
Credit: Unsplash
Depression is one of the most widespread mental health disorders worldwide, characterized by persistent feelings of sadness, a loss of interest in everyday activities, dysregulated sleep or eating patterns and other impairments. Some individuals diagnosed with depression also report being unable to pay attention during specific tasks, while also experiencing difficulties in planning and making decisions.
Recent studies have uncovered different biotypes of depression, subgroups of patients diagnosed with the condition that exhibit similar neural circuit patterns and behaviors. One of these subtypes is the so-called “cognitive biotype,” which is linked to a reduced ability to focus attention and inhibit distractions or unhelpful thinking patterns.
Researchers at Stanford University School of Medicine and the VA Palo Alto Health Care System recently carried out a study assessing the potential of guanfacine immediate release (GIR), a medication targeting neural processes known to be impaired in people with the cognitive biotype of depression.
Their findings, published in Nature Mental Health, suggest that GIR can enhance cognitive control and improve symptoms experienced by some patients diagnosed with depression.
“For decades, depression treatment has relied on trial-and-error—a process that can take years and leaves too many people suffering,” Leanne Williams, senior author of the paper, told Medical Xpress.
“Clinical guidelines emphasize the importance of integrating biological and psychological information in treatment decisions, yet psychiatry has lacked the direct biological measures to do this. That gap has been the driving force behind our work.”
Over the past 15 years or so, neuroscientists and psychiatry researchers were able to identify various depression biotypes linked to specific neural circuit dysfunctions. The cognitive biotype is marked by an impaired functioning of brain circuitry linked to cognitive control, particularly the dorsolateral prefrontal cortex and dorsal anterior cingulate cortex.
Individuals with this biological profile often say that they find it difficult to plan, focus on tasks and make decisions. Moreover, most of them responded poorly to standard antidepressants, such as selective serotonin reuptake inhibitors (SSRIs).
“Our trial was driven by a desire to move from discovery to clinical translation,” said Williams. “Could we prospectively identify this biotype using imaging, and could we then match it to a treatment designed to address its underlying circuit dysfunction?
“It represents a major step toward precision and personalized psychiatry, where treatment selection is based on brain mechanisms rather than one-size-fits-all prescribing.”
Targeting the cognitive biotype of depression
As part of their study, Williams and her colleagues first recruited individuals diagnosed with depression and asked them to complete various tests. These patients completed a clinical assessment and cognitive tests. In addition, their brain was recorded using functional magnetic resonance imaging (fMRI).
“fMRI scans were processed through the Stanford EtCere Image Processing System, to prospectively identify people with the cognitive biotype,” explained Williams.
“We then treated these people for six to eight weeks with guanfacine immediate release, a medication known to strengthen prefrontal cortical circuitry across species.
“Participants completed brain imaging before and after treatment, along with cognitive testing and clinical measures. This allowed us to determine whether the treatment engaged the target circuit and whether those biological changes aligned with improvements in depressive symptoms, cognition, and everyday functioning.”
Remarkably, the researchers found that GIR, the medication they tested, restored the function of neural circuits involved in cognitive control among the patients who took it.
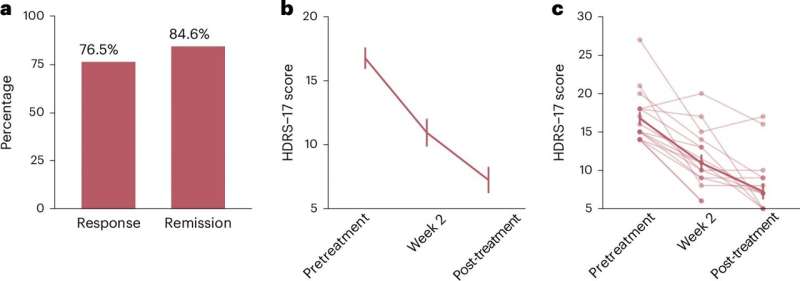
Treatment with GIR significantly improved depressive symptom severity. Credit: Nature Mental Health (2025). DOI: 10.1038/s44220-025-00510-7
In fMRI scans, this translated into an increased activation in the dorsal anterior cingulate and stronger connectivity between this region and the dorsolateral prefrontal cortex. Notably, these neural changes were also accompanied by an improved performance on cognitive tests and positive therapeutic outcomes.
Williams said, “76.5% of participants responded, and among responders, 84.6% achieved remission, substantially higher than typical remission rates with standard antidepressants.
“Overall, 65.7% achieved remission.”
Heading towards precision mental health care
Williams and her colleagues were able to identify a specific subtype of depression using fMRI scans. They then investigated the effects of a treatment that targets the brain circuit most affected in patients with this depression subtype and found that it restored the circuit’s function.
“We found that circuit engagement aligns with clinical recovery, pointing to a true mechanistic pathway,” said Williams.
“Practically, this opens the door to brain-based, personalized approaches to precision depression care, where diagnosis and treatment selection reflect underlying brain circuitry rather than symptoms alone. It is a prototype for a future where psychiatry has the same precision tools and personalized care approaches seen in other fields of medicine.”
The results of this recent study could have important implications for the future treatment of depression, particularly among some patients that typically respond poorly to conventional antidepressants.
The approach employed by Williams and her colleagues could soon be applied to the study and treatment of other depression subtypes and even other mental health disorders.
“This work is just the beginning. It lays the foundation for a new era in mental health care,” said Williams. “Next, we will conduct larger, randomized controlled trials comparing guanfacine with standard treatments. We also plan to expand to additional sites to establish reproducibility and scale the approach.”
In their next studies, the researchers will extend their precision medicine strategy and use it to study other depression biotypes. Eventually, they hope to identify the most suitable treatments for these different subtypes among various pharmacological drugs, neuromodulation tools and behavioral interventions.
“We will also continue building clinical infrastructure, with ongoing development of the Stanford EtCere Image Processing System, so that imaging-based biotype assessment can be integrated into routine care,” added Williams.
“Our vision is a future where mental health care is grounded in objective brain measures, so each person receives the right treatment for the right mechanism at the right time. This study demonstrates that such personalized, precision treatment pathways are not only possible but within reach.”
Written for you by our author Ingrid Fadelli, edited by Sadie Harley, and fact-checked and reviewed by Robert Egan—this article is the result of careful human work. We rely on readers like you to keep independent science journalism alive.
If this reporting matters to you,
please consider a donation (especially monthly).
You’ll get an ad-free account as a thank-you.
More information:
Laura M. Hack et al, A stratified precision medicine trial targeting α2A-adrenergic receptor agonism as a treatment for the cognitive biotype of depression, Nature Mental Health (2025). DOI: 10.1038/s44220-025-00510-7.
© 2025 Science X Network
Citation:
Precision medicine intervention found to ease symptoms of a depression biotype (2025, November 5)
retrieved 5 November 2025
from https://medicalxpress.com/news/2025-11-precision-medicine-intervention-ease-symptoms.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.

