The case highlights critical lessons regarding the initiation and management of PrEP among the young MSM. This case typifies key features of the young MSM population, characterized by frequent high-risk sexual behaviors and suboptimal PrEP utilization, making it a key population of continuous concern for PrEP intervention.
Improper use of PrEP is the primary cause of PrEP failure and subsequent HIV infection. The case reported engaging in high-frequency unprotected sexual behavior with multiple partners (≥ 4 per week), while inappropriately opting for “2-1-1” dosing, accompanied by suboptimal adherence. This case underscores the limitations of relying solely on mobile health technologies. In China, telemedicine has rapidly developed, with high acceptance, particularly among young people [12, 13]. Utilizing online advertisements on mobile applications, like WeChat, and other platforms commonly used within Chinese MSM communities could effectively increase awareness and uptake of PrEP [7, 14]. However, uptake and adherence rates are both indispensable parts of reducing HIV transmission through PrEP [15]. Insufficient outreach can result in inadequate knowledge about PrEP or behavioral misconceptions among users, leading to irregular adherence and poor compliance [5, 16]. Given the behavioral characteristics observed in this case, only high adherence to daily PrEP could offer protection against HIV infection. This indicates that the assessment before offering PrEP of the present telemedicine-based PrEP modalities is insufficient and requires further improvement. Prior to offering PrEP, a comprehensive epidemiological investigation of the patient, including sexual and substance use history, and informing about PrEP should be conducted to tailor PrEP use for individual success.
Furthermore, managing patients who prescribed PrEP via telemedicine also faces challenges. Multiple studies demonstrated adherence to PrEP is essential for preventing HIV infection. CDC guidelines recommend offer regular support and ongoing assessments for patients on PrEP [17]. The patient was prescribed and initiated PrEP via telemedicine. However, post-prescription counseling, particularly in-person consultation, was not sufficiently provided. The insufficiency of such support may have led to misunderstandings about the PrEP regimen and risk perception [18], which could have adversely affected the patient’s behavior and psychological preparedness, ultimately contributing to suboptimal adherence [19]. In recent years, China has been actively exploring mobile-based medical applications to improve communication and adherence by sending medication reminders while protecting privacy [20,21,22]. In this case, follow-up with long intervals delayed medication counseling and adherence monitoring, leading to failure to detect irregular medication in time. Therefore, developing and expanding telemedicine-based adherence interventions could offer personalized support, and additional reminders for those with low adherence could enhance their effectiveness of these interventions.
Within the framework of the current intervention model advocated by PrEP, there remains a critical need to enhance behavioral and psychological interventions. Previous research has demonstrated that attitudes towards PrEP, subjective norms, and perceived behavioral control significantly impact patients’ intentions to adhere to PrEP regimens [23,24,25]. This case could be serves as a microcosm of young MSM population, indicating the necessity of reinforcing behavioral and psychological interventions for this group to improve PrEP adherence in the future. Social media influencers and community organizations should strengthen collaborate to engage the target population in regular health education [26, 27]. They could provide services such as PrEP prescriptions, drug compliance education, psychological support, and follow-up monitoring to raise awareness of PrEP’s benefits and safety, reduce HIV and PrEP stigma, and alleviate psychological stress and discrimination.
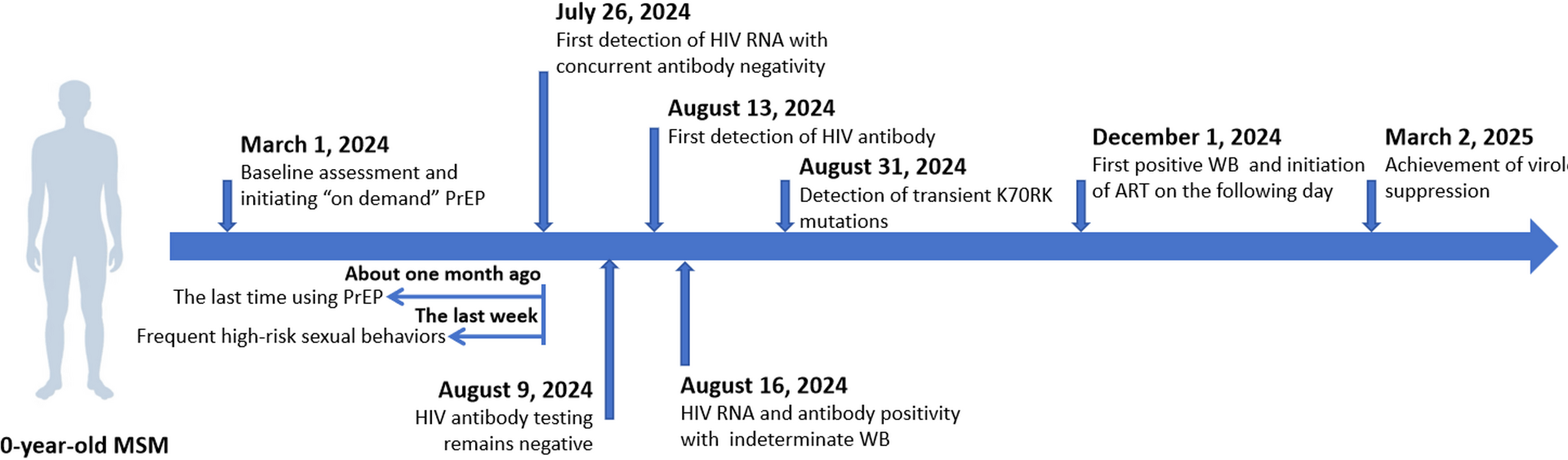
When individuals using PrEP experience breakthrough infections, the presence of residual antiretrovirals may suppress viral replication, thereby delaying seroconversion and complicating standard testing algorithms [9, 28]. This case highlights the utility of NAT in the ongoing assessment of PrEP users. Due to the short detection window and high sensitivity of NAT [29], HIV infection was promptly identified in this case, despite the viral load remaining below 1000 copies/mL one month post-detection. NAT enables earlier detection of HIV infection compared to antibody testing, facilitating the timely initiation of subsequent treatments and corresponding intervention measures, thereby aiding in the prevention of secondary transmission [30]. However, the high cost associated with HIV RNA testing limits its use for excluding primary HIV infection prior to PrEP initiation and for ongoing assessment post-initiation. Our study demonstrates that pooled RNA testing is a viable option. Utilizing the ten-in-one sample set method, it can effectively identify samples with low viral loads while reducing costs. Therefore, pooled RNA testing or RNA testing should be considered for inclusion in PrEP assessment, particularly for patients at higher epidemiological risk of HIV infection.
The transient K70KR mutation observed here reflects residual drugs may suppress wild-type virus, allowing minority-resistant variants to proliferate. K70KR is a thymidine analogue-associated mutation (TAM) that confers intermediate resistance to AZT and contributes to reduced ABC and TDF susceptibility in combination with other TAMs. Pharmacokinetic models indicate tenofovir diphosphate (TFV-DP), the active metabolites of TDF after hydrolysis and phosphorylation in vivo, very persists for several days after stopping drugs [31, 32], creating a “selection window” for resistance. The K70KR mutation impairs viral replicative capacity [33]. Upon PrEP discontinuation and clearance, wild-type strains outcompete resistant variants, explaining their disappearance by December 2024. If HIV infection with drug-resistant due to PrEP failure is not timely detected and PrEP is not carried out continuously, it may increase the risk of the transmission of drug-resistant strains [34]. Fortunately, this transient resistance mutation does not affect the subsequent therapeutic effect either. As in this case, patients with this mutation achieve virological suppression quickly when using Bictegravir/Emtricitabine/Tenofovir Alafenamide, and no drug-resistant mutations occur. Although the transient drug resistance mutations that do not damage the efficacy of HIV treatment, it should be noted the risk of the spread of drug-resistant strains.
This case underscores the urge need to optimize the present telemedicine-based PrEP modalities in China. Based on the achievements in telemedicine, it is necessary to establish a comprehensive full-course management for initiation and adherence. For PrEP users with poor adherence or high infection risk, HIV NAT is more suitable to assess infection status in early stage. Concerns about the transient drug resistance mutations after PrEP failure are unnecessary, as they do not compromise the efficacy of subsequent HIV treatment.