When Giles Turner, a 65-year-old retired banker from Sussex, was diagnosed with advanced prostate cancer, he did his research and learned that his best chance was with a drug called abiraterone.
Although his cancer was still localised – it hadn’t spread beyond the prostate – it was a high-risk and aggressive form, which abiraterone has been shown to be very effective in halting.
But while the drug is available on the NHS to men in Scotland and Wales at the same stage of the disease, Giles was stunned when his consultant explained that NHS England would not provide it.
And campaigners and experts say that this failure to provide abiraterone to earlier – but still advanced – stage cancers stems from flawed bureaucratic procedures.
The drug is currently approved on the NHS for stage 4 prostate cancer.
The charity Prostate Cancer UK, which is among those calling for abiraterone to be made available to the men with earlier, stage 3 aggressive prostate cancers, warns that NHS England’s delay in approving the drug has already cost more than 1,300 lives since 2023 – and estimates that 13 more men will die each week until NHS England changes course.
‘A blockage is costing hundreds of lives every year – this situation cannot continue,’ Amy Rylance, the charity’s assistant director of health improvement, told Good Health.
Prostate cancer is fuelled by male hormones. Abiraterone is highly effective because it is the only drug that blocks the production of male hormones not just in the testicles, but also in the adrenal glands and within the tumour itself.
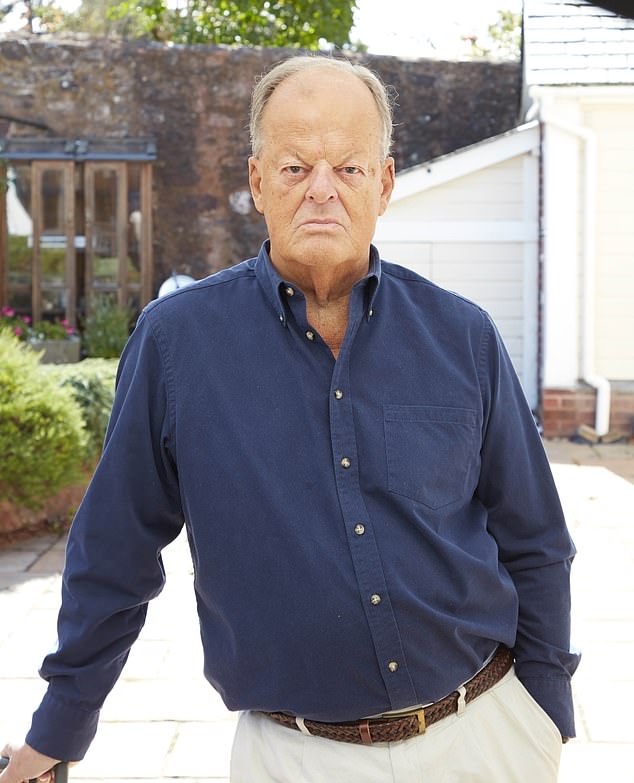
When Giles Turner was diagnosed with advanced prostate cancer, his own research showed that a drug called abiraterone would be the best treatment for his condition, but he was left stunned when his consultant explained that NHS England would not provide it
Despite strong evidence of its benefits when used to treat stage 3 aggressive cancer, NHS England has not yet approved funding for these earlier cases.
This is not a cost issue, as the drug came ‘off patent’ in 2022 and is now classed as generic. However, this means there is no company to sponsor an appraisal with the NHS’s medicines watchdog NICE (the National Institute for Health and Care Excellence).
Funding for the appraisal therefore sits with NHS England’s clinical priorities process, which has yet to allocate a sustainable budget for it.
As a result, despite now being a low-cost medication, patients in England with cancers that have not yet spread (non-metastatic cancers) must pay privately.
Following his diagnosis in March 2023, Giles has spent around £20,000 on abiraterone, plus blood tests and monitoring, to improve his odds of surviving.
He started the tablets in July that year, alongside standard hormone therapy and radiotherapy. By May 2025, an MRI showed no sign of cancer, placing him in remission.
Prostate cancer, the UK’s most common male cancer, can range from slow-growing forms that never cause serious harm to aggressive types that spread rapidly.
Giles’s doctors described his case as ‘high-risk, locally advanced’ – meaning the cancer was still contained in and around the prostate, but was highly likely to spread elsewhere in the body.
This puts men like Giles in a particularly perilous position: their disease is not yet incurable, but, without the most effective treatments, the risk of relapse or progression is high, says Professor Nick James, a clinical oncologist at The Royal Marsden Hospital in London.

Amy Rylance, assistant director of health improvement of Prostate Cancer UK, says: ‘this situation cannot continue’
Adding two years of abiraterone to standard cancer therapy for these men with high-risk cancer that hasn’t yet spread could lead to ‘just over a 40 per cent reduction in the risk of death from prostate cancer’, he explains.
This is because, while standard hormone therapy lowers testosterone from the main source – the testicles – the cancer can still feed on the small amounts made by the adrenal glands or even by the tumour itself. Abiraterone blocks the enzyme that drives those ‘back-up’ supplies.
(The drug has not been shown to help men with low-risk stage 1 or 2 prostate cancer, and as it can have significant side-effects – such as high blood pressure – and patients also need to take daily steroids, the risks aren’t justified for low-risk cases usually cured with surgery or radiotherapy alone.)
Tony Collier, 68, from Cheshire knows just how effective the drug can be. Tony, a former chartered accountant, is a keen runner and when an injury led to scans he received a shock diagnosis of stage 4 prostate cancer in 2017.
He was treated with abiraterone, and despite the cancer having already spread to his bones, he went into remission. Eight years on, he’s still running and believes he is living proof that timely use of abiraterone can change a man’s future.
When abiraterone was still under patent, a two-year course cost the NHS around £68,000 per patient, leading NICE to reject it on cost grounds. Since generic versions entered the market, the NHS price has fallen to about £66 a pack – bringing the cost of the same two-year course to under £2,000.
So why won’t NHS England choose to fund the drug directly and sooner?

Abiraterone is currently approved on the NHS for stage 4 prostate cancer
An NHS England spokesman told Good Health: ‘Expanding access to abiraterone for this particular type of prostate cancer was identified as one of the top priorities following a clinically-led review in May 2024.
‘But the NHS can only offer this treatment once the necessary recurrent funding [a year-on-year funding stream] is available, and this is being kept under active review.
‘Abiraterone continues to be routinely funded by the NHS in England for several forms of advanced prostate cancer in line with NICE guidance.’
By contrast, the Scottish and Welsh NHS moved quickly once the drug went off-patent, taking the view that abiraterone’s clinical and cost-effectiveness justified offering it to men whose cancer had not yet spread.
Even those in England who are able to pay can find the situation a patchy minefield to navigate. Keith ter Braak, 82, a retired Marks & Spencer director from Somerset, dug deep into his retirement savings after being diagnosed with an aggressive form of prostate cancer.
The disease was first spotted in November 2019, and Keith initially received standard NHS radiotherapy treatment followed by androgen-deprivation (hormone injections).
But in 2022, an MRI showed his cancer had returned and was locally advanced.
He moved to private healthcare under a consultant oncologist at Guy’s and St Thomas’s Hospital in London and began abiraterone alongside hormone therapy. But he was staggered at the cost with his private provider, Lloyds Clinical. ‘I’ve spent about £34,000 a year,’ he says – that’s a total of £88,000 to date.
After the drug became generic he expected to see a huge price drop, but ‘they’re still charging £2,750 per month’.
He adds: ‘£34,000 a year is money my wife and I saved for our retirement, for the things we wanted to do together.
‘If she were to become ill in future, we may not have the funds to get her the treatment she might need and that is a terrifying thought.
‘We were careful all our lives with money. I never imagined we’d be spending it like this just to get a medicine the NHS in Scotland and Wales gives to other men.’
A spokesman for Lloyds Clinical said that the private fee covers the British National Formulary’s list price for abiraterone (the formulary contains information and advice on prescribing, and drug cost prices) and other costs such as monitoring, clinic time and delivery charges.
He added: ‘There is clear demand for this medicine. While the cost can be significant, patients are opting to fund it themselves because of the potential benefits. We are now close to finalising a lower-cost package.’
Another option is self-funding the drug, which can be a cheaper option for many patients, says Professor James.
This involves paying for a private prescription for the medication, which is dispensed at High Street or independent pharmacies, which charge closer to market rates and can work out cheaper than some private health policies.
This approach can work out ‘incredibly cheap; a coffee a day’, adds Professor James, noting that the variation in the costs of generic tablets depending on the route a patient takes ‘shows how broken the system is’.
He also warns of an awful Catch-22 situation where paying privately for the drug may risk later penalties if men relapse. That’s because NHS England policy means patients are blocked from having the same class of drug if it was previously given – leaving them ‘doubly in jeopardy’, financially and clinically, says Professor James.
‘We don’t have this problem in Scotland or Wales – it’s a uniquely English failure. The data are the same everywhere. The only difference is the postcode. That’s not medicine, that’s bureaucracy.’
Just how effective abiraterone can be was dramatically highlighted by the long-running Stampede (Systemic Therapy in Advancing or Metastatic Prostate Cancer: Evaluation of Drug Efficiency) trial.
Led by Professor James and conducted jointly by teams from the Institute of Cancer Research and The Royal Marsden Hospital, both in London, this has involved many thousands of men since 2005.
Results published in The Lancet in 2022 and 2023 found that adding two years of abiraterone to standard care significantly improved the chance of survival for men – indeed the findings were among the evidence considered by NHS Wales to approve abiraterone.
Professor James finds NHS England’s reluctance to follow suit mystifying: ‘It’s one of the most effective interventions we’ve ever had in prostate cancer,’ he adds. ‘The survival benefit in high-risk disease is not small – it’s transformational.’
What’s more, Professor James believes that the approval delays will end up costing the NHS more money over time.

Keith ter Braak was diagnosed with an aggressive form of prostate cancer. He chose to go private to gain access to abiraterone alongside hormone therapy, at a staggering cost. ‘I’ve spent about £34,000 a year,’ he says – that’s a total of £88,000 to date’
He says: ‘We could stop men ever needing palliative treatment for metastatic disease if we gave abiraterone at the right time.
‘Instead, we’re forced to wait until the cancer has come back and spread before we can give them the drug, when care is palliative and much more expensive; the cost to the NHS is far higher.’
And now new research, presented to the American Society of Clinical Oncology’s conference in May, found that using artificial intelligence (AI) made the case for abiraterone even stronger.
Scientists at the Institute of Cancer Research and University College London found that AI can detect from tissue samples the men most likely to benefit from the drug.
Around one in four men with high-risk disease fall into this group – and for them, taking abiraterone cut the risk of dying within five years from 17 per cent, to 9 per cent.
NHS England itself estimates that abiraterone could benefit another 8,400 men a year if the criteria for those eligible were to be widened, according to a letter it sent to Giles earlier this year.
And indeed, when the Clinical Priorities Advisory Group (which advises NHS England on which treatments to fund) reported on abiraterone last year, it was ranked in the highest category of treatments – i.e. those offering the greatest health gains for the lowest cost to the NHS.
Yet as the report put it: ‘It has not been possible to identify the necessary recurrent headroom in revenue budgets’ (i.e. there is not the budget to make it routinely available).
There are signs that the message may be getting through. In June, Karin Smyth, minister for secondary care, told MPs that NHS England’s advisors support routine commissioning [of the drug] in principle and financial modelling was being reviewed with Prostate Cancer UK.
But this is scant comfort for patients, campaigners and experts, such as Professor James.
‘It’s indefensible,’ he says. ‘We are literally watching men die who should have been saved. Every month of delay means more men cross the line into incurable disease.’
prostate-cancer-research.org.ukprostatecanceruk.org
