Liver, kidney, heart and lung transplants could soon be a thing of the past as work begins on a ‘natural’ cell treatment
Liver, kidney, heart and lung transplants could soon be a thing of the past as scientists embark on an “exciting” cell therapy project they hope will render key organ replacements redundant.
It could be available to patients in as little as five years, the scientist leading the project believes, and benefit not only organ transplant patients but also people suffering from conditions including autoimmune liver diseases, Crohn’s, colitis, rheumatoid arthritis, multiple sclerosis and pemphigus.
Currently, transplant patients typically require lifelong immunosuppression treatment to ensure their donated organs are not rejected by the body.
This ongoing suppression of the immune system, using powerful steroids or drugs, can lead to severe side effects, including osteoporosis, hypertension, diabetes, kidney failure and risk of cancer, as well as a reduced resilience against everyday colds, flus and other bugs.
New FeatureIn ShortQuick Stories. Same trusted journalism.
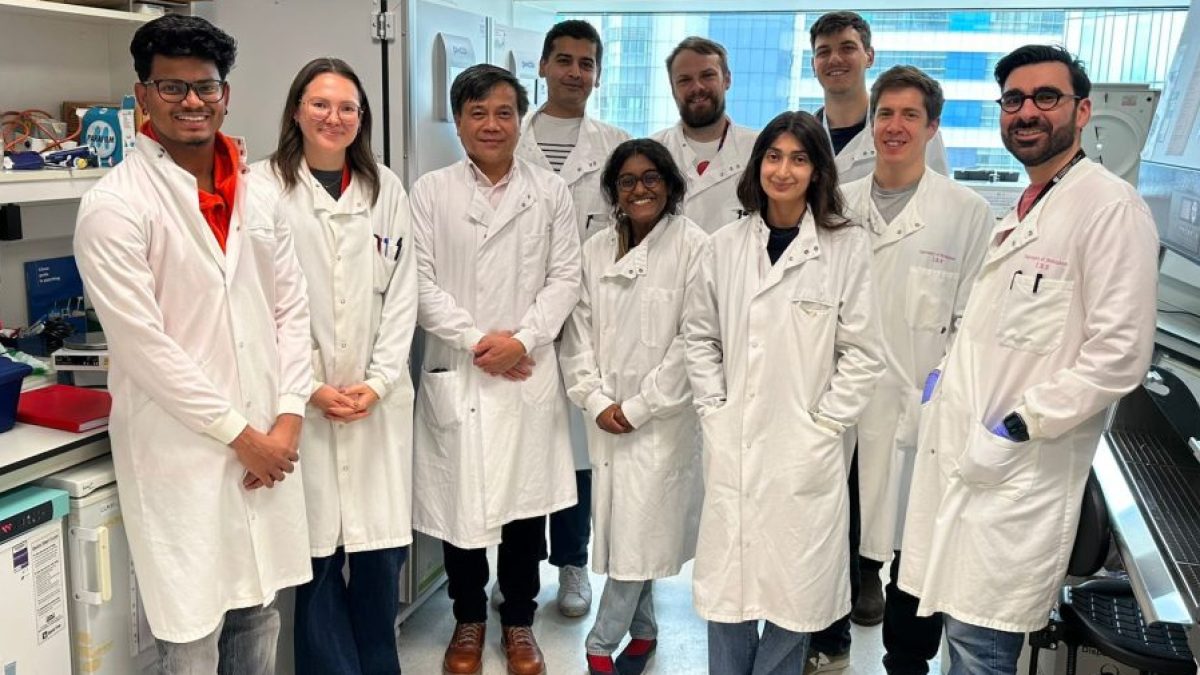
Now a team of scientists led by Professor Ye Htun Oo, of the University of Birmingham, believe a natural treatment method they are developing – using a patient’s own “good” cells to combat “bad” cells – will replace this lifelong treatment – and even the need for a transplant itself.
The NHS carries out around 4,600 organ transplants a year, while more than 8,000 people are on the transplant waiting list. Given that each liver transplant alone costs approximately £80,000 to £100,000, the new treatment could save the NHS hundreds of millions of pounds.
How it works
The research team is focusing on cellular therapy where regulatory T cells – white blood cells that originate in the bone marrow and play a crucial role in the immune system to fight infections and cancer – are harvested from a patient, multiplied, made more effective and then loaded back in to defeat rogue cells that attack the body.
Professor Oo’s specialism is autoimmune liver diseases. Other teams around the world are carrying out similar work to use regulatory T cells to treat other autoimmune diseases, with more than 200 clinical trials under way.
“In the next five to 10 years, regulatory T-cell treatment will be available for autoimmune liver disease patients,” said the professor.
Recently, his team was awarded £3.83m from the Wellcome Trust to advance their research into cellular therapy over the next eight years.
“Until now, we have been able to help organ donor recipients and people with autoimmune diseases only through the use of steroids and other severe immunosuppressive treatments.
“Regulatory T-cell therapy will save and prolong many lives. People may no longer need organ transplants at all, and if they do, they will no longer need lifelong immunosuppression treatments.”
 Professor Oo alongside Professor Shimon Sakaguchi, left, of the University of Osaka. Professor Sakaguchi discovered regulatory T cells in 1995 and was jointly awarded the Nobel Prize in Physiology or Medicine this month
Professor Oo alongside Professor Shimon Sakaguchi, left, of the University of Osaka. Professor Sakaguchi discovered regulatory T cells in 1995 and was jointly awarded the Nobel Prize in Physiology or Medicine this month
He described it as “a game-changer” for people suffering from autoimmune illnesses and said it would save the NHS money: “Each liver transplant costs approximately £80,000 to £100,000. Preventing autoimmune liver disease through regulatory T-cell therapy could substantially reduce the progression to cirrhosis and the need for liver transplantation, offering both clinical and economic benefits.”
Professor Douglas Thorburn, consultant hepatologist at The Royal Free Hospital in London, and clinical adviser to the British Liver Trust, said the new cell treatment could represent “a major advance for patients who currently rely on long-term immunosuppression medication”.
But he added: “It’s important to note that concept is yet to be fully explored but it is exciting that Professor Oo will be leading this programme from the UK to investigate the possibility.
“Further laboratory and clinical studies, including large-scale clinical trials, will be needed to confirm both the safety and long-term effectiveness of this approach in diverse patient populations. Until such data are available, standard immunosuppressive treatments remain the established and evidence-based option for patients.”
To carry out the work needed to bring cellular therapy to market, Professor Oo plans to use new facilities at the Precision Health Technologies Accelerator, at the University of Birmingham’s Health Innovation Campus – part of the city’s fast-emerging Life Sciences Quarter.
T cells – the body’s natural defence force
T cells were discovered in the early 1960s by French-Australian immunologist Jacques Miller. His experiments in 1961 showed that the thymus gland was crucial for the development of the adaptive immune system, as mice that had their thymus removed after birth became immunodeficient.
This discovery established that thymus-derived lymphocytes, or “T cells”, were essential for fighting infections and rejecting foreign tissue grafts, leading to the foundation of modern immunology.
Professor Shimon Sakaguchi, of the University of Osaka in Japan, discovered regulatory T cells – a population of T cells that prevented the immune system from over-reacting and causing autoimmune diseases – in 1995.
 Professor Oo said access to a Midlands-based manufacturing facility and industry partnership will be ‘essential’ to begin cell therapy production
Professor Oo said access to a Midlands-based manufacturing facility and industry partnership will be ‘essential’ to begin cell therapy production
Professor Oo has now teamed up with Professor Sakaguchi in his work to achieve effective regulatory T-cell cellular therapy, specifically to better understand these cells’ biology in tissue, such as the liver, with a view to bringing the treatment to market as soon as possible.
Professor Sakaguchi was jointly awarded the Nobel Prize in Physiology or Medicine this month in recognition of his trailblazing work in this area.
The Nobel committee awarded him the prize alongside Mary Brunkow, at the Institute for Systems Biology, and Fred Ramsdell, at Sonoma Biotherapeutics, both in the US, “for their discoveries concerning peripheral immune tolerance”.
Their discoveries have laid the foundation for a new field of research and led to the development of new treatments for autoimmune diseases and cancers.