NEW ORLEANS — When added to standard lipid-lowering therapy, olezarsen, a drug approved in 2024 for patients with familial chylomicronemia syndrome, significantly lowered triglycerides and reduced the risk for pancreatitis by 85% in unselected patients with severe hypertriglyceridemia.
In two phase 3 trials, the reductions in triglyceride levels, which reached 72% at the highest dose of olezarsen, were accompanied by reductions in apolipoprotein C-III, remnant cholesterol, and non-high-density lipoprotein (HDL) cholesterol. All changes were sustained at 12 months, according to the lead investigator, Nicholas A. Marston, MD, MPH, a cardiologist who specializes in familial hypercholesterolemia and is affiliated with Brigham and Women’s Hospital in Boston.
Marston presented the results of the identically designed phase 3 CORE-TIMI 72a and CORE TIMI 72b trials in a late-breaking session at American Heart Association (AHA) Scientific Sessions 2025. The data were also published in The New England Journal of Medicine.
No Prior Therapy Treated Severe Hypertriglyceridemia
Severe hypertriglyceridemia, which is associated with an increased risk for cardiovascular events, myocardial infarction, and stroke, as well as acute pancreatitis is notoriously difficult to treat with current therapies or diet. Alone or together, efficacy is limited, according to Marston.
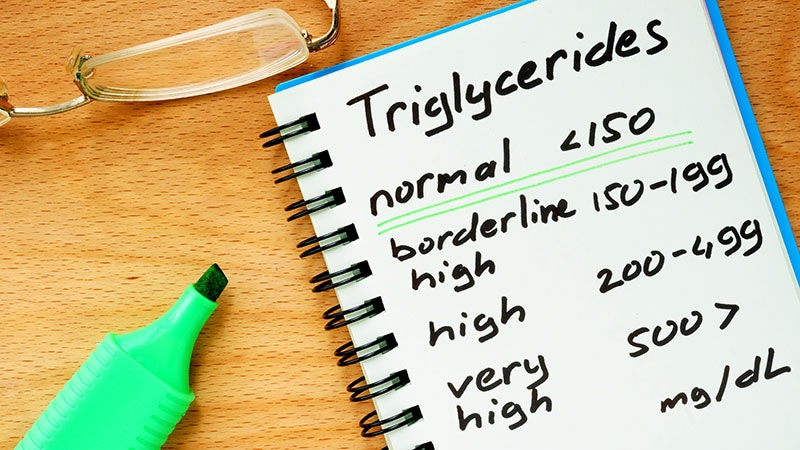
In the phase 3 trials, more than 85% of patients on either of the two study doses — 80 mg or 50 mg — of olezarsen reached triglyceride levels below 500 mg/dL at 12 months and up to 54% had levels below 150 mg/dL, Marston reported.
Despite its current indication for familial chylomicronemia syndrome, granted on the basis of the phase 3 BALANCE trial, olezarsen had not been previously tested specifically for the treatment of severe hypertriglyceridemia outside of this indication. All 617 patients recruited for the CORE-TIMI 72a trial and 444 recruited for the CORE-TIMI 72b trial had a fasting triglyceride level of at least 500 mg/dL on two occasions while receiving statins. Researchers excluded those with familial chylomicronemia syndrome.
Patients enrolled in these international, multicenter trials were randomized 1:1 to 50 mg or 80 mg of olezarsen and then rerandomized in a 2:1 fashion to active therapy or placebo. The primary outcome was percent change in fasting triglyceride levels at 6 months.
Secondary outcomes included changes in other lipids at 6 and 12 months, triglyceride levels below certain thresholds, and rates of acute pancreatitis events.
In the CORE-TIMI 72a trial, the reductions in triglyceride levels at 6 months relative to placebo were 62.9 and 72.2 percentage points for the 50-mg and 80-mg doses, respectively. In CORE-TIMI 72b, these reductions were 49.2 and 54.5 percentage points, respectively. The differences in both trials were statistically significant (P < .001 for all).
Results showed greater reductions in apolipoprotein C-III, remnant cholesterol, and non-HDL cholesterol with both olezarsen doses relative to placebo in the two trials, all of which were statistically significant (P < .0001 for all).
Olezarsen Reduced Acute Pancreatitis Risk by 85%
When the data from the two trials were combined, the seven acute pancreatitis events that occurred in five of the 705 patients randomized to olezarsen translated to an observed incidence rate of 1.01 per 100 patient-years. The 22 events that occurred in 17 of the 356 patients in the placebo group translated to an observed incidence rate of 6.23 events per 100 patient-years.
These differences produced a rate ratio of acute pancreatitis for olezarsen relative to placebo of 0.15, representing an 85% risk reduction (P < .001), according to Marston. The number needed to treat in a 1-year period to avoid an acute pancreatitis event was 20. He noted that 25 of the 29 cases of acute pancreatitis occurred in patients with a baseline triglyceride level of at least 880 mg/dL and a history of pancreatitis.
Both doses of olezarsen were reasonably well tolerated. The total proportion of the low-dose and high-dose olezarsen relative to the placebo groups were comparable for any adverse event (75% and 76% vs 75%). The rate of serious adverse events was numerically lower in the olezarsen groups (9% and 11% vs 14%). The rate of discontinuations due to an adverse event were numerically higher in the low- and high-dose olezarsen groups (3% and 4% vs 2%), but this finding fell short of statistical significance (P = .09).
In a substudy of 252 patients in the CORE-TIMI 72a and 72b trials, researchers conducted hepatic MRI at baseline and again at 12 months. At baseline, the median hepatic fat fraction was 13.9%. At 12 months, it increased 0.14 percentage points in the placebo group, 2.28 percentage points in the olezarsen 50-mg dose group and 4.18 percentage points in the 80-mg dose group (P < .001 for olezarsen vs placebo). Elevations in liver enzymes at least three times above the upper limit of normal were also more common in low-dose and high-dose olezarsen groups than in the placebo group (2.6% and 6.9% vs 2.0%; P = .003).
Marston called the clinical relevance of these liver changes “unclear.”
The researchers also noted an increase in HbA1c with both doses of olezarsen in patients with diabetes.
Cardiologists Need to Recognize New Therapy for Triglycerides
For cardiologists, having an agent capable of dramatically lowering triglyceride levels in hypertriglyceridemia is potentially important, according to Catherine Benziger, MD, director of Research at Essentia Health Heart and Vascular Center in Duluth, Minnesota.
Although elevated triglycerides are not the No. 1 priority for most cardiologists, Benzinger said this is largely due to the fact that therapies have had limited efficacy, making it difficult to show an improvement in cardiovascular outcomes.
However, Benziger, who is an adjunct professor at the University of Minnesota Medical School and serves on the American College of Cardiology Prevention of Cardiovascular Disease Council, noted the participation of triglycerides in residual cardiovascular risk after control of low-density lipoprotein cholesterol is well established.
“With effective therapies, I think more cardiologists will be able to start thinking about control of hypertriglyceridemia,” she said.
Cardiovascular outcome trials are now needed to confirm a benefit, but Benziger said that she is willing to consider drugs like olezarsen when patients are referred with very severe hypertriglyceridemia, even in the absence of cardiovascular event trials.
Ultimately, “this drug is going to be game-changing for patients [with severe hypertriglyceridemia],” she said.
“Cardiologists might not be that focused on this lipid abnormality, but patients really care about this,” she added. While this concern is concentrated in patients who want to avoid acute pancreatitis events, Benziger noted that very severe hypertriglyceridemia like that of patients enrolled in CORE-TIMI 72a and 72b does make clinical cardiologists uncomfortable.
Robert Rosenson, MD, director of the Metabolism and Lipids Program at Icahn School of Medicine at Mount Sinai in New York City, cautioned that not much can be said about olezarsen for managing cardiovascular risk on the basis of the CORE-TIMI 72a and 72b data, even if a treatment for severe hypertriglyceridemia is welcome.
In evaluating these results, he expressed concern about the increase in hepatic fat and the signal of worsening glycemic status in patients with type 2 diabetes.
“I think there is a need to control diabetes before you start patients on this drug,” said Rosenson, who served as a discussant for the trials.
Yet he agreed the findings are clinically meaningful, particularly at this time for patients with severe hypertriglyceridemia who have or are at risk for acute pancreatitis events.
The TIMI-CORE 72a and 72b trials received financial support from Ionis. Marston reported a financial relationship with Ionis, Amgen, AstraZeneca, Beckman Coulter, Novartis, and Pfizer. Benziger reported a financial relationship with Novartis. Rosenson reported financial relationships with Amgen, Arrowhead, Avilar, CRISPER Therapeutics, Editas, GlaxoSmithKline, Eli Lilly, Intercept, Life Extension, Lipigon, New Amsterdam, Novartis Regeneron, Rona, and Verve.
Ted Bosworth is a medical writer in New York City.