By Lisa Owen and Louisa Cleave
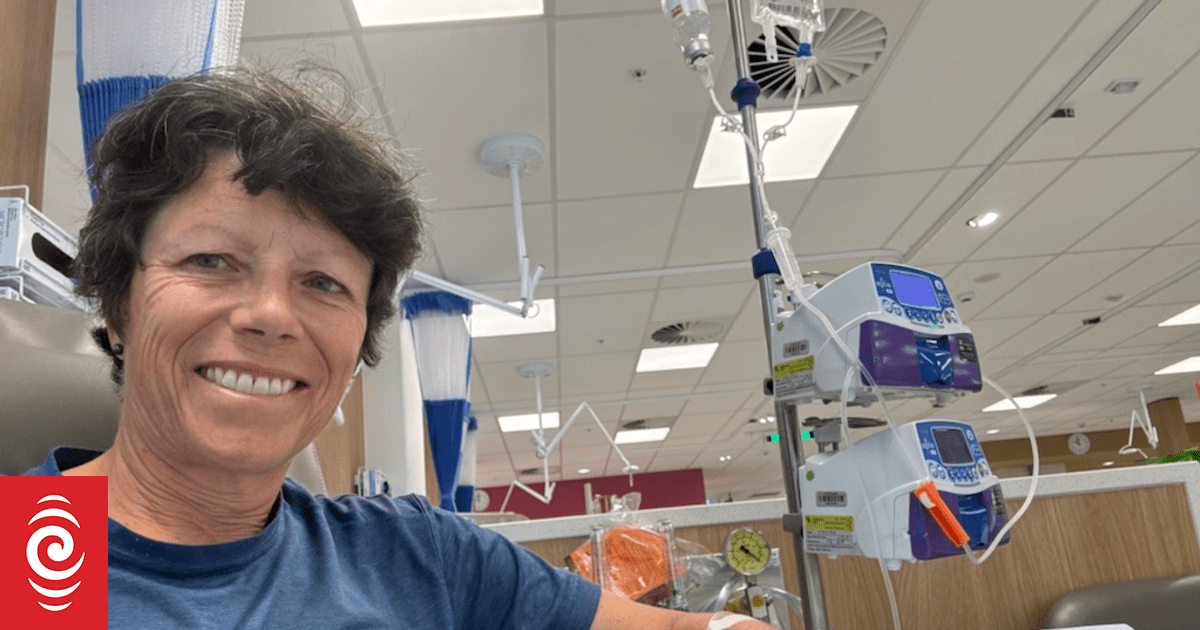
Jo Neep receiving treatment in Australia in the past year.
Photo: Supplied
A myeloma cancer patient said she felt no choice but to move to Australia to access life prolonging drugs that are not funded in New Zealand.
“I moved because I wanted life,” Jo Neep told Checkpoint.
“I could have stayed in New Zealand, and I was quite happy to stay in New Zealand until my friend kicked my **** and said, you know, you just need to look elsewhere.”
Neep had been living in Australia and visiting New Zealand regularly when she decided to move to the South Island in 2015. A couple of years later, the “fit, healthy 50-year-old” was diagnosed with myeloma and underwent a stem cell transplant.
Jo Neep receiving a stem cell transplant in 2022.
Photo: Supplied
“I was quite accepting, thinking that that medics all knew what they were talking about. But they’re only limited by what they have available to them.”
By 2022, haematologists in New Zealand were telling Neep that she could get better treatment in Australia.
The medicine they were telling her to get on was daratumumab, or dara, an immunotherapy that’s funded in Australia and costs Neep about $45 a dose. A Kiwi patient funding the drug privately pays $10,000 a dose.
“It’s a no brainer. You just have to go.”
Neep is not alone in seeking out “life” in Australia. She is one of three so-called medical migrants from Aotearoa treated by her haematologist in Sydney, while Checkpoint has also spoken to a former New Plymouth woman who returned to live in Perth to access dara.
Dara, which is funded in more than 45 other countries, has been on Pharmac’s “options for investment” list for years and is considered a high priority drug – meaning it would fund it if it had the money.
Blood cancer patients are speaking out about what they see as broken government promises to improve access to life-improving medicines.
Campaigning in 2023 Christopher Luxon said National wanted people to be able to stay in New Zealand and fight their cancer with the support of a world-class health system.
“And every minute counts in the battle against cancer and we want Kiwis to have access to better treatments here at home to give more of them the chance to beat cancer and get back to their normal lives,” he said.
Dr Rodger Tiedemann, consultant haematologist.
Photo: Supplied
Consultant haematologist Dr Rodger Tiedemann told Checkpoint about 400 people are diagnosed with myeloma every year, and many patients would benefit from dara. Trials have shown that when used in its best form, daratumumab can lead to improvements in survival of four years or more, he said.
It was sad that doctors were suggesting patients travel overseas but he understood why.
“When patients are facing a shorter life expectancy than they otherwise would, they’re going to miss out on years with their children or see them graduate or, you know, see them get through those critical teenage years. There’s a real pressure for them to try to live those years as well as they can, and that’s possible overseas, but it’s not possible in New Zealand.”
Dr Tiedemann said additional funding benefited fewer than one percent of blood cancer patients, and he questioned the Cancer Control Agency’s decision to not include daratumumab on a list of 12 medicines with substantial clinical benefits when it reported on blood cancer medicines last year.
“They stuck their head in the sands and conducted this incredibly narrow analysis that ignored a huge amount of medical literature. When they evaluated daratumumab, they ignored 90 percent of the daratumumab trials. and chose to focus only on a single trial that showed an 11-month survival benefit. And then they chose to analyse that in a way that belittle that benefit and they really ignored all of the other trial data that’s out there. Their reporting really smells of this an agenda to downplay what Kiwis are missing out on.”
The Cancer Control Agency said its analysis of blood cancer medicines was not done to decide which medicines should or should not be funded, but to highlighted gaps with Australia for drugs meeting a minimum threshold of clinical benefit. The report gave medicines a score, and the one for dara reflected clinical trial data available at the time.
The CCA noted that Pharmac’s methodology for deciding which medicines to fund considered a wider range of factors than those used in the agency’s reports.
Checkpoint asked Prime Minister Christopher Luxon to come on the programme and the request was bumped to Associate Health Minister David Seymour. His office said he could talk about access to medicines but could not speak to the National party’s cancer drugs election promise.
Asked again for an interview, the prime minister’s office sent a statement on behalf of Health Minister Simeon Brown.
It said that National was “focused on putting patients first and ensuring all New Zealanders have access to timely, quality healthcare”.
The statement pointed to a record investment in health. The government had boosted Pharmac’s budget by $604 million, which has been used for funding 66 new medicines. Mr Brown said six are for blood cancers but none of those drugs are for treating patients with myeloma.
Leukaemia and Blood Cancer NZ said only 115 patients were set to benefit from the six medicines in the first year of funding, and the clinical need remained unmet for thousands more blood cancer patients.
Neep said the government was not prioritising cancer treatment “as far as I can see”.
“I’m really grateful to the medical people in New Zealand. I know their hands are tied and it must be so frustrating for the. I know that people are agitating. All I would say is keep going, keep agitating. It has to change at some stage.”
Sign up for Ngā Pitopito Kōrero, a daily newsletter curated by our editors and delivered straight to your inbox every weekday.