By Michelle Crouch
When city of Charlotte workers get sick, they don’t have to wait weeks for a primary care appointment or shell out a co-pay for an urgent care visit. Instead, they can often be seen on the same day, at no charge, at one of six local clinics run by Marathon Health.
Like a growing number of other employers, the city has embraced a health care model known as direct primary care that sidesteps traditional health insurance for its 9,000 workers and 3,500 retirees. Under the arrangement, the city pays Marathon a flat monthly fee for each employee; in turn, employees are guaranteed same-day or next-day doctor’s appointments.
Think of it “like a gym membership for health care,” said Dr. Meaghann Bernardy, regional medical director for Marathon Health’s East region.
At the appointments, employees can get care for minor injuries or illnesses, nutrition coaching, lab work, mental health therapy and even physical therapy. Some of the clinics are open outside of typical business hours. Depending on their insurance plan, employees pay nothing or a $30 fee.
The employees still have traditional insurance for bigger-ticket needs, such as specialist visits, complex procedures and hospital stays.
Christina Fath, the city’s benefits manager, told a group of local human resources professionals last week that the city has saved millions since contracting with Marathon in 2016 by reducing emergency room visits and making it easier for city workers to get care before health problems turn into crises.
“Our health care costs have not gone up as much as national averages,” she said. “While this may be attributed to various factors, the data shows that if our plan members had sought the same care in another health care setting, the plan would have paid more for that same health care. We’ve seen a reduction in non-emergent emergency room visits, urgent care visits, lab spend and (an) increase in preventive care visits and screenings.”
Employees also save money, she said, by avoiding copays and coinsurance payments. “That’s money in their pockets,” she said.
Popping up all over
The direct primary care model is catching on nationwide. Between 2017 and 2021, direct primary care memberships nationwide grew 241%, according to a 2023 industry report. Another analysis predicted the global market for direct primary care would grow from $61.34 billion in 2025 to $96.4 billion in 2033.
Some direct primary care practices operate like so-called concierge medicine practices, which sell memberships directly to patients. But benefits experts said a lot of the growth has been employer-based, like the city’s plan with Marathon, as companies look for ways to provide better care for their workers while keeping soaring health care costs in check.
“The whole issue has always been that it’s difficult to get your employees to go to a primary care physician, so they end up going to ER instead,” said Jon Rankin, CEO of the North Carolina Business Coalition on Health, an employer group that advocates for improved health care delivery.
“Oftentimes, folks are waiting six months to a year to see somebody,” he said. “Employers are saying: ‘What are our options? How can we improve that?’”
Jordan Harris, an employee benefits consultant for Main Street Insurance Group, said direct care providers are “popping up all over the place.” He mo said some operate strictly through telehealth while others, like Marathon, run on-site or near-site clinics.
The monthly fee typically ranges from $25 to $100 per person and can depend on the total number of employees, their ages and how many extra services, such as physical therapy or health coaching, are included.
New law could boost direct care trend
So why isn’t every company jumping on the direct primary care bandwagon? Rankin and Harris said employers with staff scattered across multiple locations can run into challenges guaranteeing that every worker has a clinic nearby. Even if geography isn’t an issue, some companies hesitate to make the up-front investment or aren’t convinced of the promised long-term savings, they said.
However, Harris said he expects the trend to accelerate as a result of recent federal legislation that allows Health Savings Account dollars to be used for direct primary care. Previously, he said, many employers hesitated to offer it to workers on high-deductible plans who have HSAs to pay for their out-of-pocket costs.
About 20 percent of the city’s workers are currently on such an HSA plan and have to pay a nominal fee for using Marathon’s services, Fath said.
Marathon Health is one of the largest employer-based providers of direct primary care in the U.S., with more than 720 locations nationwide, including 60 in North Carolina. In addition to the city of Charlotte, it has contracts with 27 other N.C. organizations, including Mecklenburg County, Lenovo and Reynolds American.
Marathon estimates that employers who sign up save $1,100 per year on each enrolled worker, and up to $4,400 annually on those with a chronic condition.
Tryon Medical’s homegrown approach
In Charlotte, Tryon Medical Partners has built a direct primary care program that has steadily expanded since 2019 and now serves about 25 Charlotte-area employers, according to Chief Operating Officer Jordan Archer.
Archer, who described the model as “all-you-can-eat primary care,” said enrolled workers receive unlimited, preferred access to Tryon Medical doctors and longer appointments than other patients.
Local companies see the program as a way to cut costs and as a retention benefit, Archer said. What sets Tryon apart, he added, are its local providers.
“Do you want a physician who just got plopped down in this market coordinating your care?” he said. “Or do you want a doctor who has been here 20 years building their career, who knows the best orthopedic surgeon to do your hip?”
More time with patients
Doctors said they like the direct care model because they can avoid the hassle of dealing with health insurers and spend more time with patients.
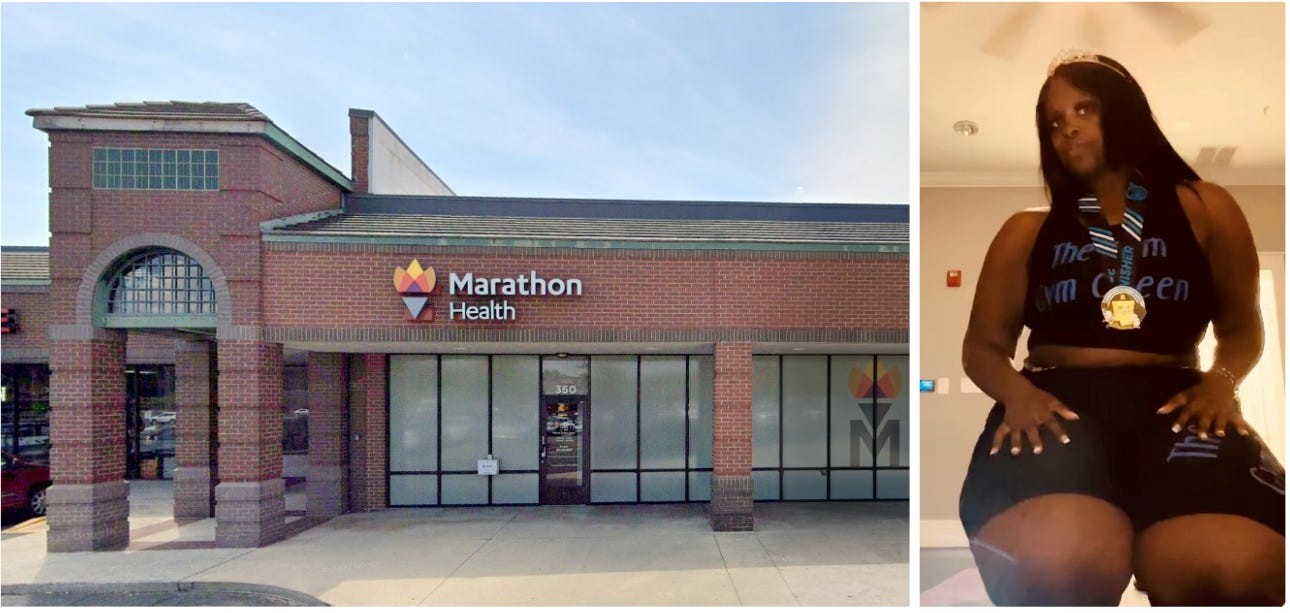
Family medicine physician Ajiri Barnes joined Marathon Health in 2023 after 18 years at a large Charlotte-based hospital system. At the hospital, she said, she was pressured to refer patients to in-house specialists, not always the ones she felt were best for her patients. And appointments were limited to 20 minutes.
“I didn’t feel like I had the time to spend with patients to do what they needed,” she said. “Invariably, you ran behind. Then you’re charting for hours after work.”
Although Barnes took a small pay cut when she left the hospital system, she said the change was worth it. She now sees about half as many patients per day, and she spends 30 to 40 minutes with each. She also leaves on time almost every day.
“I finally feel like I can finally practice medicine the way it should be practiced,” she said. “In my old job, patients sometimes waited a year to see me. Here, they can see me tomorrow.”
Support beyond primary care
Menshana Briana McNeil, 25, receives care at a Marathon Health clinic through her father, a Charlotte sanitation worker. Nearly three years ago, she said, she asked her Marathon Health physician for help losing weight and was paired with nutrition coach Amy Hanson. They met twice a week at no cost.
McNeil said the coach’s support helped her to lose 63 pounds, run her first 5K and reverse her prediabetes. At Hanson’s urging, she also completed her CNA certification, which helped her to get a better-paying job.
‘She is like my guardian angel,” she said. “I don’t know where I would be without her.”
McNeil will soon turn 26 and age off of her father’s insurance plan — a change she is already dreading.
“It’s hard to believe that all of this is included because he works for the city,” she said. “When I turn 26, I’m going to cry.”
This article is part of a partnership between The Charlotte Ledger and North Carolina Health News to produce original health care reporting.
You can support this effort with a tax-deductible donation.
Republish This Story
Republish our articles for free, online or in print, under a Creative Commons license.