Harmful gut bacteria could be driving the surge in cases of deadly liver cancer, scientists have revealed in a concerning new study.
When people think of liver disease, many will say it is caused by excessive alcohol intake—but experts say anything that can increase fat in and on the liver, such as a poor diet, can raise the risk of the disease.
According to the British Liver Trust, liver disease is the only major disease to see death rates continually rising, with figures having quadrupled in the past 50 years.
But now Canadian researchers may have discovered a way of controlling blood sugar levels and reduce liver damage, especially in high-risk obese patients.
In the study, published in the journal Cell Metabolism, scientists were able to identify and isolate a molecule produced by bacteria in the gut that triggers the liver to make too much sugar and fat.
Professor Jonathan Schetzer, expert in biomedical sciences at McMaster University and study lead author, said: ‘This is a completely new way to think about treating metabolic diseases like fatty liver disease.
‘Instead of targeting hormones or the liver directly, we’re intercepting a microbial fuel source before it can do harm.’
He added: We’ve known for nearly a century that muscles and the liver exchange lactate and glucose. What we’ve discovered is a new branch of that cycle, where gut bacteria are also part of the conversation.’
It’s a common and dangerous misconception that only alcohol can cause liver scarring
In 1974 married scientists Carl and Gerty Cori demonstrated how muscles in the body produce L-lactate which pushes the liver to produce glucose, which then cycles back to fuel the muscle—known as the Cori cycle.
The Canadian researchers used this theory in the current study to analyse how a lesser known molecule called D-lactate works in the body.
They found that obese people have higher levels of this molecule, the majority of which comes from gut microbes, shown to raise blood sugar levels and liver fat more dramatically than the common L-lactate.
To see if they could stop this effect, the researchers designed a ‘gut substrate trap’ which they hoped would bind to D-lactate in the gut and prevent it from being absorbed.
They found that mice fed this biodegradable trap had lower blood glucose levels, better insulin resistance and reduced liver inflammation and fibrosis—the development of fibrous connective tissue as a response to damage—than mice who were not fed the trap.
These changes were observed without any changes being made to diet or body weight.
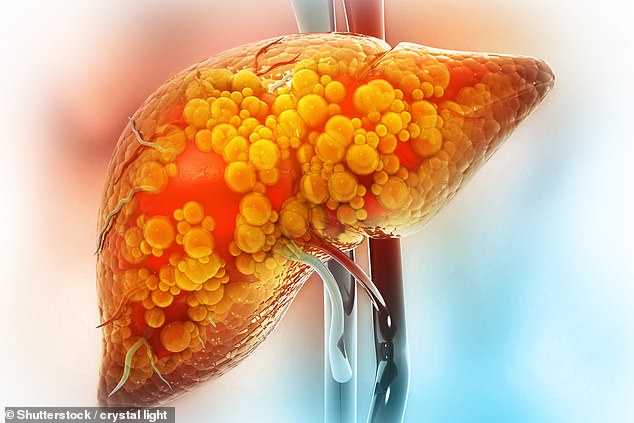
One of the most common forms of liver disease, affecting around 1 in 5 people in the UK, is metabolic dysfunction-associated steatotic liver disease (MASLD), formerly known an non-alcoholic fatty liver disease.
The condition is caused by a build-up of fat in the liver which triggers inflammation.

MALSD is becoming increasingly common, with overweight and obesity increasing the risk of the disease. Sedentary lifestyles, an ageing population and high blood pressure are also thought to be behind the surge in cases
Over time, this leads to scarring, which can eventually cause cirrhosis.
Left untreated, it can lead to liver failure or even cancer, with obese people and type 2 diabetics at higher risk of the disease.
Figures from The Liver Trust revealed there were 11,000 deaths from liver disease last year—many of which could have been prevented with early intervention and lifestyle changes.
Professor Philip Newsome, Director of the Roger Williams Institute of Liver Studies at King’s College London previously told the Daily Mail: ‘People who develop MASLD are often overweight or have diabetes.
‘We’re seeing an increase in liver disease in the UK, and the challenge is that symptoms are often unnoticeable until it’s too late.’
He added that it’s a common and dangerous misconception that only alcohol can cause liver scarring, as excess fat and uncontrolled blood sugar levels can lead to the same outcome.
Whilst MASLD does not usually cause any symptoms, meaning it is only detected when tests are carried out for a seemingly unrelated health issue, some patients will experience fatigue, malaise, and liver pain or discomfort felt in the abdomen under the right side of the ribs.
In the UK, there has been a strong sense of urgency to tackle the UK’s growing obesity crisis to alleviate pressures on the National Health Service.
According to recent data, nearly two-thirds of adults in England are overweight, with an extra 260,000 people entering the category last year.
Meanwhile, more than a quarter (26.5 per cent)—an estimated 14 million people—were classified as obese.
Last month GPs allowed to prescribe weight loss jabs, collectively known as GLP-1s for the first time in a bid to tackle the crisis.
An estimated 1.5 million people are now using weight loss jabs through the NHS or private clinics, while millions more are eligible.
