It’s the most commonly used painkiller in the world, one you’ve probably taken yourself at some point over the last few weeks.
But is paracetamol, which is used to treat everything from headaches to fevers to back pain, as safe as it appears?
The average Briton pops around 70 tablets every year – nearly six doses a month – and the latest official figures reveal the NHS in England dished out more than 15million prescriptions for the painkiller in 2024/25, at a cost of £80.6million.
But several recent studies have linked regular use of the drug to liver failure, high blood pressure, gastrointestinal bleeding and heart disease – and even to issues such as tinnitus and developmental problems such as autism and ADHD.
Some doctors now say that, while it might be fine to take a couple of paracetamol to combat a headache or any kind of pain that will pass quickly, it should not be used regularly – and certainly not for longer than a few weeks at a time – because it can cause liver damage, even at the ‘safe’ dose.
Professor Andrew Moore, a member of the respected Cochrane Collaboration’s Pain, Palliative Care and Supportive Care group – which analyses evidence from international research – writing in online publication The Conversation, said that the ‘conventional view’ that paracetamol is safe and a ‘go-to’ treatment for pain was ‘probably wrong’.
‘[The studies] we have tell us that paracetamol use is associated with increased rates of death, heart attack, stomach bleeding and kidney failure,’ he says.
‘Paracetamol is known to cause liver failure in overdose but it also causes liver failure in people taking standard doses for pain relief. The risk is only about one in a million, but it is a risk. All these different risks stack up.’

Dozens of studies have already linked paracetamol, known as acetaminophen in the US, to two neuropsychiatric conditions
His views are echoed by GPs, including Doncaster-based GP Dr Dean Eggitt, who adds: ‘People think paracetamol is harmless because it’s easy to get so people take it like Smarties. But even if you’re not exceeding the recommended amount in one day, you can still overdose.’
The dose considered ‘safe’ is 4g a day, the equivalent of taking two 500mg tablets four times in a 24-hour period.
But even just slightly exceeding the recommended dose every day for 10 days or more could be enough to cause permanent liver and kidney damage, Dr Eggitt has warned.
Reviews of the evidence also suggest that paracetamol is not even as effective as people think for pain relief.
‘For postoperative pain, perhaps one in four people benefit,’ Prof Moore writes. ‘For headache, perhaps one in ten. These are robust and trustworthy results. If paracetamol works for you, that’s great. But for most, it won’t.’
So what does the evidence say, and are you taking too much?
How paracetamol can damage the liver
It’s a startling fact: paracetamol is the leading cause of acute liver failure in adults.
In general, studies suggest taking nearly twice the daily recommended dose – around 7.5g – in 24 hours is enough to cause toxicity in the liver in some people.
This is because, as paracetamol is broken down in the body, it produces a toxic by-product called NAPQI. At low doses, or if just a couple of pills are needed to treat a headache, this doesn’t cause an issue as it can be neutralised by a protective substance called glutathione.
But at high doses, or if paracetamol is taken over a longer period, the liver can become overwhelmed, which means it can’t produce enough glutathione and damage can occur.
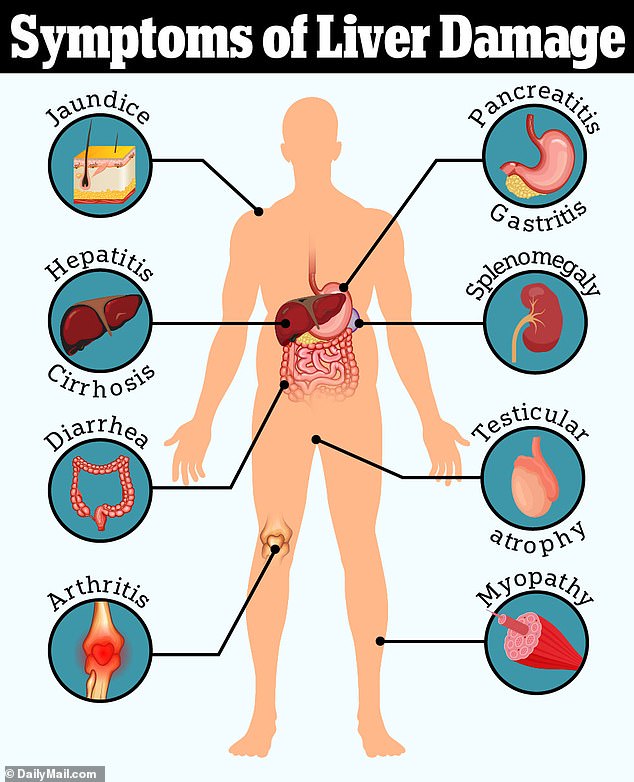
Some studies have found taking even slightly over the recommended dose for several days in a row can also lead to liver failure. The risk is particularly acute in people who are underweight, who drink alcohol or who already have some form of liver disease.
Prof Moore says part of the problem is that most people don’t know how much they’re using. He points out that soluble cold remedy products such as Lemsip or Beechams also contain paracetamol – so if these are being taken alongside paracetamol tablets it can easily lead to an accidental overdose.
Paracetamol might not even work for chronic pain
Several studies have shown that over-the-counter painkillers, including paracetamol, have little effect for conditions such as back pain and osteoarthritis.
In fact, the UK’s medicines watchdog, NICE, revised its guidelines in 2020 to say that paracetamol should not be used for chronic pain because of a lack of evidence that it worked – and that it could cause harm, such as liver toxicity, kidney damage and gastrointestinal issues, if taken regularly.
Studies looking at lower back pain and osteoarthritis specifically found it was ‘no better than placebo’ and did not improve quality of life.
Even the ‘right’ dose can raise your blood pressure – especially if you’re a woman
Paracetamol is often recommended as a ‘safer’ alternative to ibuprofen and other painkillers known as non-steroidal anti-inflammatory drugs, or NSAIDs, which are known to increase the risk of high blood pressure and heart disease if taken regularly.
But multiple studies now show that paracetamol may, in fact, have a similar effect – although the evidence is less consistent than for NSAIDs.
One 2022 study at the University of Edinburgh gave 110 patients with a history of high blood pressure the standard dose of paracetamol – two 500mg tablets, taken four times a day – over a two-week period. They were also given placebo tablets over a separate two-week period.
The researchers found their was a noticeable rise in their blood pressure during the period they were given paracetamol.
Another large US study also found chronic paracetamol use was associated with twice the risk of high blood pressure in women.
Raised blood pressure over time is linked with an increased risk of heart attacks and strokes.
Weiya Zhang, professor of epidemiology at the University of Nottingham, said: ‘Although we don’t fully know how paracetamol works, we think it may target some of the same pain receptors as NSAIDs. So, mechanistically, it’s possible it could cause a rise in blood pressure like NSAIDs are known to do.’
Paracetamol is still recommended to treat short-term pain in people with high blood pressure – but NHS and NICE guidelines recommend anyone with cardiovascular problems should take it at the lowest effective dose, for the shortest amount of time.
Could paracetamol be causing the ringing in your ears?
One in ten people suffer from tinnitus – a condition that involves hearing a ringing or buzzing noise which is not actually caused by any external source.
But researchers from the US recently found that a daily dose of paracetamol was linked to an 18 per cent increased risk of having tinnitus.
The study was observational and did not note the exact doses taken, nor did it prove paracetamol caused tinnitus. It may be, for example, that people with tinnitus may be more likely to take paracetamol to alleviate tension headaches some experience because of the condition.
But previous research has found painkillers, and particularly NSAIDs, can damage the inner ear and cause hearing loss.
Dr Sharon Curhan, from Brigham and Women’s Hospital in Boston, who led the study, said the findings should make people reconsider taking over the counter painkillers.
‘For anyone who is considering taking these types of medications regularly, it is advisable to consult with a health care professional to discuss the risks and benefits and to explore whether there are alternatives to using medication,’ she said.
Mystery over link to autism
There is emerging data that suggests an association between women who take paracetamol during pregnancy and a risk of autism and ADHD in children.
One analysis of 100,000 people by researchers from Harvard’s School of Public Health and Mount Sinai Hospital found mothers exposed to paracetamol during their pregnancies were more likely to have children with the developmental disorders.
But the study was unable to conclude how much of the painkiller the women took – and was also not proof that it caused the conditions.
Prof Zhang says: ‘It’s an observational study – more work needs to be done to see whether there is actually a link between paracetamol and autism. It’s possible the women who took paracetamol had other risk factors, too, which were not part of the study.’
Your browser does not support iframes.
Over 65? Taking paracetamol too regularly could cause your stomach to bleed
A major study found older adults prescribed paracetamol by their GP were significantly more likely to be at risk of gastrointestinal bleeding and chronic kidney disease.
The study, which tracked half a million over-65s over 20 years, found even those prescribed the painkiller twice in six months were at risk of complications including stomach ulcers, heart failure, and hypertension.
And those taking the most were more likely to end up with a burst stomach ulcer or bleeding.
Prof Zhang, who carried out the study, said: ‘The message from this and other studies should be to take the lowest dose of paracetamol that you need. Take it only as you need it, and don’t just take it continuously as that could lead to problems – particularly if you’re taking it every day, at the maximum therapeutic dose. And you need to be particularly careful if you’re over 65.’
