
Vivek Kaul, MD, FACG, FASGE, AGAF
Division of Gastroenterology and Hepatology
University of Rochester Medical Center
Rochester, New York

Sarah Enslin, PA-C
Division of Gastroenterology and Hepatology
University of Rochester Medical Center Rochester, New York
As the landscape of GI oncology grows more complex, advanced practice providers play an increasingly important role in delivering high-quality, patient-centered care in highly specialized interdisciplinary settings. From risk assessment and genetic counseling to palliative care and precision medicine, APPs are a key part of multidisciplinary teams working to improve outcomes and experiences for patients facing gastrointestinal cancers.
For this installment of GI APP Corner, we highlight the collaborative efforts of physicians and APPs across several key areas of GI oncology. We sat down with team members at the forefront of GI endoscopy, palliative care, and genetic counseling, each offering insight into how team-based models are transforming care and better supporting both patients and providers.
These conversations highlight what many in GI oncology already know: Integrated, team-based care—driven by the expertise and adaptability of highly specialized APPs—is not just the future of cancer care but is its foundation today.
Whether leading hereditary risk clinics, guiding patients through difficult conversations and decisions, or advancing precision medicine, APPs are helping shape the evolution of GI oncology care in powerful, patient-centered ways.
As the field continues to evolve, so too does the importance of fostering APP leadership, autonomy, and innovation within multidisciplinary teams. The models shared here offer both inspiration and a blueprint for teams looking to strengthen their approach to GI oncology care through deeper collaboration and shared purpose.
GEN: What does collaboration between physicians and APPs look like in your practice?
Ms. Gomez: Effective collaboration in GI oncology requires intentional role delineation, open communication, and a shared commitment to patient-centered care. Given the complexity of GI cancers—often marked by malnutrition, luminal obstruction, bleeding, and treatment-related toxicities—specialized, streamlined support is essential.
At our institution, we’ve implemented a parallel practice model with tiered inpatient rounding. This gives APPs a high degree of autonomy while maintaining physician availability for complex consultations and endoscopy. Daily interdisciplinary huddles serve as a touchpoint for case discussions and care planning, reinforcing a strong culture of collaboration and partnership in patient care.
APPs enhance patient access by triaging urgent symptoms, ensuring timely follow-up after discharge, and facilitating diagnostic and palliative procedures. Mentorship from physicians remains central. They provide guidance on clinical reasoning, procedural skills, and research engagement. This approach improves patient outcomes and fosters professional growth and cohesion within the team.
GEN: What are some unique challenges in GI oncology that your APP team is well positioned to address, either clinically or with respect to patient support?
Dr. Kachaamy: GI oncology presents both clinical and psychosocial challenges due to its high acuity and symptom burden for the patient. APPs are uniquely equipped to respond to these challenges through expert clinical management and patient support.
Clinically, they help manage adverse events such as immunotherapy-related toxicity, chemotherapy-induced side effects, and bowel dysfunction. Timely triage and proactive interventions help prevent hospitalizations, readmissions, and delays in care. APPs also play a central role in coordinating urgent diagnostic and interventional procedures, helping optimize pre-procedure patient preparation, and ensuring that post-endoscopy follow-up and referrals are in place.
On the support side, APPs provide continuity across care settings, offering education, anticipatory guidance, and caregiver support. Their integrated role bridges gaps in care, helping patients and families navigate the emotional and physical toll of cancer treatment.
GEN: How do you foster professional growth and autonomy within your APP team, and how does this translate into better care for patients?
Dr. Kachaamy: We foster growth through a structured, supportive framework focused on skill building, leadership development, and continuous learning. Clearly defined roles and protocols enable APPs to run clinics independently while collaborating with physicians on complex cases.
Our onboarding process allows for progressive responsibility and mentorship, helping APPs build confidence in high-acuity care. Ongoing mentorship extends beyond clinical oversight, guiding diagnostic reasoning and decision-making in complex situations.
APPs are actively involved in protocol development, quality improvement, and institutional decision-making. We also invest in professional development, with protected time for education, conference attendance, and participation in journal clubs and tumor boards.
This culture of growth directly benefits patients, improving access, streamlining care, and strengthening the team’s ability to meet evolving patient needs in the GI oncology space.
GEN: What does an ideal multidisciplinary model look like to you for managing hereditary cancer syndromes, and what role do APPs play in driving that model forward?
Ms. Gomez: An ideal model for managing hereditary cancer syndromes is proactive, comprehensive, and deeply multidisciplinary. It includes gastroenterologists, oncologists, genetic counselors, surgeons, dietitians, and social workers, each collaborating to provide risk assessment, screening, early intervention, and long-term support.
APPs often initiate this process, collecting detailed family and personal histories and identifying patients who need genetic evaluation. They help guide discussions around surveillance protocols, risk reduction strategies, and personalized lifestyle interventions.
As care coordinators, APPs ensure smooth communication across specialties, helping patients navigate the complex pathway of hereditary cancer risk management. Their involvement empowers patients to make informed decisions and ensures continuity of care.
GEN: What inspired your focus on genetics within the GI oncology space, and how has your role evolved as precision medicine becomes more central to care?
Ms. Weaver: My interest in genetics stems from a desire to help patients understand the “why” behind their cancer. For many, especially those diagnosed at a young age, genetics can provide that answer. It also helps shift oncology from a one-size-fits-all model to precision medicine, enabling tailored treatment strategies based on genetic profiles.
As genetic testing becomes standard in cancer care, my role has evolved to guide patients and providers through increasingly complex testing and decision-making. There are several ethical, clinical, emotional, and psychological elements that we help patients get through.
GEN: As genetic testing becomes more complex, how do you ensure patients and colleagues understand the implications of test results and appropriate next steps?
Ms. Weaver: Education is central to our approach. At Mayo Clinic, we’ve embedded genetics education into our medical training programs, partnered with community hospitals, and developed conferences focused on precision medicine and hereditary cancer syndromes. Through these initiatives, we’re equipping providers with the knowledge they need to integrate genetics into care, and we aim to educate our patients along the way as new information becomes available.
GEN: How do you navigate challenging conversations around prognosis, advance care planning, and symptom management?
Dr. Farfour: Navigating these conversations begins with deep listening and presence. I strive to create a space where patients and families feel seen, heard, and supported, meeting them where they are emotionally and cognitively. I use structured communication frameworks such as SPIKES and REMAP (Table), integrating empathetic statements and active inquiry to understand their goals and values.
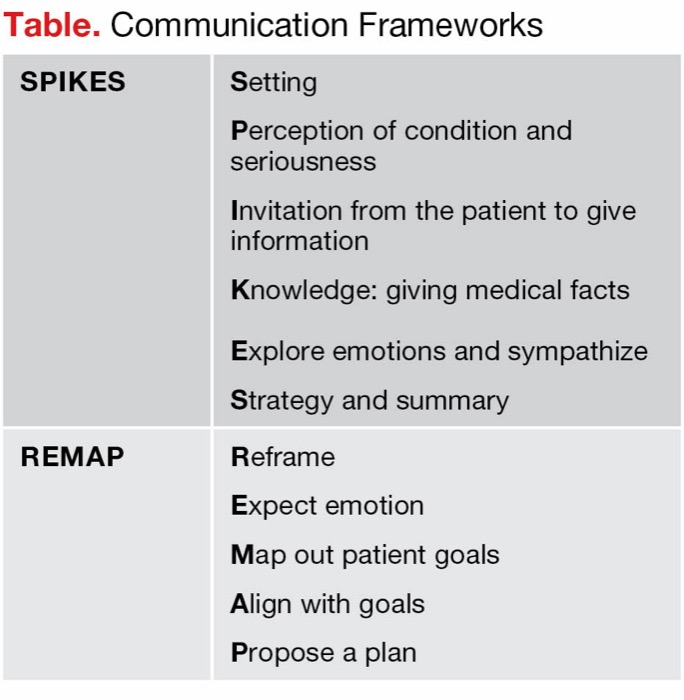 Table. Communication Frameworks SPIKESSetting
Table. Communication Frameworks SPIKESSetting
Perception of condition and seriousness
Invitation from the patient to give information
Knowledge: giving medical facts
Explore emotions and sympathize
Strategy and summary
REMAPReframe
Expect emotion
Map out patient goals
Align with goals
Propose a plan
Advance care planning is not a one-time event; it’s a series of conversations rooted in trust. I normalize the process by framing it as a proactive process of love and dignity. When discussing prognosis or progression, I balance honesty with compassion, offering clarity while holding space for hope in its many forms.
Symptom management is integral to these conversations. By addressing distressing symptoms early and comprehensively—whether through physical, emotional, or spiritual ways—I help patients maintain their quality of life and autonomy.
GEN: How do you coordinate with oncologists, gastroenterologists, surgeons, and others to ensure patients receive holistic support?
Dr. Farfour: Interdisciplinary collaboration is at the heart of quality palliative care. I work closely with oncologists, gastroenterologists, surgeons, and other specialists to ensure that care is medically appropriate and aligned with the patient’s goals and preferences. This means engaging early in the care continuum, joining tumor boards, contributing to care planning discussions, and often acting as a bridge between teams and the patient. I bring a lens that integrates symptom expertise with a whole-person perspective—addressing not just the disease, but the person living with it.
By fostering open, respectful communication and building trust with my colleagues, we collaborate to create care plans that are both evidence-based and deeply personalized.
GEN: What are some misconceptions about palliative care that you frequently encounter, and how do you work to reframe them?
Dr. Farfour: One of the most common misconceptions is that palliative care is synonymous with end-of-life or hospice care. Palliative care is about enhancing quality of life at any stage of a serious illness, often alongside curative or life-prolonging treatments.
Another misconception is that involving palliative care means “giving up.” I reframe this by helping patients and families see that palliative care is about showing up for what matters most to them. It’s about supporting people to live as well as possible for as long as possible.
I also educate clinicians about the value of early palliative involvement, how we can improve symptom control, reduce hospitalizations, and support difficult decisions, which improves patient outcomes and satisfaction for patients and the care team.
This article is from the September 2025 print issue.


