In this week’s health update, the Africa CDC is turning to drone-based logistics to expand access to vaccines and essential medicines, while researchers in West Africa are testing the use of artificial intelligence to improve the prediction of Lassa fever outbreaks. In Madagascar, elimination efforts against lymphatic filariasis are gaining momentum in partnership with the World Health Organization and the Carter Center, even as the WHO warns of counterfeit cancer treatments entering the market. Meanwhile, Uganda is battling a deadly measles outbreak in its northeastern region, and Sierra Leone has brought its mpox outbreak under control but continues to face stigma affecting survivors. In Senegal, researchers are also documenting record dengue cases linked to the emergence of a new viral lineage.
Africa CDC turns to drones to boost epidemic preparedness
The African Union’s health agency, Africa CDC, is turning to drones to strengthen epidemic preparedness across the continent. The pan-African body signed an agreement last week with logistics company Zipline to cooperate in this area.
?️ Breaking: @AfricaCDC and @Zipline International have signed a Memorandum of Understanding to strengthen last-mile health delivery across Africa.
The partnership will help countries expand access to essential health products, improve emergency preparedness, and enhance data… pic.twitter.com/CvcunawN7n
— Africa CDC (@AfricaCDC) December 12, 2025
The partnership focuses on last-mile delivery of vaccines, diagnostics and essential medicines, particularly in remote or high-risk areas. It falls under the Africa CDC Strategic Plan 2023-2027 and supports the African Agenda for Health Security and Sovereignty. The agreement allows African Union member states, on a voluntary basis, to integrate aerial delivery solutions into their national health systems.
Beyond logistics, the initiative also aims to strengthen health data systems, epidemiological surveillance and early-warning capabilities. Zipline will contribute its operational expertise, autonomous aircraft networks and supply-chain management systems. Already operating in Rwanda, Ghana, Nigeria and Côte d’Ivoire, the model has improved delivery times and supported earlier outbreak detection. Africa CDC now wants to scale it up as a continent-wide tool for health resilience.
West Africa deploys artificial intelligence against Lassa fever
In West Africa, researchers are stepping up the use of artificial intelligence to improve early detection and forecasting of Lassa fever outbreaks. Machine-learning tools analyse large datasets, including environmental factors, population density and past epidemics, to identify high-risk areas.
According to GeneOnline, these predictive models help anticipate transmission patterns and guide public-health interventions more effectively. The aim is to optimise resource allocation during health crises and shorten response times.
Researchers are also exploring AI applications to improve diagnostic accuracy and speed up work on vaccines and treatments. Integrating these tools into existing health systems is expected to strengthen preparedness for haemorrhagic fevers and emerging epidemics. In a region regularly affected by Lassa fever, such approaches help offset weak conventional surveillance and highlight the growing role of data science in regional health security.
WHO warns of fake breast cancer drugs in Africa and the Middle East
The World Health Organization has issued a global alert after detecting falsified versions of the anticancer drug IBRANCE in five countries, including Côte d’Ivoire, Egypt and Libya. The counterfeit products, sold online and in some pharmacies, contain no active ingredient and pose serious risks to patients.
Laboratory analyses confirmed the absence of palbociclib, used to treat certain advanced breast cancers. While the packaging closely resembles the genuine product, subtle anomalies such as labelling errors or unusual markings can help identify the fakes.
The WHO warned that use of the counterfeit drugs can lead to treatment failure, uncontrolled disease progression and a higher risk of death. It called on national authorities to strengthen supply-chain surveillance, particularly in informal and online markets. Patients were urged to buy medicines only from authorised sources and to report any suspected adverse effects.
African states renew commitment to fight diphtheria
Health ministers from several African countries have renewed their political commitment to halt the resurgence of diphtheria, a vaccine-preventable disease now reported in at least eight countries. More than 90% of recorded cases involve unvaccinated or under-immunised children.

At a meeting convened by WHO Africa on December 17, 2025, representatives from affected countries, including Chad, Nigeria and Niger, called for stronger routine immunisation systems and catch-up vaccination campaigns. Partners such as UNICEF, Gavi and Africa CDC reaffirmed their support.
The WHO said funding gaps, weak laboratory capacity and limited access to diphtheria antitoxin continue to slow progress. It also warned that disruptions linked to the Covid-19 pandemic have widened immunity gaps, particularly in conflict-affected areas. Experts stress the need to strengthen surveillance, community engagement and local vaccine production to prevent further outbreaks.
New viral lineage behind Senegal’s largest dengue outbreak
Senegal recorded its largest dengue outbreak in 2025, with 3,633 confirmed cases and two deaths. Genomic analyses by the Institut Pasteur in Dakar show the co-circulation of DENV-1 and DENV-2 serotypes, with DENV-2 accounting for nearly 98% of typed samples.
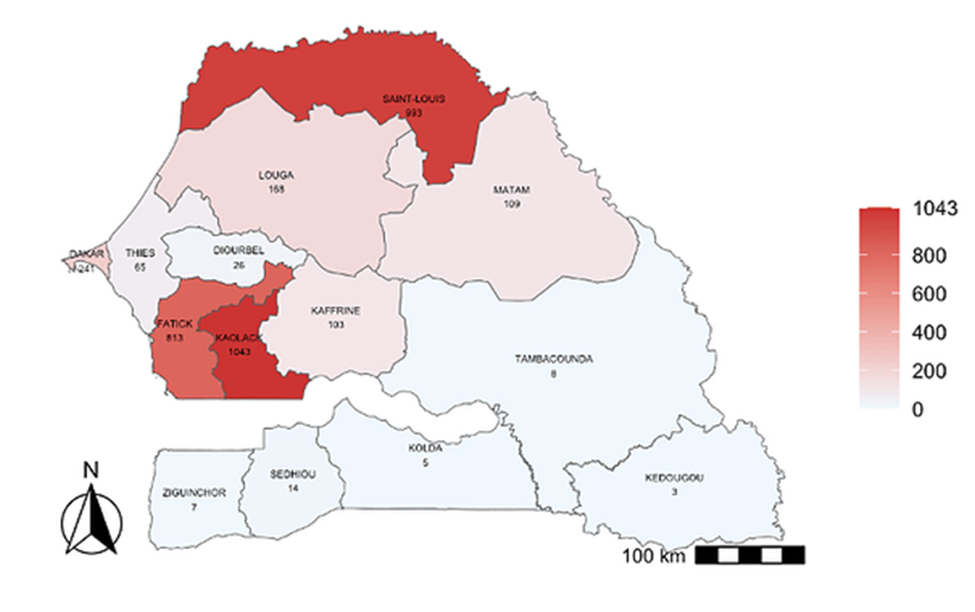
Researchers identified the introduction of a new DENV-2 lineage closely related to strains detected in India and Réunion Island in 2023 and 2024. This lineage is linked to the most severe cases observed during the outbreak.
The continued presence of DENV-1, detected in previous years, points to endemic circulation in the region. No mutations associated with resistance to the antiviral mosnodenvir were found, suggesting the drug remains effective. Researchers called for stronger genomic and syndromic surveillance to track viral evolution and adapt vaccine and treatment strategies in West Africa.
Côte d’Ivoire to host first African Health Fair in 2026
Côte d’Ivoire will host the first African Health Fair from April 15 to 17, 2026, in Abidjan, authorities said this week. The announcement was made by Yéo Pena Abdoulaye, director of health infrastructure, during a press briefing.
The event aims to become a regional platform for dialogue and solutions, bringing together policymakers, health professionals, investors, companies and civil-society organisations. Organisers hope it will help position Côte d’Ivoire as a hub for medical solutions tailored to African needs.
Congo approves national plan to strengthen health workforce
The Republic of Congo has approved its National Health Human Resources Development Plan for 2026-2030. The strategy focuses on four main areas, including improved initial and in-service training, modernised career management and the gradual introduction of digital tools, alongside stronger governance.
The plan aims to improve the quality of care, strengthen resilience to health emergencies and restore public confidence in the health system. The WHO welcomed the plan, noting its alignment with regional and global commitments and stressing that health workers are a cornerstone of any effective health system.
Congolese authorities called for increased funding and stronger coordination across sectors to ensure the plan is fully implemented.
WHO and Carter Center step up fight against neglected tropical diseases in Madagascar
The World Health Organization and the Carter Center have signed an agreement to accelerate efforts to eliminate lymphatic filariasis in Madagascar. Backed by the Reaching the Last Mile Fund, the partnership will support the Ministry of Public Health in 87 districts still affected by the mosquito-borne disease.
The project aims to eliminate lymphatic filariasis as a public-health problem by 2030. It includes mass drug administration campaigns, stronger epidemiological surveillance and improved care for patients with lymphedema or hydrocele.
Beyond disease control, the partners also aim to strengthen local logistics and technical capacity to expand prevention efforts and improve access to care in vulnerable areas.
Measles outbreak kills 32 in northeastern Uganda
A measles outbreak in northeastern Uganda has killed 32 people across four districts, according to an updated report from the Ministry of Health. Most of the deaths were children. Seventeen deaths were recorded in Napak district, seven in Nakapiripirit, and four each in Abim and Moroto.
A total of 505 cases have been confirmed since the outbreak was declared one month ago. Authorities have deployed emergency teams to step up investigations, active surveillance and rapid response.
The ministry cited low vaccination coverage, delayed case detection, weaknesses in routine immunisation and late access to care as key factors worsening the outbreak. A vaccination campaign targeting children aged six months to 15 years is under way. Measles remains endemic in Uganda, with recurrent outbreaks. In 2024, cases were reported in 56 districts.
Sierra Leone declares end of mpox outbreak but stigma persists
Sierra Leone has declared the end of its mpox outbreak after more than two years, health authorities said. The country recorded over 5,000 confirmed cases and 60 deaths, with a recovery rate estimated at 99%. No new cases have been reported for more than 42 days nationwide.
Despite the epidemiological success, many survivors continue to face stigma. Reports include family rejection, job losses and difficulties reintegrating into society, driven by fear and misinformation. Health officials stressed the need for psychosocial support in the post-outbreak phase.
Some cases during the outbreak involved genital lesions, which fuelled stigma and complicated efforts to break transmission chains. Authorities say community awareness campaigns remain essential to rebuild trust. The response, supported by international partners, included the vaccination of more than 186,000 people and expanded laboratory capacity.
Ayi Renaud Dossavi

