Goutman SA, Hardiman O, Al-Chalabi A, Chió A, Savelieff MG, Kiernan MC, Feldman EL. Emerging insights into the complex genetics and pathophysiology of amyotrophic lateral sclerosis. Lancet Neurol. 2022;21(5):465–79. https://doi.org/10.1016/S1474-4422(21)00414-2.
Dharmadasa T, Henderson RD, Talman PS, Macdonell RA, Mathers S, Schultz DW, et al. Motor neurone disease: progress and challenges. Med J Aust. 2017;206(8):357–62.
Rooney J, Byrne S, Heverin M, Tobin K, Dick A, Donaghy C, et al. A multidisciplinary clinic approach improves survival in ALS: a comparative study of ALS in Ireland and Northern Ireland. J Neurol Neurosurg Psychiatry. 2015;86(5):496–501.
Wobst HJ, Mack KL, Brown DG, Brandon NJ, Shorter J. The clinical trial landscape in amyotrophic lateral sclerosis—past, present, and future. Med Res Rev. 2020;40(4):1352–84.
Bensimon G, Lacomblez L, Meininger Vf, Group ALRS. A controlled trial of riluzole in amyotrophic lateral sclerosis. N Engl J Med. 1994;330(9):585–91.
Lacomblez L, Bensimon G, Meininger V, Leigh PN, Guillet P, Amyotrphic lateral sclerosis/riluzole study group II. Dose-ranging study of riluzole in amyotrophic lateral sclerosis. Lancet. 1996;347(9013):1425–31.
Hinchcliffe M, Smith A. Riluzole: real-world evidence supports significant extension of median survival times in patients with amyotrophic lateral sclerosis. Degener Neurol Neuromuscul Dis. 2017. https://doi.org/10.2147/DNND.S135748.
Jablonski MR, Markandaiah SS, Jacob D, Meng NJ, Li K, Gennaro V, et al. Inhibiting drug efflux transporters improves efficacy of ALS therapeutics. Ann Clin Transl Neurol. 2014;1(12):996–1005.
Abe K, Aoki M, Tsuji S, Itoyama Y, Sobue G, Togo M, et al. Safety and efficacy of edaravone in well defined patients with amyotrophic lateral sclerosis: a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2017;16(7):505–12.
Hirai M, Ishizaki K, Matsuda H, Sobue G. Surveillance of using novel free radical scavenger, edaravone to investigate survival effect for ALS patients in Japan (SUNRISE Japan): a study design. J Neurol Sci. 2017;381:207.
Shefner J, Heiman-Patterson T, Pioro EP, Wiedau-Pazos M, Liu S, Zhang J, et al. Long-term edaravone efficacy in amyotrophic lateral sclerosis: post-hoc analyses of study 19 (MCI186-19). Muscle Nerve. 2020;61(2):218–21.
Witzel S, Maier A, Steinbach R, Grosskreutz J, Koch JC, Sarikidi A, et al. Safety and effectiveness of long-term intravenous administration of edaravone for treatment of patients with amyotrophic lateral sclerosis. JAMA Neurol. 2022;79(2):121–30.
Mejzini R, Flynn LL, Pitout IL, Fletcher S, Wilton SD, Akkari PA. ALS genetics, mechanisms, and therapeutics: where are we now? Front Neurosci. 2019;13:1310.
Dharmadasa T, Scaber J, Edmond E, Marsden R, Thompson A, Talbot K, et al. Genetic testing in motor neurone disease. Pract Neurol. 2022;22(2):107–16.
Özgiray E, Serarslan Y, Öztürk OH, Altaş M, Aras M, Söğüt S, et al. Protective effects of edaravone on experimental spinal cord injury in rats. Pediatr Neurosurg. 2011;47(4):254–60.
Miller T, Cudkowicz M, Shaw PJ, Andersen PM, Atassi N, Bucelli RC, et al. Phase 1–2 trial of antisense oligonucleotide tofersen for SOD1 ALS. N Engl J Med. 2020;383(2):109–19.
Miller TM, Cudkowicz ME, Genge A, Shaw PJ, Sobue G, Bucelli RC, et al. Trial of antisense oligonucleotide tofersen for SOD1 ALS. N Engl J Med. 2022;387(12):1099–110.
Mead RJ, Shan N, Reiser HJ, Marshall F, Shaw PJ. Amyotrophic lateral sclerosis: a neurodegenerative disorder poised for successful therapeutic translation. Nat Rev Drug Discov. 2023;22(3):185–212.
Neel DV, Baselga-Garriga C, Benson M, Keegan M, Chase M, D’Agostino D, Drake K, Hagar JL, Hasenoehrl MG, Kulesa‐Kelley J, Leite A. Multicenter expanded access program for access to investigational products for amyotrophic lateral sclerosis. Muscle Nerve. 2024;70(2):232–39.
Biogen. Biogen and ionis announce topline phase 1/2 Study results of investigational drug in amyotrophic lateral sclerosis. 2024. Available from: https://investors.biogen.com/news-releases/news-release-details/biogen-and-ionis-announce-topline-phase-12-study-results.
Biogen. Biogen and ionis announce topline phase 1 study results of investigational drug in C9orf72 amyotrophic lateral sclerosis. 2022. Available from: https://investors.biogen.com/news-releases/news-release-details/biogen-and-ionis-announce-topline-phase-1-study-results.
van den Berg LH, Rothstein JD, Shaw PJ, Babu S, Benatar M, Bucelli RC, et al. Safety, tolerability, and pharmacokinetics of antisense oligonucleotide BIIB078 in adults with C9orf72-associated amyotrophic lateral sclerosis: a phase 1, randomised, double blinded, placebo-controlled, multiple ascending dose study. Lancet Neurol. 2024;23(9):901–12.
Wave Life Sciences. Wave Life Sciences announces topline results from phase 1b/2a FOCUS-C9 study of WVE-004 for C9orf72-associated amyotrophic lateral sclerosis and frontotemporal dementia. 2023. Available from: https://ir.wavelifesciences.com/news-releases/news-release-details/wave-life-sciences-announces-topline-results-phase-1b2a-focus-c9.
Amylyx. Amylyx pharmaceuticals announces formal intention to remove RELYVRIO®/ALBRIOZA™ from the market; provides updates on access to therapy, pipeline, corporate restructuring, and strategy. 2024. Available from: https://www.amylyx.com/news/amylyx-pharmaceuticals-announces-formal-intention-to-remove-relyvrior/albriozatm-from-the-market-provides-updates-on-access-to-therapy-pipeline-corporate-restructuring-and-strategy.
Camu W, Mickunas M, Veyrune JL, Payan C, Garlanda C, Locati M, et al. Repeated 5-day cycles of low dose aldesleukin in amyotrophic lateral sclerosis (IMODALS): a phase 2a randomised, double-blind, placebo-controlled trial. EBioMedicine. 2020;59:102844.
Bensimon G, Leigh PN, Tree T, Malaspina A, Payan CAM, Pham H-P, et al. Efficacy and safety of low-dose IL-2 as an add-on therapy to riluzole (MIROCALS): a phase 2b, double-blind, randomised, placebo-controlled trial. Lancet. 2025;405(10492):1837–50.
Rulten SL, Grose RP, Gatz SA, Jones JL, Cameron AJM. The future of precision oncology. Int J Mol Sci. 2023. https://doi.org/10.3390/ijms241612613.
National Insitute of Health. National Cancer Institute 2024. Cited 2024. Available from: https://www.cancer.gov/about-cancer/treatment/types/targeted-therapies/approved-drug-list#targeted-therapy-approved-for-lung-cancer.
Hofmarcher T, Malmberg C, Lindgren P. A global analysis of the value of precision medicine in oncology–the case of non-small cell lung cancer. Front Med. 2023;10:1119506.
Benatar M, Wuu J, Andersen PM, Bucelli RC, Andrews JA, Otto M, et al. Design of a randomized, placebo-controlled, phase 3 trial of Tofersen initiated in clinically presymptomatic SOD1 variant carriers: the ATLAS study. Neurotherapeutics. 2022;19(4):1248–58.
Benatar M, Wuu J, Andersen PM, Lombardi V, Malaspina A. Neurofilament light: a candidate biomarker of presymptomatic amyotrophic lateral sclerosis and phenoconversion. Ann Neurol. 2018;84(1):130–9.
Benatar M, Wuu J, Lombardi V, Jeromin A, Bowser R, Andersen PM, et al. Neurofilaments in pre-symptomatic ALS and the impact of genotype. Amyotroph Lateral Scler Frontotemporal Degener. 2019;20(7–8):538–48.
Opie-Martin S, Iacoangeli A, Topp SD, Abel O, Mayl K, Mehta PR, et al. The SOD1-mediated ALS phenotype shows a decoupling between age of symptom onset and disease duration. Nat Commun. 2022;13(1):6901.
Wiesenfarth M, Dorst J, Brenner D, Elmas Z, Parlak Ö, Uzelac Z, et al. Effects of tofersen treatment in patients with SOD1-ALS in a real-world setting; a 12-month multicenter cohort study from the German early access program. eClinicalMedicine. 2024;69:102495.
He D, Xu Y, Liu M, Cui L. The inflammatory puzzle: piecing together the links between neuroinflammation and amyotrophic lateral sclerosis. Aging Dis. 2024;15(1):96.
Yu CH, Davidson S, Harapas CR, Hilton JB, Mlodzianoski MJ, Laohamonthonkul P, et al. TDP-43 triggers mitochondrial DNA release via mPTP to activate cGAS/STING in ALS. Cell. 2020;183(3):636–49. e18.
Gille B, De Schaepdryver M, Dedeene L, Goossens J, Claeys KG, Van Den Bosch L, et al. Inflammatory markers in cerebrospinal fluid: independent prognostic biomarkers in amyotrophic lateral sclerosis? J Neurol Neurosurg Psychiatry. 2019;90(12):1338–46.
Thonhoff JR, Beers DR, Zhao W, Pleitez M, Simpson EP, Berry JD, et al. Expanded autologous regulatory T-lymphocyte infusions in ALS: a phase I, first-in-human study. Neurol Neuroimmunol Neuroinflamm. 2018;5(4):e465.
Cheng G, Yu A, Malek TR. T-cell tolerance and the multi-functional role of IL-2R signaling in T-regulatory cells. Immunol Rev. 2011;241(1):63–76.
Toomer KH, Lui JB, Altman NH, Ban Y, Chen X, Malek TR. Essential and non-overlapping IL-2Rα-dependent processes for thymic development and peripheral homeostasis of regulatory T cells. Nat Commun. 2019;10(1):1037.
van den Berg LH, Sorenson E, Gronseth G, Macklin EA, Andrews J, Baloh RH, et al. Revised Airlie House consensus guidelines for design and implementation of ALS clinical trials. Neurology. 2019;92(14):e1610–23.
Giovannelli I, Bayatti N, Brown A, Wang D, Mickunas M, Camu W, et al. Amyotrophic lateral sclerosis transcriptomics reveals immunological effects of low-dose interleukin-2. Brain Commun. 2021;3(3):fcab141.
Forlenza OV, De-Paula VJR, Diniz BSO. Neuroprotective effects of lithium: implications for the treatment of Alzheimer’s disease and related neurodegenerative disorders. ACS Chem Neurosci. 2014;5(6):443–50.
Van Eijk RP, Jones AR, Sproviero W, Shatunov A, Shaw PJ, Leigh PN, et al. Meta-analysis of pharmacogenetic interactions in amyotrophic lateral sclerosis clinical trials. Neurology. 2017;89(18):1915–22.
Willemse SW, Roes KCB, Van Damme P, Hardiman O, Ingre C, Povedano M, et al. Lithium carbonate in amyotrophic lateral sclerosis patients homozygous for the C-allele at SNP rs12608932 in UNC13A: protocol for a confirmatory, randomized, group-sequential, event-driven, double-blind, placebo-controlled trial. Trials. 2022;23(1):978.
Feldman EL, Goutman SA, Petri S, Mazzini L, Savelieff MG, Shaw PJ, Sobue, G. Amyotrophic lateral sclerosis. Lancet. 400(10360):1363–1380. https://doi.org/10.1016/S0140-6736(22)01272-7.
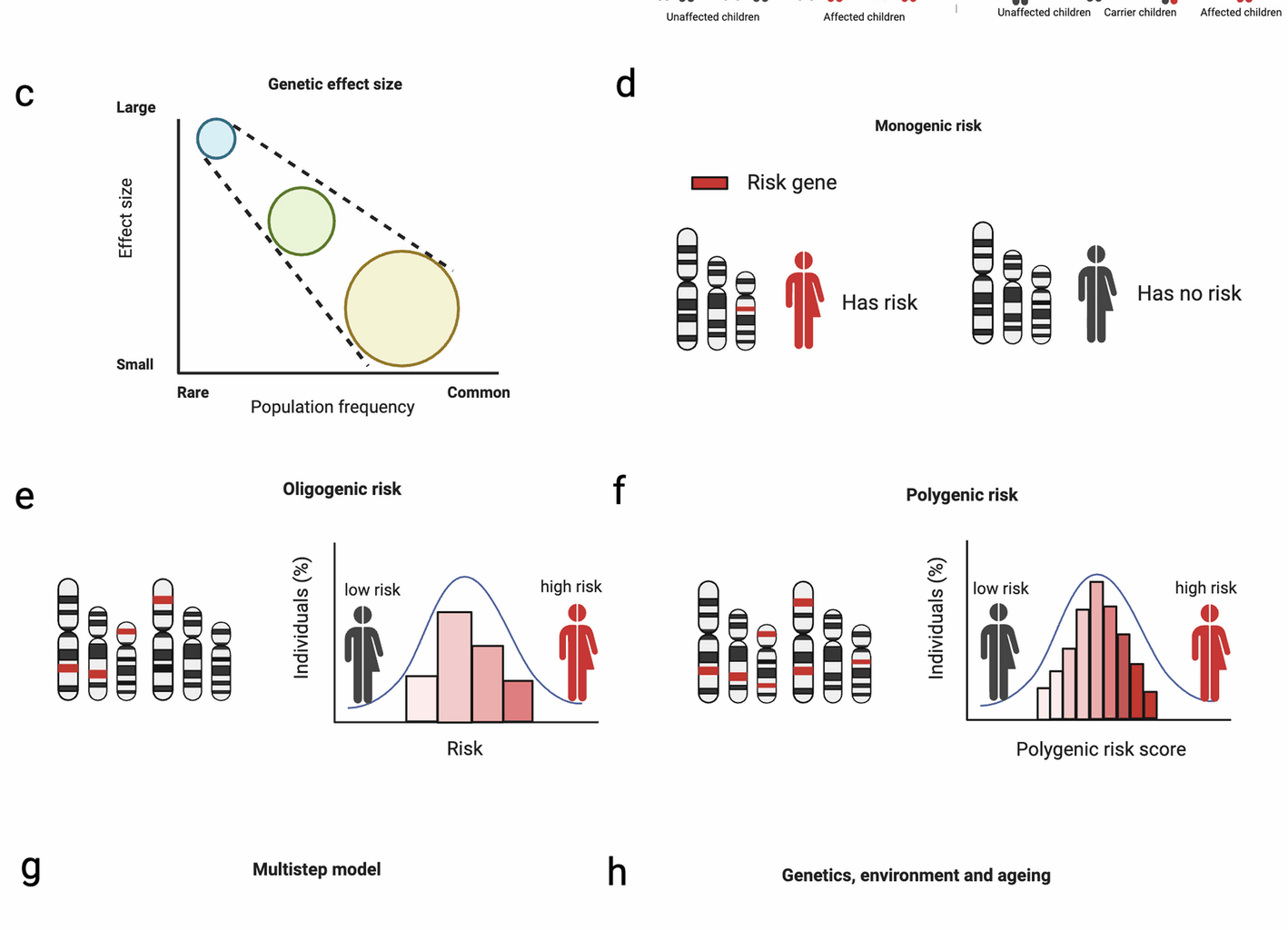
Ryan M, Heverin M, McLaughlin RL, Hardiman O. Lifetime risk and heritability of amyotrophic lateral sclerosis. JAMA Neurol. 2019;76(11):1367–74.
Al-Chalabi A, Fang F, Hanby MF, Leigh PN, Shaw CE, Ye W, et al. An estimate of amyotrophic lateral sclerosis heritability using twin data. J Neurol Neurosurg Psychiatry. 2010;81(12):1324–6.
Dekker AM, Diekstra FP, Pulit SL, Tazelaar GHP, van der Spek RA, van Rheenen W, et al. Exome array analysis of rare and low frequency variants in amyotrophic lateral sclerosis. Sci Rep. 2019;9(1):5931.
Morgan S, Shatunov A, Sproviero W, Jones AR, Shoai M, Hughes D, et al. A comprehensive analysis of rare genetic variation in amyotrophic lateral sclerosis in the UK. Brain. 2017;140(6):1611–8.
Theunissen F, Flynn LL, Anderton RS, Mastaglia F, Pytte J, Jiang L, et al. Structural variants may be a source of missing heritability in sALS. Front Neurosci. 2020;14:47.
Hop PJ, Zwamborn RA, Hannon E, Shireby GL, Nabais MF, Walker EM, et al. Genome-wide study of DNA methylation shows alterations in metabolic, inflammatory, and cholesterol pathways in ALS. Sci Transl Med. 2022;14(633):eabj0264.
Al-Chalabi A. Perspective: don’t keep it in the family. Nature. 2017;550(7676):S112-S.
Al-Chalabi A, Lewis CM. Modelling the effects of penetrance and family size on rates of sporadic and familial disease. Hum Hered. 2011;71(4):281–8.
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17(5):405–24.
Mehta PR, Iacoangeli A, Opie-Martin S, van Vugt JJ, Al Khleifat A, Bredin A, et al. The impact of age on genetic testing decisions in amyotrophic lateral sclerosis. Brain. 2022;145(12):4440–7.
Spargo TP, Opie-Martin S, Bowles H, Lewis CM, Iacoangeli A, Al-Chalabi A. Calculating variant penetrance from family history of disease and average family size in population-scale data. Genome Med. 2022;14(1):141.
Akçimen F, Lopez ER, Landers JE, Nath A, Chiò A, Chia R, et al. Amyotrophic lateral sclerosis: translating genetic discoveries into therapies. Nat Rev Genet. 2023;24(9):642–58.
Rosen DR, Siddique T, Patterson D, Figlewicz DA, Sapp P, Hentati A, et al. Mutations in Cu/Zn superoxide dismutase gene are associated with familial amyotrophic lateral sclerosis. Nature. 1993;362(6415):59.
Chen Y-Z, Bennett CL, Huynh HM, Blair IP, Puls I, Irobi J, et al. DNA/RNA helicase gene mutations in a form of juvenile amyotrophic lateral sclerosis (ALS4). Am J Hum Genet. 2004;74(6):1128–35.
Greenway MJ, Andersen PM, Russ C, Ennis S, Cashman S, Donaghy C, et al. ANG mutations segregate with familial and’sporadic’amyotrophic lateral sclerosis. Nat Genet. 2006;38(4):411.
Vance C, Rogelj B, Hortobágyi T, De Vos KJ, Nishimura AL, Sreedharan J, et al. Mutations in FUS, an RNA processing protein, cause familial amyotrophic lateral sclerosis type 6. Science. 2009;323(5918):1208–11.
Kwiatkowski T Jr., Bosco D, Leclerc A, Tamrazian E, Vanderburg C, Russ C, et al. Mutations in the FUS/TLS gene on chromosome 16 cause familial amyotrophic lateral sclerosis. Science. 2009;323(5918):1205–8.
Kabashi E, Valdmanis PN, Dion P, Spiegelman D, McConkey BJ, Velde CV, et al. TARDBP mutations in individuals with sporadic and familial amyotrophic lateral sclerosis. Nat Genet. 2008;40(5):572–4.
Sreedharan J, Blair IP, Tripathi VB, Hu X, Vance C, Rogelj B, et al. TDP-43 mutations in familial and sporadic amyotrophic lateral sclerosis. Science. 2008;319(5870):1668–72.
Simpson CL, Lemmens R, Miskiewicz K, Broom WJ, Hansen VK, van Vught PW, et al. Variants of the elongator protein 3 (ELP3) gene are associated with motor neuron degeneration. Hum Mol Genet. 2008;18(3):472–81.
Elden AC, Kim H-J, Hart MP, Chen-Plotkin AS, Johnson BS, Fang X, et al. Ataxin-2 intermediate-length polyglutamine expansions are associated with increased risk for ALS. Nature. 2010;466(7310):1069.
Ticozzi N, Vance C, Leclerc A, Keagle P, Glass J, McKenna-Yasek D, et al. Mutational analysis reveals the FUS homolog TAF15 as a candidate gene for familial amyotrophic lateral sclerosis. Am J Med Genet B Neuropsychiatr Genet. 2011;156(3):285–90.
Neumann M, Bentmann E, Dormann D, Jawaid A, DeJesus-Hernandez M, Ansorge O, et al. FET proteins TAF15 and EWS are selective markers that distinguish FTLD with FUS pathology from amyotrophic lateral sclerosis with FUS mutations. Brain. 2011;134(9):2595–609.
Renton AE, Majounie E, Waite A, Simón-Sánchez J, Rollinson S, Gibbs JR, et al. A hexanucleotide repeat expansion in C9ORF72 is the cause of chromosome 9p21-linked ALS-FTD. Neuron. 2011;72(2):257–68.
DeJesus-Hernandez M, Mackenzie IR, Boeve BF, Boxer AL, Baker M, Rutherford NJ, et al. Expanded GGGGCC hexanucleotide repeat in noncoding region of C9ORF72 causes chromosome 9p-linked FTD and ALS. Neuron. 2011;72(2):245–56.
Kim HJ, Kim NC, Wang Y-D, Scarborough EA, Moore J, Diaz Z, et al. Mutations in prion-like domains in hnRNPA2B1 and hnRNPA1 cause multisystem proteinopathy and ALS. Nature. 2013;495(7442):467–73.
Droppelmann CA, Wang J, Campos-Melo D, Keller B, Volkening K, Hegele RA, et al. Detection of a novel frameshift mutation and regions with homozygosis within ARHGEF28 gene in familial amyotrophic lateral sclerosis. Amyotroph Lateral Scler Frontotemporal Degener. 2013;14(5–6):444–51.
Song Y, Lin F, Ye CH, Huang H, Li X, Yao X, et al. Rare, low-frequency and common coding variants of ARHGEF28 gene and their association with sporadic amyotrophic lateral sclerosis. Neurobiol Aging. 2020;87:138. e1-. e6.
Johnson JO, Pioro EP, Boehringer A, Chia R, Feit H, Renton AE, et al. Mutations in the Matrin 3 gene cause familial amyotrophic lateral sclerosis. Nat Neurosci. 2014;17(5):664–6.
Kaneb HM, Folkmann AW, Belzil VV, Jao L-E, Leblond CS, Girard SL, et al. Deleterious mutations in the essential mRNA metabolism factor, hGle1, in amyotrophic lateral sclerosis. Hum Mol Genet. 2015;24(5):1363–73.
Li Y, Sun B, Wang Z, He Z, Yang F, Wang H, et al. Mutation screening of the GLE1 gene in a large Chinese cohort of amyotrophic lateral sclerosis patients. Front Neurosci. 2021;15:595775.
Bannwarth S, Ait-El-Mkadem S, Chaussenot A, Genin EC, Lacas-Gervais S, Fragaki K, et al. A mitochondrial origin for frontotemporal dementia and amyotrophic lateral sclerosis through CHCHD10 involvement. Brain. 2014;137(8):2329–45.
Cirulli ET, Lasseigne BN, Petrovski S, Sapp PC, Dion PA, Leblond CS, et al. Exome sequencing in amyotrophic lateral sclerosis identifies risk genes and pathways. Science. 2015;347(6229):1436–41.
Kenna KP, Van Doormaal PT, Dekker AM, Ticozzi N, Kenna BJ, Diekstra FP, et al. NEK1 variants confer susceptibility to amyotrophic lateral sclerosis. Nat Genet. 2016;48(9):1037.
Brenner D, Müller K, Wieland T, Weydt P, Böhm S, Lule D, et al. NEK1 mutations in familial amyotrophic lateral sclerosis. Brain. 2016;139(5):e28-e.
Van Rheenen W, Shatunov A, Dekker AM, McLaughlin RL, Diekstra FP, Pulit SL, et al. Genome-wide association analyses identify new risk variants and the genetic architecture of amyotrophic lateral sclerosis. Nat Genet. 2016;48:1043.
Yang Y, Hentati A, Deng H-X, Dabbagh O, Sasaki T, Hirano M, et al. The gene encoding alsin, a protein with three guanine-nucleotide exchange factor domains, is mutated in a form of recessive amyotrophic lateral sclerosis. Nat Genet. 2001;29(2):160–5.
Chow CY, Landers JE, Bergren SK, Sapp PC, Grant AE, Jones JM, et al. Deleterious variants of FIG4, a phosphoinositide phosphatase, in patients with ALS. Am J Hum Genet. 2009;84(1):85–8.
Orlacchio A, Babalini C, Borreca A, Patrono C, Massa R, Basaran S, et al. Spatacsin mutations cause autosomal recessive juvenile amyotrophic lateral sclerosis. Brain. 2010;133(2):591–8.
Smith BN, Topp SD, Fallini C, Shibata H, Chen H-J, Troakes C, et al. Mutations in the vesicular trafficking protein annexin A11 are associated with amyotrophic lateral sclerosis. Sci Transl Med. 2017;9(388):eaad9157.
Spataro R, Kousi M, Farhan SM, Willer JR, Ross JP, Dion PA, et al. Mutations in ATP13A2 (PARK9) are associated with an amyotrophic lateral sclerosis-like phenotype, implicating this locus in further phenotypic expansion. Hum Genomics. 2019;13:1–10.
Dewan R, Scholz SW, Chiò A, Traynor BJ. Highlighting the clinical potential of HTT repeat expansions in frontotemporal dementia and amyotrophic lateral sclerosis. Neuron. 2021;109(12):1947–8.
Megat S, Mora N, Sanogo J, Roman O, Catanese A, Alami NO, et al. Integrative genetic analysis illuminates ALS heritability and identifies risk genes. Nat Commun. 2023;14(1):342.
Nishimura AL, Mitne-Neto M, Silva HC, Richieri-Costa A, Middleton S, Cascio D, et al. A mutation in the vesicle-trafficking protein VAPB causes late-onset spinal muscular atrophy and amyotrophic lateral sclerosis. Am J Hum Genet. 2004;75(5):822–31.
Parkinson N, Ince P, Smith M, Highley R, Skibinski G, Andersen P, et al. ALS phenotypes with mutations in CHMP2B (charged multivesicular body protein 2B). Neurology. 2006;67(6):1074–7.
Skibinski G, Parkinson NJ, Brown JM, Chakrabarti L, Lloyd SL, Hummerich H, et al. Mutations in the endosomal ESCRTIII-complex subunit CHMP2B in frontotemporal dementia. Nat Genet. 2005;37(8):806–8.
Maruyama H, Morino H, Ito H, Izumi Y, Kato H, Watanabe Y, et al. Mutations of optineurin in amyotrophic lateral sclerosis. Nature. 2010;465(7295):223.
Johnson JO, Mandrioli J, Benatar M, Abramzon Y, Van Deerlin VM, Trojanowski JQ, et al. Exome sequencing reveals VCP mutations as a cause of familial ALS. Neuron. 2010;68(5):857–64.
Deng H-X, Chen W, Hong S-T, Boycott KM, Gorrie GH, Siddique N, et al. Mutations in UBQLN2 cause dominant X-linked juvenile and adult-onset ALS and ALS/dementia. Nature. 2011;477(7363):211–5.
Fecto F, Yan J, Vemula SP, Liu E, Yang Y, Chen W, et al. SQSTM1 mutations in familial and sporadic amyotrophic lateral sclerosis. JAMA Neurol. 2011;68(11):1440–6.
Luty AA, Kwok JB, Dobson-Stone C, Loy CT, Coupland KG, Karlström H, et al. Sigma nonopioid intracellular receptor 1 mutations cause frontotemporal lobar degeneration–motor neuron disease. Ann Neurol. 2010;68(5):639–49.
Al-Saif A, Al-Mohanna F, Bohlega S. A mutation in sigma-1 receptor causes juvenile amyotrophic lateral sclerosis. Ann Neurol. 2011;70(6):913–9.
Williams KL, Topp S, Yang S, Smith B, Fifita JA, Warraich ST, et al. Ccnf mutations in amyotrophic lateral sclerosis and frontotemporal dementia. Nat Commun. 2016;7:11253.
Farhan SM, Howrigan DP, Abbott LE, Klim JR, Topp SD, Byrnes AE, et al. Exome sequencing in amyotrophic lateral sclerosis implicates a novel gene, DNAJC7, encoding a heat-shock protein. Nat Neurosci. 2019;22(12):1966–74.
Figlewicz DA, Krizus A, Martinoli MG, Meininger V, Dib M, Rouleau GA, et al. Variants of the heavy neurofilament subunit are associated with the development of amyotrophic lateral sclerosis. Hum Mol Genet. 1994;3(10):1757–61.
Figlewicz DA, Rouleau GA, Krizus A, Julien J-P. Polymorphism in the multi-phosphorylation domain of the human neurofilament heavy-subunit-encoding gene. Gene. 1993;132(2):297–300.
Puls I, Jonnakuty C, LaMonte BH, Holzbaur ELF, Tokito M, Mann E, et al. Mutant dynactin in motor neuron disease. Nat Genet. 2003;33(4):455–6.
Gros-Louis F, Larivière R, Gowing G, Laurent S, Camu W, Bouchard J-P, et al. A frameshift deletion in peripherin gene associated with amyotrophic lateral sclerosis. J Biol Chem. 2004;279(44):45951–6.
Leung CL, He CZ, Kaufmann P, Chin SS, Naini A, Liem RKH, et al. A pathogenic peripherin gene mutation in a patient with amyotrophic lateral sclerosis. Brain Pathol. 2004;14(3):290–6.
Wu C-H, Fallini C, Ticozzi N, Keagle PJ, Sapp PC, Piotrowska K, et al. Mutations in the profilin 1 gene cause familial amyotrophic lateral sclerosis. Nature. 2012;488(7412):499–503.
Smith BN, Ticozzi N, Fallini C, Gkazi AS, Topp S, Kenna KP, et al. Exome-wide rare variant analysis identifies TUBA4A mutations associated with familial ALS. Neuron. 2014;84(2):324–31.
Nicolas A, Kenna KP, Renton AE, Ticozzi N, Faghri F, Chia R, et al. Genome-wide analyses identify KIF5A as a novel ALS gene. Neuron. 2018;97(6):1268–83. e6.
Brenner D, Yilmaz R, Müller K, Grehl T, Petri S, Meyer T, et al. Hot-spot KIF5A mutations cause familial ALS. Brain. 2018;141(3):688–97.
Zhang S, Cooper-Knock J, Weimer AK, Shi M, Moll T, Marshall JN, et al. Genome-wide identification of the genetic basis of amyotrophic lateral sclerosis. Neuron. 2022;110(6):992–1008. e11.
Van Damme P, Van Hoecke A, Lambrechts D, Vanacker P, Bogaert E, Van Swieten J, et al. Progranulin functions as a neurotrophic factor to regulate neurite outgrowth and enhance neuronal survival. J Cell Biol. 2008;181(1):37–41.
Cooper-Knock J, Moll T, Ramesh T, Castelli L, Beer A, Robins H, et al. Mutations in the glycosyltransferase domain of GLT8D1 are associated with familial amyotrophic lateral sclerosis. Cell Rep. 2019;26(9):2298–306. e5.
Cooper-Knock J, Zhang S, Kenna KP, Moll T, Franklin JP, Allen S, et al. Rare variant burden analysis within enhancers identifies CAV1 as an ALS risk gene. Cell Rep. 2020;33(9):108456.
Adey BN, Cooper-Knock J, Al Khleifat A, Fogh I, van Damme P, Corcia P, et al. Large-scale analyses of CAV1 and CAV2 suggest their expression is higher in post-mortem ALS brain tissue and affects survival. Front Cell Neurosci. 2023;17:1112405.
Li W, Liu Z, Sun W, Yuan Y, Hu Y, Ni J, et al. Mutation analysis of GLT8D1 and ARPP21 genes in amyotrophic lateral sclerosis patients from mainland China. Neurobiol Aging. 2020;85:156. e1-. e4.
Dols-Icardo O, Carbayo Á, Jericó I, Blasco-Martínez O, Álvarez-Sánchez E, Pérez MAL, Bernal S, Rodríguez-Santiago B, Cusco I, Turon-Sans J, Cabezas-Torres M. Identification of a pathogenic mutation in ARPP21 in patients with amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry. 2024;96(2):132–139. https://doi.org/10.1136/jnnp-2024-333834.
Mackenzie IR, Nicholson AM, Sarkar M, Messing J, Purice MD, Pottier C, et al. TIA1 mutations in amyotrophic lateral sclerosis and frontotemporal dementia promote phase separation and alter stress granule dynamics. Neuron. 2017;95(4):808–16. e9.
Iacoangeli A, Lin T, Al Khleifat A, Jones AR, Opie-Martin S, Coleman JR, et al. Genome-wide meta-analysis finds the ACSL5-ZDHHC6 locus is associated with ALS and links weight loss to the disease genetics. Cell Rep. 2020;33(4):108323.
Nakamura R, Misawa K, Tohnai G, Nakatochi M, Furuhashi S, Atsuta N, et al. A multi-ethnic meta-analysis identifies novel genes, including ACSL5, associated with amyotrophic lateral sclerosis. Commun Biol. 2020;3(1):526.
Johnson JO, Chia R, Miller DE, Li R, Kumaran R, Abramzon Y, et al. Association of variants in the SPTLC1 gene with juvenile amyotrophic lateral sclerosis. JAMA Neurol. 2021;78(10):1236–48.
Mohassel P, Donkervoort S, Lone MA, Nalls M, Gable K, Gupta SD, et al. Childhood amyotrophic lateral sclerosis caused by excess sphingolipid synthesis. Nat Med. 2021;27(7):1197–204.
Naruse H, Ishiura H, Esaki K, Mitsui J, Satake W, Greimel P, et al. Variants are associated with early-onset ALS and FTD due to aberrant sphingolipid synthesis. Ann Clin Transl Neurol. 2024;11(4):946–57.
Al Khleifat A, Iacoangeli A, Van Vugt JJfa, Bowles H, Zwamborn RAJ, Moisse M, et al. Structural variation analysis of 6,500 whole genome sequences in amyotrophic lateral sclerosis. NPJ Genomic Med. 2021;7(1):8.
Takahashi Y, Fukuda Y, Yoshimura J, Toyoda A, Kurppa K, Moritoyo H, et al. <ERBB4> mutations that disrupt the neuregulin-ErbB4 pathway cause amyotrophic lateral sclerosis type 19. Am J Hum Genet. 2013;93(5):900–5.
Tunca C, Akçimen F, Coşkun C, Gündoğdu-Eken A, Kocoglu C, Çevik B, et al. ERLIN1 mutations cause teenage-onset slowly progressive ALS in a large Turkish pedigree. Eur J Hum Genet. 2018;26(5):745–8.
Dobson-Stone C, Hallupp M, Shahheydari H, Ragagnin AMG, Chatterton Z, Carew-Jones F, et al. CYLD is a causative gene for frontotemporal dementia – amyotrophic lateral sclerosis. Brain. 2020;143(3):783–99.
Chesi A, Staahl BT, Jovičić A, Couthouis J, Fasolino M, Raphael AR, et al. Exome sequencing to identify de novo mutations in sporadic ALS trios. Nat Neurosci. 2013;16(7):851–5.
Gelfman S, Dugger S, Moreno CDAM, Ren Z, Wolock CJ, Shneider NA, et al. A new approach for rare variation collapsing on functional protein domains implicates specific genic regions in ALS. Genome Res. 2019;29(5):809–18.
Shepheard SR, Parker MD, Cooper-Knock J, Verber NS, Tuddenham L, Heath P, et al. Value of systematic genetic screening of patients with amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry. 2021;92(5):510–8.
Clinical Genome Resource. Amyotrophic Lateral Sclerosis Spectrum Disorders Gene Curation Expert Panel 2024 [Available from: https://clinicalgenome.org/affiliation/40096/.
Glass JD, Dewan R, Ding J, Gibbs JR, Dalgard C, Keagle PJ, et al. ATXN2 intermediate expansions in amyotrophic lateral sclerosis. Brain. 2022;145(8):2671–6.
Tazelaar GHP, Boeynaems S, De Decker M, van Vugt J, Kool L, Goedee HS, et al. ATXN1 repeat expansions confer risk for amyotrophic lateral sclerosis and contribute to TDP-43 mislocalization. Brain Commun. 2020;2(2):fcaa064.
Tazelaar GHP, Dekker AM, van Vugt J, van der Spek RA, Westeneng HJ, Kool L, et al. Association of NIPA1 repeat expansions with amyotrophic lateral sclerosis in a large international cohort. Neurobiol Aging. 2019;74:234.e9-.e15.
Dewan R, Chia R, Ding J, Hickman RA, Stein TD, Abramzon Y, et al. Pathogenic huntingtin repeat expansions in patients with frontotemporal dementia and amyotrophic lateral sclerosis. Neuron. 2021;109(3):448-60.e4.
Wieder N, D’Souza EN, Martin-Geary AC, Lassen FH, Talbot-Martin J, Fernandes M, et al. Differences in 5’untranslated regions highlight the importance of translational regulation of dosage sensitive genes. Genome Biol. 2024;25(1):111.
Marriott H, Spargo TP, Al Khleifat A, Andersen PM, Başak NA, Cooper-Knock J, et al. Mutations in the tail and rod domains of the neurofilament heavy-chain gene increase the risk of ALS. Ann Clin Transl Neurol. 2024;11(7):1775–86.
Theunissen F, Anderton RS, Mastaglia FL, James I, Bedlack R, Akkari PA. Intronic NEFH variant is associated with reduced risk for sporadic ALS and later age of disease onset. Sci Rep. 2022;12(1):14739.
Grassano M, Calvo A, Moglia C, Brunetti M, Barberis M, Sbaiz L, et al. Mutational analysis of known ALS genes in an Italian population-based cohort. Neurology. 2021;96(4):e600-9.
Valdmanis PN, Belzil VV, Lee J, Dion PA, St-Onge J, Hince P, et al. A mutation that creates a pseudoexon in SOD1 causes familial ALS. Ann Hum Genet. 2009;73(Pt 6):652–7.
Birve A, Neuwirth C, Weber M, Marklund SL, Nilsson AC, Jonsson PA, et al. A novel SOD1 splice site mutation associated with familial ALS revealed by SOD activity analysis. Hum Mol Genet. 2010;19(21):4201–6.
Nakano J, Chiba K, Niwa S. An ALS-associated KIF5A mutant forms oligomers and aggregates and induces neuronal toxicity. Genes Cells. 2022;27(6):421–35.
Ling JP, Pletnikova O, Troncoso JC, Wong PC. TDP-43 repression of nonconserved cryptic exons is compromised in ALS-FTD. Science. 2015;349(6248):650–5.
Klim JR, Williams LA, Limone F, San Juan IG, Davis-Dusenbery BN, Mordes DA, et al. ALS-implicated protein TDP-43 sustains levels of STMN2, a mediator of motor neuron growth and repair. Nat Neurosci. 2019;22(2):167–79.
Melamed Ze, Lopez-Erauskin J, Baughn MW, Zhang O, Drenner K, Sun Y, et al. Premature polyadenylation-mediated loss of stathmin-2 is a hallmark of TDP-43-dependent neurodegeneration. Nat Neurosci. 2019;22(2):180.
Ma XR, Prudencio M, Koike Y, Vatsavayai SC, Kim G, Harbinski F, et al. TDP-43 represses cryptic exon inclusion in the FTD–ALS gene UNC13A. Nature. 2022;603(7899):124–30.
Van Es MA, Veldink JH, Saris CG, Blauw HM, van Vught PW, Birve A, et al. Genome-wide association study identifies 19p13. 3 (UNC13A) and 9p21. 2 as susceptibility loci for sporadic amyotrophic lateral sclerosis. Nat Genet. 2009;41(10):1083.
Diekstra FP, Van Deerlin VM, van Swieten JC, Al-Chalabi A, Ludolph AC, Weishaupt JH, et al. C9orf72 and UNC13A are shared risk loci for amyotrophic lateral sclerosis and frontotemporal dementia: a genome-wide meta-analysis. Ann Neurol. 2014;76(1):120–33.
van Rheenen W, van der Spek R, Bakker M, van den Berg L, Veldink J, van Vugt J, et al. Common and rare variant association analyses in Amyotrophic Lateral Sclerosis identify 15 risk loci with distinct genetic architectures and neuron-specific biology. Nat Genet. 2021;53(12):1636–48.
Diekstra FP, van Vught PWJ, van Rheenen W, Koppers M, Pasterkamp RJ, van Es MA, et al. UNC13A is a modifier of survival in amyotrophic lateral sclerosis. Neurobiol Aging. 2012;33(3):630.e3-.e8.
Yang B, Jiang H, Wang F, Li S, Wu C, Bao J, et al. UNC13A variant rs12608932 is associated with increased risk of amyotrophic lateral sclerosis and reduced patient survival: a meta-analysis. Neurol Sci. 2019;40(11):2293–302.
Brown A-L, Wilkins OG, Keuss MJ, Hill SE, Zanovello M, Lee WC, et al. TDP-43 loss and ALS-risk SNPs drive mis-splicing and depletion of UNC13A. Nature. 2022;603(7899):131–7.
Müller K, Oh K-W, Nordin A, Panthi S, Kim SH, Nordin F, et al. De novo mutations in SOD1 are a cause of ALS. J Neurol Neurosurg Psychiatry. 2022;93(2):201–6.
Chiò A, Calvo A, Moglia C, Ossola I, Brunetti M, Sbaiz L, et al. A de novo missense mutation of the FUS gene in a “true” sporadic ALS case. Neurobiol Aging. 2011;32(3):553. e23-. e26.
Abramzon Y, Johnson JO, Scholz SW, Taylor JP, Brunetti M, Calvo A, et al. Valosin-containing protein (VCP) mutations in sporadic amyotrophic lateral sclerosis. Neurobiol Aging. 2012;33(9):2231.e1-.e6.
Al-Chalabi A, Hardiman O. The epidemiology of ALS: a conspiracy of genes, environment and time. Nat Rev Neurol. 2013;9(11):617.
Chiò A, Mazzini L, D’Alfonso S, Corrado L, Canosa A, Moglia C, et al. The multistep hypothesis of ALS revisited: the role of genetic mutations. Neurology. 2018;91(7):e635–42.
Vucic S, Higashihara M, Sobue G, Atsuta N, Doi Y, Kuwabara S, et al. ALS is a multistep process in South Korean, Japanese, and Australian patients. Neurology. 2020;94(15):e1657-e63.
Garton FC, Trabjerg BB, Wray NR, Agerbo E. Cardiovascular disease, psychiatric diagnosis and sex differences in the multistep hypothesis of amyotrophic lateral sclerosis. Eur J Neurol. 2021;28(2):421–9.
Chiò A, Logroscino G, Traynor B, Collins J, Simeone J, Goldstein L, et al. Global epidemiology of amyotrophic lateral sclerosis: a systematic review of the published literature. Neuroepidemiology. 2013;41(2):118–30.
Cronin S, Hardiman O, Traynor BJ. Ethnic variation in the incidence of ALS: a systematic review. Neurology. 2007;68(13):1002–7.
Goutman SA, Savelieff MG, Jang D-G, Hur J, Feldman EL. The amyotrophic lateral sclerosis exposome: recent advances and future directions. Nat Rev Neurol. 2023;19(10):617–34.
Zou Z-Y, Zhou Z-R, Che C-H, Liu C-Y, He R-L, Huang H-P. Genetic epidemiology of amyotrophic lateral sclerosis: a systematic review and meta-analysis. J Neurol Neurosurg Psychiatry. 2017;88(7):540–9.
Olsen CG, Busk ØL, Aanjesen TN, Alstadhaug KB, Bjørnå IK, Braathen GJ, et al. Genetic epidemiology of amyotrophic lateral sclerosis in Norway: a 2-year population-based study. Neuroepidemiology. 2022;56(4):271–82.
Alavi A, Nafissi S, Rohani M, Shahidi G, Zamani B, Shamshiri H, et al. Repeat expansion in C9ORF72 is not a major cause of amyotrophic lateral sclerosis among Iranian patients. Neurobiol Aging. 2014;35(1):267. e1-. e7.
McCann E, Williams K, Fifita J, Tarr I, O’connor J, Rowe D, et al. The genotype–phenotype landscape of familial amyotrophic lateral sclerosis in Australia. Clin Genet. 2017;92(3):259–66.
McCann EP, Henden L, Fifita JA, Zhang KY, Grima N, Bauer DC, et al. Evidence for polygenic and oligogenic basis of Australian sporadic amyotrophic lateral sclerosis. J Med Genet. 2021;58(2):87–95.
Liu ZJ, Lin HX, Wei Q, Zhang QJ, Chen CX, Tao QQ, et al. Genetic spectrum and variability in Chinese patients with amyotrophic lateral sclerosis. Aging Dis. 2019;10(6):1199–206.
Zou ZY, Liu MS, Li XG, Cui LY. The distinctive genetic architecture of ALS in mainland China. J Neurol Neurosurg Psychiatry. 2016;87(8):906–7.
Naruse H, Ishiura H, Mitsui J, Takahashi Y, Matsukawa T, Tanaka M, et al. Burden of rare variants in causative genes for amyotrophic lateral sclerosis (ALS) accelerates age at onset of ALS. J Neurol Neurosurg Psychiatry. 2019;90(5):537–42.
Nishiyama A, Niihori T, Warita H, Izumi R, Akiyama T, Kato M, et al. Comprehensive targeted next-generation sequencing in Japanese familial amyotrophic lateral sclerosis. Neurobiol Aging. 2017;53:194.e1-.e8.
Narain P, Pandey A, Gupta S, Gomes J, Bhatia R, Vivekanandan P. Targeted next-generation sequencing reveals novel and rare variants in Indian patients with amyotrophic lateral sclerosis. Neurobiol Aging. 2018;71:265.e9-e14.
Soong B-W, Lin K-P, Guo Y-C, Lin C-CK, Tsai P-C, Liao Y-C, et al. Extensive molecular genetic survey of Taiwanese patients with amyotrophic lateral sclerosis. Neurobiology of Aging. 2014;35(10):2423.e1-.e6.
Sung W, Kim J-A, Kim YS, Park J, Oh K-W, Sung J-J, et al. An analysis of variants in TARDBP in the Korean population with amyotrophic lateral sclerosis: comparison with previous data. Sci Rep. 2023;13(1):18805.
Salmon K, Kiernan MC, Kim SH, Andersen PM, Chio A, van den Berg LH, et al. The importance of offering early genetic testing in everyone with amyotrophic lateral sclerosis. Brain. 2022;145(4):1207–10.
Dilliott AA, Al Nasser A, Elnagheeb M, Fifita J, Henden L, Keseler IM, et al. Clinical testing panels for ALS: global distribution, consistency, and challenges. Amyotroph Lateral Scler Frontotemporal Degener. 2023;24(5–6):420–35.
Goutman SA. Diagnosis and clinical management of amyotrophic lateral sclerosis and other motor neuron disorders. CONTINUUM: Lifelong Learn Neurol. 2017;23(5):1332–59.
Moss DH, Poulter M, Beck J, Polke J, Campbell T, Adamson G, et al. K11 C9orf72 expansions are the Most common genetic cause of Huntington’s disease Phenocopy presentations in a UK cohort. Neurology. 2014;82(4):292–9.
Cooper-Knock J, Frolov A, Highley JR, Charlesworth G, Kirby J, Milano A, et al. C9ORF72 expansions, parkinsonism, and Parkinson disease: a clinicopathologic study. Neurology. 2013;81(9):808–11.
Estevez-Fraga C, Magrinelli F, Hensman Moss D, Mulroy E, Di Lazzaro G, Latorre A, et al. Expanding the spectrum of movement disorders associated with C9orf72 hexanucleotide expansions. Neurol Genet. 2021;7(2):e575.
Myers RH. Huntington’s disease genetics. Neurotherapeutics. 2004;1:255–62.
Nicolas A, Kenna KP, Renton AE, Ticozzi N, Faghri F, Chia R, et al. Genome-wide Analyses Identify KIF5A as a Novel ALS Gene. Neuron. 2018;97(6):1268-83.e6.
Crimella C, Baschirotto C, Arnoldi A, Tonelli A, Tenderini E, Airoldi G, et al. Mutations in the motor and stalk domains of KIF5A in spastic paraplegia type 10 and in axonal Charcot–Marie–Tooth type 2. Clin Genet. 2012;82(2):157–64.
Reid E, Kloos M, Ashley-Koch A, Hughes L, Bevan S, Svenson IK, et al. A kinesin heavy chain (KIF5A) mutation in hereditary spastic paraplegia (SPG10). Am J Hum Genet. 2002;71(5):1189–94.
Bejaoui K, Wu C, Scheffler MD, Haan G, Ashby P, Wu L, et al. Sptlc1 is mutated in hereditary sensory neuropathy, type 1. Nat Genet. 2001;27(3):261–2.
Course MM, Gudsnuk K, Smukowski SN, Winston K, Desai N, Ross JP, et al. Evolution of a human-specific tandem repeat associated with ALS. Am J Hum Genet. 2020;107(3):445–60.
PacBio. PureTarget. https://www.pacb.com/technology/puretarget/2024. Available from: https://www.pacb.com/technology/puretarget/.
Salmon K, Ross JP, Bertone V, Gobbo M, Anoja N, Karamchandani J, et al. The value of testing for ATXN2 intermediate repeat expansions in routine clinical practice for amyotrophic lateral sclerosis. Eur J Hum Genet. 2022;30(11):1205–7.
Foox J, Tighe SW, Nicolet CM, Zook JM, Byrska-Bishop M, Clarke WE, et al. Performance assessment of DNA sequencing platforms in the ABRF next-generation sequencing study. Nat Biotechnol. 2021;39(9):1129–40.
Olson ND, Wagner J, McDaniel J, Stephens SH, Westreich ST, Prasanna AG, et al. PrecisionFDA truth challenge v2: calling variants from short and long reads in difficult-to-map regions. Cell Genom. 2022;2(5):100129.
Jarvis ED, Formenti G, Rhie A, Guarracino A, Yang C, Wood J, et al. Semi-automated assembly of high-quality diploid human reference genomes. Nature. 2022;611(7936):519–31.
Marx V. Method of the year: long-read sequencing. Nat Methods. 2023;20(1):6–11.
Conesa A, Hoischen A, Sedlazeck FJ. Revolutionizing genomics and medicine—one long molecule at a time. Genome Res. 2024;34(11):ix–xi.
Logsdon GA, Vollger MR, Eichler EE. Long-read human genome sequencing and its applications. Nat Rev Genet. 2020;21(10):597–614.
Mahmoud M, Huang Y, Garimella K, Audano PA, Wan W, Prasad N, et al. Utility of long-read sequencing for all of us. Nat Commun. 2024;15(1):837.
Harvey WT, Ebert P, Ebler J, Audano PA, Munson KM, Hoekzema K, et al. Whole-genome long-read sequencing downsampling and its effect on variant-calling precision and recall. Genome Res. 2023;33(12):2029–40.
Sarashetti P, Lipovac J, Tomas F, Šikic M, Liu J. The hitchhiker’s guide to sequencing data types and volumes for population-scale pangenome construction. Preprint at bioRxiv. 2024.
Abdelwahab O, Belzile F, Torkamaneh D. Performance analysis of conventional and AI-based variant callers using short and long reads. BMC Bioinformatics. 2023;24(1):472.
Kolesnikov A, Cook D, Nattestad M, Brambrink L, McNulty B, Gorzynski J, et al. Local read haplotagging enables accurate long-read small variant calling. Nat Commun. 2024;15(1):5907.
Nurk S, Koren S, Rhie A, Rautiainen M, Bzikadze AV, Mikheenko A, et al. The complete sequence of a human genome. Science. 2022;376(6588):44–53.
Liao W-W, Asri M, Ebler J, Doerr D, Haukness M, Hickey G, et al. A draft human pangenome reference. Nature. 2023;617(7960):312–24.
Gao Y, Yang X, Chen H, Tan X, Yang Z, Deng L, et al. A pangenome reference of 36 Chinese populations. Nature. 2023;619(7968):112–21.
Littlefield C, Lazaro-Guevara JM, Stucki D, Lansford M, Pezzolesi MH, Taylor EJ, et al. A draft pacific ancestry pangenome reference. Preprint at bioRxiv. 2024.
Nassir N, Almarri MA, Kumail M, Mohamed N, Balan B, Hanif S, et al. A draft UAE-based Arab pangenome reference. Nat Commun. 2025;16(1):6747.
Porubsky D, Vollger MR, Harvey WT, Rozanski AN, Ebert P, Hickey G, et al. Gaps and complex structurally variant loci in phased genome assemblies. Genome Res. 2023;33(4):496–510.
Vollger MR, Dishuck PC, Harvey WT, DeWitt WS, Guitart X, Goldberg ME, et al. Increased mutation and gene conversion within human segmental duplications. Nature. 2023;617(7960):325–34.
Dolzhenko E, English A, Dashnow H, De Sena Brandine G, Mokveld T, Rowell WJ, et al. Characterization and visualization of tandem repeats at genome scale. Nat Biotechnol. 2024;42(10):1606–14.
Weisburd B, Dolzhenko E, Bennett MF, Danzi MC, English A, Hiatt L, et al. Defining a tandem repeat catalog and variation clusters for genome-wide analyses and population databases. Preprint at bioRxiv. 2024.
Cheung WA, Johnson AF, Rowell WJ, Farrow E, Hall R, Cohen ASA, et al. Direct haplotype-resolved 5-base HiFi sequencing for genome-wide profiling of hypermethylation outliers in a rare disease cohort. Nat Commun. 2023;14(1):3090.
Pagni S, Mills JD, Frankish A, Mudge JM, Sisodiya SM. Non-coding regulatory elements: potential roles in disease and the case of epilepsy. Neuropathol Appl Neurobiol. 2022;48(3):e12775.
Cohen ASA, Farrow EG, Abdelmoity AT, Alaimo JT, Amudhavalli SM, Anderson JT, et al. Genomic answers for children: Dynamic analyses of 1000 pediatric rare disease genomes. Genet Med. 2022;24(6):1336–48.
Hiatt SM, Lawlor JMJ, Handley LH, Latner DR, Bonnstetter ZT, Finnila CR, et al. Long-read genome sequencing and variant reanalysis increase diagnostic yield in neurodevelopmental disorders. Genome Res. 2024;34(11):1747–62.
Steyaert W, Sagath L, Demidov G, Yépez VA, Esteve-Codina A, Gagneur J, et al. Unravelling undiagnosed rare disease cases by HiFi long-read genome sequencing. Preprint at medRxiv. 2024.
Estonia National Biobank. Estonia National Biobank selects PacBio to sequence 10,000 whole genomes 2024. Available from: https://www.prnewswire.com/news-releases/estonia-national-biobank-selects-pacbio-to-sequence-10-000-whole-genomes-302100822.html.
Eisfeldt J, Ameur A, Lenner F, Ten Berk Boer E, Ek M, Wincent J, et al. A national long-read sequencing study on chromosomal rearrangements uncovers hidden complexities. Genome Res. 2024;34(11):1774–84.
Handsaker RE, Kashin S, Reed NM, Tan S, Lee W-S, McDonald TM, et al. Long somatic DNA-repeat expansion drives neurodegeneration in Huntingtons disease. Cell. 2025;188(3):623-39.e19.
Evans JR, Gustavsson EK, Doykov I, Murphy D, Virdi GS, Lachica J, et al. The diversity of SNCA transcripts in neurons, and its impact on antisense oligonucleotide therapeutics. Preprint at bioRxiv. 2024.
Pachchek S, Landoulsi Z, Pavelka L, Schulte C, Buena-Atienza E, Gross C, et al. Accurate long-read sequencing identified GBA1 as major risk factor in the Luxembourgish Parkinson’s study. NPJ Parkinsons Dis. 2023;9(1):156.
Song JHT, Lowe CB, Kingsley DM. Characterization of a human-specific tandem repeat associated with bipolar disorder and schizophrenia. Am J Hum Genet. 2018;103(3):421–30.
Zhang H-Y, Minnis C, Gustavsson E, Ryten M, Mole SE. CLN3 transcript complexity revealed by long-read RNA sequencing analysis. BMC Med Genomics. 2024;17(1):244.
Udine E, Jain A, van Blitterswijk M. Advances in sequencing technologies for amyotrophic lateral sclerosis research. Mol Neurodegener. 2023;18(1):4.
Ebbert MTW, Farrugia SL, Sens JP, Jansen-West K, Gendron TF, Prudencio M, et al. Long-read sequencing across the C9orf72 ‘GGGGCC’ repeat expansion: implications for clinical use and genetic discovery efforts in human disease. Mol Neurodegener. 2018;13(1):46.
Tsai Y-C, Brown KA, Bernardi MT, Harting J, Clelland CD. Single-molecule sequencing of the C9orf72 repeat expansion in patient iPSCs. Bio-Protoc. 2024;14(17):e5060.
DeJesus-Hernandez M, Aleff RA, Jackson JL, Finch NA, Baker MC, Gendron TF, et al. Long-read targeted sequencing uncovers clinicopathological associations for C9orf72-linked diseases. Brain. 2021;144(4):1082–8.
Salomonsson SE, Maltos AM, Gill K, Aladesuyi Arogundade O, Brown KA, Sachdev A, et al. Validated assays for the quantification of C9orf72 human pathology. Sci Rep. 2024;14(1):828.
Sachdev A, Gill K, Sckaff M, Birk AM, Aladesuyi Arogundade O, Brown KA, et al. Reversal of C9orf72 mutation-induced transcriptional dysregulation and pathology in cultured human neurons by allele-specific excision. Proc Natl Acad Sci U S A. 2024;121(17):e2307814121.
Masala A, Sanna S, Esposito S, Rassu M, Galioto M, Zinellu A, et al. Epigenetic changes associated with the expression of amyotrophic lateral sclerosis (ALS) causing genes. Neuroscience. 2018;390:1–11.
Grant OA, Iacoangeli A, Zwamborn RAJ, van Rheenen W, Byrne R, Van Eijk KR, et al. Sex-specific DNA methylation differences in Amyotrophic lateral sclerosis. Preprint at bioRxiv. 2024:2024.11.22.624866.
Kitsou K, Katzourakis A, Magiorkinis G. Limitations of current high-throughput sequencing technologies lead to biased expression estimates of endogenous retroviral elements. NAR Genomics Bioinform. 2024;6(3):lqae081.
Brinzevich D, Young GR, Sebra R, Ayllon J, Maio SM, Deikus G, et al. HIV-1 interacts with human endogenous retrovirus K (HML-2) envelopes derived from human primary lymphocytes. J Virol. 2014;88(11):6213–23.
Li W, Pandya D, Pasternack N, Garcia-Montojo M, Henderson L, Kozak CA, et al. Retroviral elements in pathophysiology and as therapeutic targets for amyotrophic lateral sclerosis. Neurotherapeutics. 2022;19(4):1085–101.
Yang X, Coulombe-Huntington J, Kang S, Sheynkman Gloria M, Hao T, Richardson A, et al. Widespread expansion of protein interaction capabilities by alternative splicing. Cell. 2016;164(4):805–17.
Stevens M, Oltean S. Modulation of the apoptosis gene Bcl-x function through alternative splicing. Front Genet. 2019. https://doi.org/10.3389/fgene.2019.00804.
Abood A, Mesner LD, Jeffery ED, Murali M, Lehe MD, Saquing J, et al. Long-read proteogenomics to connect disease-associated sQTLs to the protein isoform effectors of disease. Am J Hum Genet. 2024;111(9):1914–31.
Oehler D, Spychala A, Gödecke A, Lang A, Gerdes N, Ruas J, et al. Full-length transcriptomic analysis in murine and human heart reveals diversity of PGC-1α promoters and isoforms regulated distinctly in myocardial ischemia and obesity. BMC Biol. 2022;20(1):169.
Reese F, Williams B, Balderrama-Gutierrez G, Wyman D, Çelik MH, Rebboah E, et al. The ENCODE4 long-read RNA-seq collection reveals distinct classes of transcript structure diversity. Preprint at bioRxiv. 2023.
Pardo-Palacios FJ, Wang D, Reese F, Diekhans M, Carbonell-Sala S, Williams B, et al. Systematic assessment of long-read RNA-seq methods for transcript identification and quantification. Nat Methods. 2024;21(7):1349–63.
Torre D, Francoeur NJ, Kalma Y, Gross Carmel I, Melo BS, Deikus G, et al. Isoform-resolved transcriptome of the human preimplantation embryo. Nat Commun. 2023;14(1):6902.
Gallo CM, Kistler S, Natrakul A, Labadorf AT, Beffert U, Ho A. Heterogeneity of novel APOER2 isoforms specific to Alzheimer’s disease impact cellular and synaptic states. Preprint at bioRxiv. 2023.
Manek R, Nelson T, Tseng E, Rodriguez-Lebron E. 5′UTR-mediated regulation of Ataxin-1 expression. Neurobiol Dis. 2020;134:104564.
Tseng E, Rowell WJ, Glenn OC, Hon T, Barrera J, Kujawa S, et al. The landscape of SNCA transcripts across synucleinopathies: new insights from long reads sequencing analysis. Front Genet. 2019;10:584.
Vollger MR, Korlach J, Eldred KC, Swanson E, Underwood JG, Bohaczuk SC, et al. Synchronized long-read genome, methylome, epigenome and transcriptome profiling resolve a Mendelian condition. Nat Genet. 2025;57(2):469–79.
Spargo TP, Marriott H, Hunt GP, Pain O, Kabiljo R, Bowles H, et al. Unsupervised machine-learning identifies clinically distinct subtypes of ALS that reflect different genetic architectures and biological mechanisms. Preprint at medRxiv. 2023.
Eshima J, O’Connor SA, Marschall E, Bowser R, Plaisier CL, Smith BS. Molecular subtypes of ALS are associated with differences in patient prognosis. Nat Commun. 2023;14(1):95.
Tam OH, Rozhkov NV, Shaw R, Kim D, Hubbard I, Fennessey S, et al. Postmortem cortex samples identify distinct molecular subtypes of ALS: retrotransposon activation, oxidative stress, and activated glia. Cell Rep. 2019;29(5):1164-77.e5.
Ravnik-Glavač M, Goričar K, Vogrinc D, Koritnik B, Lavrenčič JG, Glavač D, et al. Genetic variability of inflammation and oxidative stress genes affects onset, progression of the disease and survival of patients with amyotrophic lateral sclerosis. Genes. 2022;13(5):757.
Caldi Gomes L, Hänzelmann S, Hausmann F, Khatri R, Oller S, Parvaz M, et al. Multiomic ALS signatures highlight subclusters and sex differences suggesting the MAPK pathway as therapeutic target. Nat Commun. 2024;15(1):4893.
Marriott H, Kabiljo R, Hunt GP, Khleifat AA, Jones A, Troakes C, et al. Unsupervised machine learning identifies distinct ALS molecular subtypes in post-mortem motor cortex and blood expression data. Acta Neuropathol Commun. 2023;11(1):208.
Aronica E, Baas F, Iyer A, ten Asbroek AL, Morello G, Cavallaro S. Molecular classification of amyotrophic lateral sclerosis by unsupervised clustering of gene expression in motor cortex. Neurobiol Dis. 2015;74:359–76.
La Cognata V, Gentile G, Aronica E, Cavallaro S. Splicing players are differently expressed in sporadic amyotrophic lateral sclerosis molecular clusters and brain regions. Cells. 2020;9(1):159.
Morello G, Spampinato AG, Cavallaro S. Molecular taxonomy of sporadic amyotrophic lateral sclerosis using disease-associated genes. Front Neurol. 2017;8:152.
Kumbier K, Roth M, Li Z, Lazzari-Dean J, Waters C, Hammerlindl S, et al. Identifying FUS amyotrophic lateral sclerosis disease signatures in patient dermal fibroblasts. Dev Cell. 2024;59(16):2134-42.e6.
GenieUs Genomics. DiGAP 2023. Available from: https://www.genieus.co/digap.
Giordano J, Shook JR. Minding brain science in medicine: on the need for neuroethical engagement for guidance of neuroscience in clinical contexts. Ethic Biol Eng Med. 2015. https://doi.org/10.1615/EthicsBiologyEngMed.2015015333.
Giordano J, Hutchison PJ, Benedikter RA. Culture, sustainability, and medicine in the twenty-first century. Re-grounding the focus of medicine amidst the current “global systemic shift” and the forces of the market: elements for a contemporary social philosophy of medicine. Int J Polit Cult Soc. 2010;23:29–41.
Giordano J. Quo vadis? Philosophy, Ethics, and Humanities in Medicine-preserving the humanistic character of medicine in a biotechnological future. Springer; 2009;4(1):12.
Giordano J. Conditions for consent to the use of neurotechnology: a preparatory neuroethical approach to risk assessment and reduction. AJOB Neurosci. 2015;6(4):12–4.
Desai P, Shook JR, Giordano J. Addressing and managing systemic benefit, burden and risk of emerging neurotechnology. AJOB Neurosci. 2022;13(1):68–70.
Shook JR, Giordano J. Designing new neurorights: tasking and translating them to all humanity. AJOB Neurosci. 2023;14(4):372–4.
DeFranco J, Rhemann M, Giordano J. The emerging neurobioeconomy: implications for national security. Health Secur. 2020;18(4):267–77.