With over 40 million Nigerians suffering from mental health disorders as against about 200 psychiatrists serving the entire country, over 85 per cent of Nigerians lack access to reliable, well-structured, and well-organised mental health services. With dire socioeconomic conditions that compel the economy to work in fits and starts, experts emphasise the compelling need to integrate mental health services into the primary healthcare system to ensure access for people in rural communities. NKECHI ONYEDIKA-UGOEZE reports that the country must also implement the Mental Health Policy that has remained unimplemented for 36 years until the recent review in 2023, therefore bequeathing to the country an economic burden that exceeds N21 billion yearly.
Since losing his N220,000 monthly paid job as a line supervisor in a prominent bakery in Lagos State in late 2020, Obanor, E.O., a graduate of sociology, who obtained a certificate in catering from a government vocational institute, spent the better part of 2021 applying to over 30 companies for employment, none of which responded in the affirmative.
Grossly demotivated, he veered into pastry making to keep body and soul intact. But the arrival of the President Bola Ahmed Tinubu-led government technically threw a spanner in his works when petrol subsidy was removed, and the price of flour, vegetable oil and sundry raw materials used by Obanor spiked.
Within months, the high cost of living wiped out his working capital and this was shortly after his second child was delivered. With dire conditions unabating, suicidal thoughts assailed him daily. Pronto, one of the firms he applied to, reached out to him, offering him the same role he last played in the bakery. Obanor was saved by the bell!
Chukwuma Ibezim, a computer hardware dealer at the Computer Village, Ikeja, recalled how a next-door neighbour at his former compound was saved from something untoward after he was defrauded in the line of duty.
“Kunle ‘K’, as we used to call him, was a lady’s man; always very decent, courteous, and was liked by everybody. So, it was easy for everyone to notice that something was wrong with him. When close neighbours inquired about his new disposition, he dismissed all fears, insisting that he was okay.
“A persistent neighbour who knew K’s relatives brought the matter to their attention and after investigation, it was revealed that he was duped, and his employer was using half of his salary to defray the loss incurred. They eventually found a way around it and he got back himself with strict medical care after being depressed for months,” the Abia State-born merchant said.
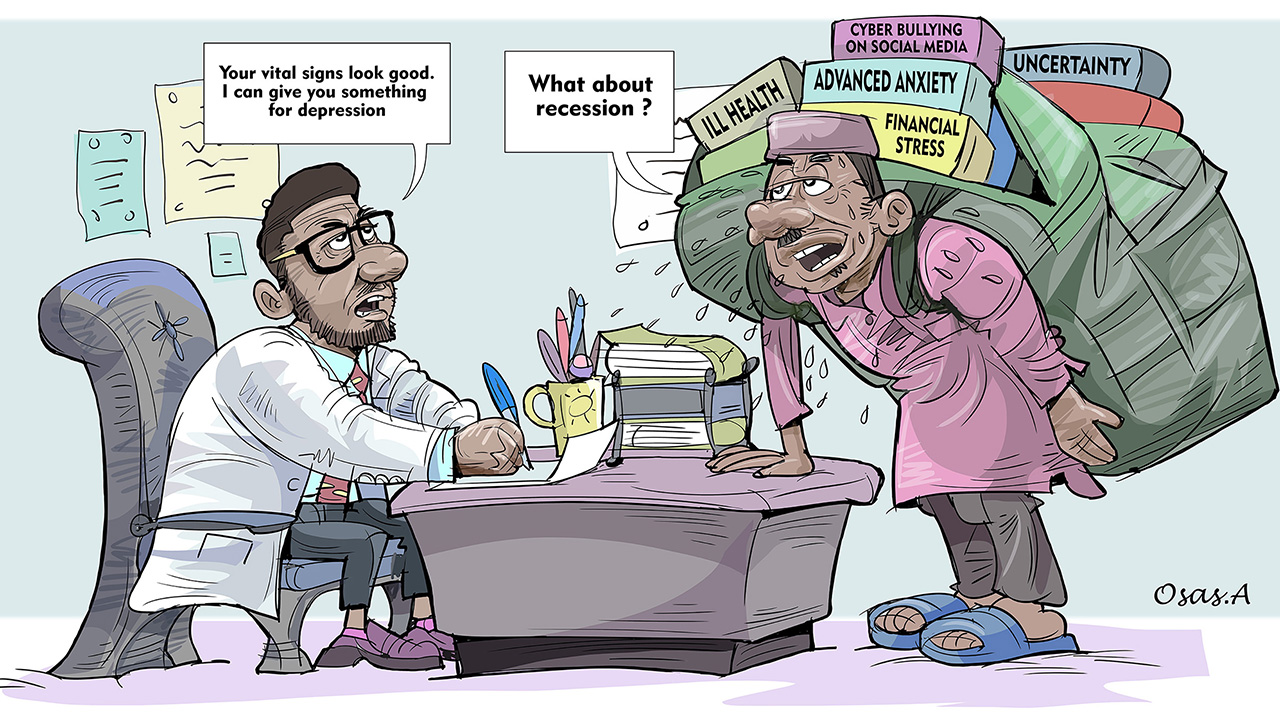
While the two above were salvaged from what could have taken their lives eventually, millions of Nigerians are daily losing their mental health due to unforeseen circumstances, economic concerns, unmet expectations and other challenges, which force them to believe that they have run out of options, or leave them at their wits’ end.
In its latest Nigeria Development Update (NDU) released on Wednesday, the World Bank warned that gains of the reforms – subsidy removal, foreign exchange (FX) market liberalisation and tax system recalibration – remain fragile and unevenly distributed, with the historical structural imbalance in growth and economic inequality deepening.
It pointed at rising poverty, high inflation and falling purchasing power as major setbacks to the reforms, advising the authorities to reduce food inflation, improve the use of public resources for development and strengthen the social safety net to “bring gains home to Nigerians”.
The report noted that the number of poor Nigerians rose from 81 million (40 per cent) in 2019 to 139 million or 61 per cent this year, with projections putting the absolute poverty rate at 141 per cent next year.
From 2019 to 2023, the report added, average consumption fell by 6.7 per cent, highlighting the sharp deterioration in the welfare of the average Nigerian.
Indeed, Nigeria is battling a mounting mental health emergency and experts, in painting how dire the situation is, warned that 85 per cent of those in need lack access to care. With only nine psychiatric hospitals and fewer than 300 psychiatrists nationwide, millions are left vulnerable to poverty, stigma, and worsening psychological distress.
According to reports, across the country, mental health facilities are experiencing an unprecedented increase in patient intake, with some of the facilities reporting over a 200 per cent rise in daily cases.
A further confirmation of the critical scenario that is engulfing the country is also reports that from 2020 to 2023, the country’s suicide rate doubled, and became a major cause of under-40 death.
As the country joins the rest of the world to mark World Mental Health Day today, specialists are stressing the need for urgent action to close the widening mental health gap, the depth of which is evident in Nigeria’s threadbare mental health infrastructure, a situation worsened by a severe shortage of mental health professionals.
According to the Association of Psychiatrists in Nigeria (APN), only about 200 practising psychiatrists serve a population exceeding 220 million.
Available data credits the country with roughly 1,000 psychiatric nurses, 319 licensed clinical psychologists, a handful of psychiatric social workers and occupational therapists, far below the global benchmark of one psychiatrist for every 10,000 patients.
The World Health Organisation (WHO) estimates that about 20 per cent of Nigerians, representing roughly 40 million people, are affected by mental illness. It also warns that poor mental health contributes to low productivity, absenteeism, and high staff turnover. Depression and anxiety alone account for an estimated loss of 12 billion workdays each year, costing the global economy about $1 trillion annually.
Globally, economic losses from mental disorders were projected to rise from $1.6 trillion in 2019 to $3 trillion by 2030. In Nigeria, the economic burden of mental illness is equally significant, with some estimates placing the yearly cost at more than N21 billion.
Experts say the costs of medication, hospital care, and long-term treatment for severe conditions such as schizophrenia continue to deepen the strain on families.
They noted that although effective treatment options exist, most people with mental disorders are unable to access care. Many also face stigmatisation, discrimination, torture, and human rights abuses.
In their estimation, mental health advocates maintain that the high cost of services, inadequate insurance coverage, poor infrastructure, and shortage of skilled professionals have continued to worsen the present condition and push more Nigerians into distress.
In addition to others, World Mental Health Day, observed yearly on October 10, aims to raise awareness about mental health issues and promote global support for individuals affected by these issues worldwide.
The focus is timely, given the growing global burden of mental illness. Nearly one in seven people lives with a mental disorder, and in 2021, about 1.1 billion people were recorded as living with mental health conditions, with anxiety and depression being the most common.
Insecurity, dire socio-economic conditions as enablers of mental illness
RISING insecurity, armed robberies, and unemployment are among the worsening socio-economic conditions that are driving a surge in mental health disorders across the country, particularly among young adults and adolescents.
Speaking with The Guardian, the President of the Association of Psychiatrists in Nigeria (APN), Prof Taiwo Obindo, emphasised that the rising economic hardship facing Nigerians is taking a toll on mental health.
“The impact is such that people’s economic power has been reduced, their needs have increased, and the cost of living has gone up. Several people have been retrenched, many are unemployed, and quite a number of those employed are underemployed. All these affect their mental health.
“Generally, there has been an increase in mental health conditions even among young adults and adolescents. There has also been an upsurge in the use of psychoactive substances, which has further affected the mental health of the population,” he said.
Obindo informed that about 85 to 90 per cent of Nigerians living with mental health conditions do not have access to proper care, largely due to myths and misconceptions about the causes of mental illness, as well as the high cost of treatment and inadequate medical facilities.
“Concerning those who have access to the right treatments, we believe that between 10 and 15 per cent of them can access appropriate care. So, the mental health gap shows that about 85 to 90 per cent of people who have mental health conditions do not get the right care,” he explained.
He added that while the WHO recommends at least one psychiatrist for every 10,000 people, Nigeria has only one psychiatrist for about one million citizens.
“We have fewer than 250 psychiatrists presently working. As you know, I am the President of the Association of Psychiatrists in Nigeria, so I know the number regularly leaving the country. We probably have between 200 and 250, but it’s difficult to say exactly how many of them are remaining because almost every day, you hear that someone else has left. It’s no longer limited to the younger ones; even the more experienced ones are leaving,” he said.
“So, on average, we have a ratio of one psychiatrist to about a million Nigerians. It is grossly inadequate, and most of these psychiatrists are in urban areas. More than 65 per cent of our population live in rural areas, and they cannot access care. When they consider the cost and means of transportation to the city, most eventually resort to traditional or faith healers.”
Obindo, who decried the rising cost of managing mental illnesses, said the cost of medication and access to care has increased more than fourfold, even though people’s incomes have not improved. He also lamented that many Nigerians still believe that mental illness is caused by spiritual forces or evil deeds, which often influences where they seek help.
According to him, the integration of mental health services into primary health care, meant to serve as the ninth component of the primary health care system since 1996, has yet to be implemented. “It hasn’t been done, and that is affecting services,” he said.
The APN president called for greater attention to the issue of stigmatisation, discrimination, and torture faced by people living with mental health conditions.
“If someone is seen to have a mental health condition in their family, people will not marry into that family. And when they marry and later find out that the person has a mental illness, they often refuse to continue the marriage. These are significant barriers to accessing care because people can’t open up about their condition. Instead of taking them to nearby facilities, families send the infirm to villages where they are tied up, or subjected to degrading treatment,” he said. Obindo urged the government to prioritise mental health by providing incentives and better remuneration for professionals who risk their safety treating patients.
He also called for the full implementation of the Mental Health Act, which was passed and gazetted in 2023, and for the allocation of more funds to improve mental health services nationwide. He stressed the need for greater public awareness to encourage more Nigerians to seek help and urged the government to ensure comprehensive coverage of mental health care under the National Health Insurance Scheme.
Shedding light on other causes of mental illness, Obindo said: “We believe that genetics plays a significant role in the development of mental health conditions. It is said that poverty and mental health are bidirectional. Those with mental health conditions are more likely to gradually move down the socio-economic ladder and become poor, particularly in chronic cases. Exposure to trauma, whether physical, psychological, or emotional, can predispose individuals to developing mental health conditions, including the use of psychoactive substances.”
Unimplemented mental health policy widens growing gap
NIGERIA’S growing mental health gap is not just a social or humanitarian crisis, but a severe and multifaceted drag on the country’s economy on the one hand. On the other hand, the consequences are indelible and profound, impacting productivity, human capital, public finances, and social stability.
For instance, mental health conditions like depression, anxiety, and PTSD directly impair concentration, energy levels, decision-making, and reliability, leading to absenteeism, high staff turnover, increased healthcare burden, and loss of income/ livelihood.
Among children and adolescents, mental health issues exacerbated by poverty, conflict, and societal pressures lead to poor school attendance, difficulty concentrating, and higher dropout rates.
Consultant psychiatrist and acting Medical Director of the Federal Neuropsychiatric Hospital, Yaba, Lagos, Dr Olugbenga Owoeye, while lamenting the growing gap in the mental health system, pointed out that “the country’s limited facilities and weak health infrastructure have left millions without proper support. That is why this year’s theme is ‘Access to Services,’ especially in mental health catastrophes and emergencies. The emphasis now is to make services accessible, affordable, and reliable. We only have nine federally owned psychiatric hospitals in the whole country. We should have at least one in every state so that access to services will improve,” he said.
The psychiatrist emphasised the need to integrate mental health services into Nigeria’s primary health care system to ensure access for people in rural communities. He noted that although mental health was adopted as the ninth component of primary health care in 1989, the policy has not been implemented more than three decades later.
Indeed, Nigeria’s Mental Health Policy is centered on the National Mental Health Act 2021, signed into law in January 2023. Key aspects include establishing human rights-based protections and promoting the integration of mental health into primary care. The extent of implementation remains a source of concern to stakeholders.
He identified genetic predisposition, trauma, drug abuse, loss of jobs or loved ones, and economic hardship as major causes of mental illness, while stigmatisation and discrimination often worsen patients’ conditions.
“In low-income countries where poverty prevails, where infections and other challenges exist, mental illness is bound to be common. There is not much difference between Nigeria and other parts of the world where war and daily killings are realities,” he said.
Owoeye, who also observed that many Nigerians cannot afford the cost of mental health care and called for comprehensive insurance coverage. He added that while the National Health Insurance Authority has included some mental health conditions in the scheme, full integration into the national health insurance scheme is necessary so that patients can access treatment without financial barriers, especially for long-term conditions.
Owoeye described manpower shortages and inadequate facilities as some of the greatest challenges facing mental health care in the country, saying, “There are some states in Nigeria without a single psychiatrist. Clinical psychologists are grossly inadequate, psychiatric nurses are grossly inadequate, psychiatric social workers are the same, and so are occupational therapists. Manpower is a major challenge,” he said.
He stressed the need for continuous training of mental health experts, including psychiatrists, clinical psychologists, psychiatric nurses, psychiatric social workers, and occupational therapists, describing them as “a five-member team crucial to the delivery of mental health services.”
Owoeye also urged the Federal Government to establish research centres dedicated to the study and management of mental health conditions in Nigeria. even as he advised Nigerians to understand their limits and avoid drug abuse as a coping strategy.
“We need to ensure that we don’t turn to drug abuse as a coping mechanism. Some people use drugs to sleep or deal with problems, but that should not be an option. Regular exercise, adequate sleep, enough rest, and active participation in religious activities have been shown to promote mental health…People going to church to sing and dance has really helped our mental health as a nation,” he said.
Accessing mental health care through insurance, subsidies, employer-assisted programmes as necessity
CLINICAL psychologist, Dr Miracle Ihuoma, wants the Federal Government to create a system that allows Nigerians, regardless of their socio-economic background, to access mental health care through insurance, subsidies, or employer-assisted programmes.He said, “Mental health care in Nigeria is evolving. It’s not where it needs to be, but it’s not where it used to be either. There has been progress, but we are not there yet. Mental health care is improving as we’ve seen more private institutions emerge.”
Ihuoma explained that the causes of mental illness are multifaceted and can be grouped into biological, psychological, and sociological factors.
According to him, biological factors include family history, brain chemistry, brain injury, hereditary genetics, and drug use, while psychological factors include loss of employment, poor economic conditions, sexual abuse, physical abuse, and neglect.
He added that sociological factors such as fuel scarcity, loss of loved ones, and incarceration can also trigger or worsen mental health conditions.
Highlighting the major barriers to effective mental health care in Nigeria, Ihuoma listed ignorance, religion, and poor infrastructure as key challenges.
He said, “People don’t know about mental health, and they don’t know where to seek help. Religion is also a major hindrance to the management of mental illness in Nigeria because, a lot of the time, whatever Africans don’t understand, they mystify. So, if an African is experiencing a headache and goes to the hospital, and the doctor says nothing is wrong, they assume it’s spiritual. It might just be a mental health-related issue. There are not many federal neuropsychiatric hospitals, and I’m not sure there are even state-owned ones.”
Ihuoma called for increased public awareness to address stigma, misinformation, and ignorance surrounding mental health. He restated that treatment remains costly and urged the government to establish a national framework to guarantee affordable access for all Nigerians.