Infections that are resistant to antibiotics continue to threaten global health, experts have warned—as hospitals report an alarming rise in the number of deaths driven by drug resistant strains.
According to the World Health Organisation‘s (WHO) latest surveillance report, one in six bacterial infections were resistant to antibiotic treatments in 2023.
Alarmingly, more than 40 per cent of antibiotics lost efficacy to treat common urinary tract, blood, gut and sexually-transmitted infections between 2018 and 2023, figures show.
The health watchdog added that the problem was most severe, and rapidly deteriorating, in low and middle-income countries with less robust healthcare systems, after analysing data on more than 23million infections across 104 countries.
Dr Yvan Hutin, director of the WHO’s department of antimicrobial resistance said the findings were deeply concerning.
‘As antibiotic resistance continues to rise, we are running out of treatment options and we are putting lives at risk, especially in countries where infection prevention and control is weak and access to diagnostics and effective medicine is already limited.’
Antimicrobial resistance (AMR) occurs when the pathogens which cause disease—including bacteria, viruses, fungi and parasites—evolve to withstand the drugs used to kill them, prevent and treat the disease.
In 2021 alone, 7.7million people died from bacterial infections, with drug resistance though to have contributed to more than half of the deaths and directly caused over 1million.

Gram negative bacteria such as E.coli are of particular concern because they are protected by an outer shell
By 2050, it’s estimated that 10million people will die every year as a result of resistant infections.
The report raises serious concerns about drug resistant fungal infections—previously described by the WHO as a ‘serious threat to humanity’—and bacteria protected by an outer shell like E.coli which can cause very serious infections often resulting in sepsis, blood clotting disorders, organ failure and even death.
Dr Hutin added that 40 per cent of E. coli are now resistant to the first line of treatment for such infections.
Fungal infections are also a particular concern, as well as gram negative bacteria like salmonella, because it has become increasingly difficult to develop new anti-fungal medicines—because the cells are remarkably similar to human cells.
As such, only four new antifungal drugs have been approved by regulatory authorities in the last ten years.
Dr Hutin told The Guardian: ‘These antibiotics are critical for treating severe infections and their growing ineffectiveness is narrowing the treatment options.
Dr Manica Balasegaram, from the Global Antibiotic Research and Development Partnership, echoed his concerns adding to the report that AMR has reached a ‘critical tipping point.’
‘The most difficult-to-treat gram-negative infections are now beginning to outpace antibiotic development, either because the right antibiotics are not reaching the people who need them, or because they are not being developed in the first place.
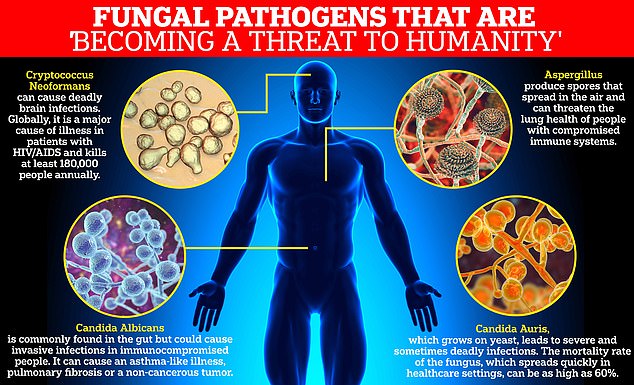
Four types of fungi were included in the World Health Organization’s critical priority group: Aspergillus fumigatus, Candida albicans, Cryptococcus neoformans and Candida Auris
‘It’s not enough to develop new antibiotics, they have to be the right ones, those that target infections that have the greatests public health impact.
‘We are failing to replace the antibiotics that are being lost to resistance, and this latests report shows that the consequences of that are now finally beginning to be felt.’
The experts added that developing new antibiotics is not enough, suggesting that there needs to be a better global effort to prevent infection through cleaner water, better sanitation and hygiene and vaccination to ‘avoid the tipping point’.
Share or comment on this article:
WHO warns of increase in antibiotic-resistant infections – with STIs, UTIs and gut bugs becoming harder to treat
