. 10, 421 (2009).
Supek, F., Bošnjak, M., Škunca, N. & Šmuc, T. REVIGO summarizes and visualizes long lists of gene ontology terms. PLoS ONE 6, e21800 (2011).
Farrer, R. A. Synima: a synteny imaging tool for annotated genome assemblies. BMC Bioinforma. 18, 507 (2017).
Emms, D. M. & Kelly, S. OrthoFinder: phylogenetic orthology inference for comparative genomics. Genome Biol. 20, 238 (2019).
Edgar, R. C. MUSCLE: Multiple sequence alignment with high accuracy and high throughput. Nucleic Acids Res. 32, 1792–1797 (2004).
Price, M. N., Dehal, P. S. & Arkin, A. P. FastTree 2 – approximately maximum-likelihood trees for large alignments. PLoS ONE 5, e9490 (2010).
Abramson, J. et al. Accurate structure prediction of biomolecular interactions with AlphaFold 3. Nature 630, 493–500 (2024).
Pettersen, E. F. et al. UCSF ChimeraX: structure visualization for researchers, educators, and developers. Protein Sci. 30, 70–82 (2021).
Stamatakis, A. RAxML version 8: a tool for phylogenetic analysis and post-analysis of large phylogenies. Bioinformatics 30, 1312–1313 (2014).
Sievers, F. & Higgins, D. G. Clustal Omega. Curr. Protoc. Bioinforma. 48, 3.13.1–3.13.16 (2014).
Gifford, H. et al. Hughgifford/Arabian_Killifish_C_auris_2024: Pre-publication. https://zenodo.org/records/17515669 (2025).