A deadly ‘superbug’ that doctors struggle to detect and is resistant to most treatments is silently exploding in America, with cases of the bacterial infection skyrocketing since 2019, according to a bombshell government study.
The ‘nightmare bacteria’ known as NDM-producing CRE can cause pneumonia, bloodstream infections and untreatable fatal urinary tract infections.
It can evade even the most potent antibiotics and is spreading uncontrollably through healthcare facilities, with cases rising 18 percent over the last five years, and infections from the most dangerous strain have surged by 69 percent.
The dramatic rise threatens to undo progress against antibiotic-resistant germs and poses a serious risk to vulnerable patients in hospitals and nursing homes across the nation. In 2020, there were approximately 12,700 infections and 1,100 deaths in the US due to CRE, according to the most recent data published in 2022.
When the genes of a bacterial strain mutate to resist antibiotics, doctors have far fewer treatment options when patients present with symptoms of the infection.
The crisis is compounded by the fact that many hospitals and clinics lack the specialized tests needed to quickly identify the superbug, resulting in critical delays in initiating the correct, targeted treatments and allowing the bacteria to spread undetected.
Danielle Rankin, an epidemiologist in CDC’s Division of Healthcare Quality Promotion, said in a statement: ‘This sharp rise in NDM-CRE means we face a growing threat that limits our ability to treat some of the most serious bacterial infections.
‘Selecting the right treatment has never been more complicated, so it is vitally important that healthcare providers have access to testing to help them select the proper targeted therapies.’

In 2020, there were approximately 12,700 infections and 1,100 deaths in the US due to CRE (stock)
Your browser does not support iframes.
Carbapenem-resistant Enterobacterales (CRE) are a major public health threat, consisting of common bacteria like E. coli and Klebsiella, which can cause infections in the gut, urinary tract, lungs, and bloodstream.
They have developed resistance to carbapenem antibiotics, a class of drugs often used as a last-resort defense for severe infections.
These bacteria use various methods to reach antibiotic resistance, but the most dangerous is the production of enzymes called carbapenemases.
The enzymes act like scissors, cutting up and destroying the antibiotics, rendering them useless.
Bacteria that produce carbapenemases are especially dangerous because they can easily pass the gene for this resistance to other bacteria, rapidly spreading the threat.
The bacteria are common and often live harmlessly in the human gut. But over time, the bacteria has gained the NDM gene, which acts as armor against common antibiotics.
The gene likely emerged due to the widespread overuse and misuse of antibiotics in both medicine and agriculture, creating evolutionary pressure that allowed resistant bacteria to survive and thrive.
NDM-CRE is transmitted through direct or indirect contact in healthcare settings, including the transmission via the contaminated hands of healthcare workers, contact with contaminated surfaces or medical equipment and from person-to-person, especially among patients with weakened immune systems.
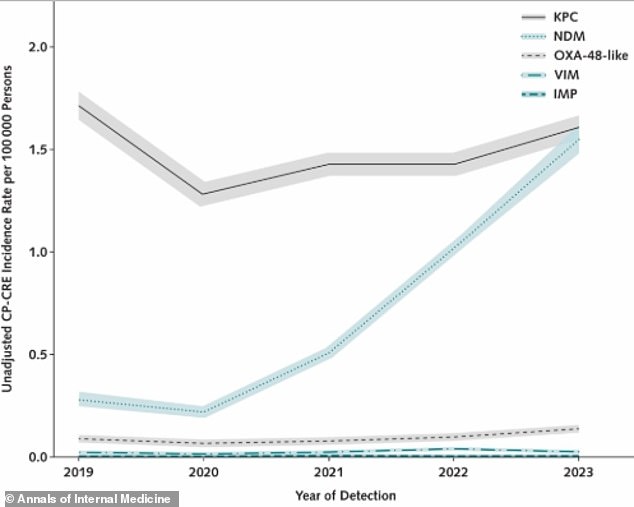
Between 2019 and 2023, dangerous CRE bacteria that are hard to treat became much more common
The NDM gene itself can also spread between different bacterial species, thereby accelerating its global expansion.
The symptoms of infection depend on which part of the body is affected.
If the bacteria cause pneumonia, a patient will experience symptoms such as cough, fever, and shortness of breath.
If the infection is in the urinary tract, it would typically present as a urinary tract infection, characterized by painful and frequent urination, and potentially accompanied by a fever.
In the most serious cases, where the bacteria enter the bloodstream, causing sepsis, symptoms escalate to high fever, chills, dangerously low blood pressure, confusion and potentially death.
The rise in NDM-CRE infections is driven by a dangerous combination of the bacteria spreading more widely and more people being vulnerable to them.
The bacteria move easily through global travel and healthcare facilities, increasing the number of carriers.
At the same time, modern medicine is saving patients with complex illnesses, but they often have weakened immune systems and need medical procedures that provide a point of entry for dangerous bacteria.

After accounting for the age of the population, one type (CP-CRE) increased by 69 percent. An even more resistant type (NDM-CRE) saw a dramatic surge of 461 percent, meaning it became more than five times as widespread
As more bacteria reach more susceptible people, the number of infections is likely to increase.
To track the spread of dangerous, drug-resistant bacteria, researchers analyzed public health data from a growing cohort of US states, 24 in 2019 and 29 in 2021.
Doctors typically have to use more specialized diagnostic testing to determine NDM-CRE as the cause of illness.
Not all states report data, and major states like California, Florida, New York, and Texas were missing, meaning the national totals are likely a significant undercount.
By calculating infection rates and utilizing statistical models, they identified a dramatic and alarming shift that occurred between 2019 and 2023.
According to a study, the overall number of CRE infections increased by 18 percent during that time.
BUT Infections caused by the most dangerous type, carbapenemase-producing CRE (CP-CRE), which are especially good at spreading and resisting treatment, surged by 69 percent among a large segment of the US population.
The authors concluded that the dramatic increase in CP-CRE is primarily driven by a 461 percent rise in infections involving the superbug NDM-CRE, meaning that while CRE infections are becoming more common overall, the specific threat from the nearly untreatable NDM variant is growing at an exceptionally rapid rate.
The data also show that infections caused by a different drug-resistant strain of Klebsiella bacteria have risen significantly, by 50 percent.
The spread of this strain is establishing a stronger foothold, specifically in Klebsiella strains.
The rise of both NDM and Klebsiella strains means that doctors are facing a wider array of resistant infections that require different, specific antibiotics, complicating treatment decisions.
Treating CP-CRE infections is always challenging, but NDM-producing strains are particularly difficult. They are resistant to even the newest antibiotics designed for such infections, severely limiting treatment options.
Historically, KPC was the most common carbapenemase in the US, but its incidence declined after 2019. By 2023, NDM had become as prevalent as KPC overall and the leading type found in E. coli.
The latest findings were published in the Annals of Internal Medicine.
More than 2.8 million antimicrobial-resistant infections occur in the US each year and over 35,000 people die as a result, according to CDC.
Researchers said: ‘The increasing diversity of carbapenemases among CRE complicates treatment, as most new U.S. Food and Drug Administration–approved antimicrobial agents active against CRE target specific carbapenemase classes.
‘Consequently, treatment should be tailored to the carbapenemase type, but carbapenemase testing is limited in clinical laboratories, and public health laboratory results may not be timely for clinical decisions.’
