My teenage years were ravaged by severe autoimmune disease. In that era, the burdens of treatment for Crohn’s disease rivaled the misery of the affliction.
My illness brought searing stomach pain, fatigue, and fistulas. The steroids my physician prescribed caused breakouts of cystic acne all over my body as well as exhausting bouts of hyperactivity, manic mood swings, and a serious case of moon face.
Hopelessly trapped between symptoms and side effects, I would have jumped at the chance to participate in a clinical trial. Instead, faced with an impossible choice of excruciating pain vs. mania, lethargy, and disfigurement, I opted for an eight-hour surgical intervention.
Forty-six years later, I’m still managing my autoimmune disease, but I’m also a CEO of a biotech company focused on delivering a new kind of cell therapy for people with autoimmune conditions. While biologics transformed what’s possible for people living with Crohn’s, millions of autoimmune patients still manage the side effects, risks, and tradeoffs of lifelong immunosuppressive steroids.
As a teenager, I rarely talked about my condition. For so long, stoicism has been the default posture of so many people living with severe, yet often invisible autoimmune diseases. We’re a community that has been taught to cope, not hope. But recently, thanks to biotechnology innovation, what’s medically possible may be changing.

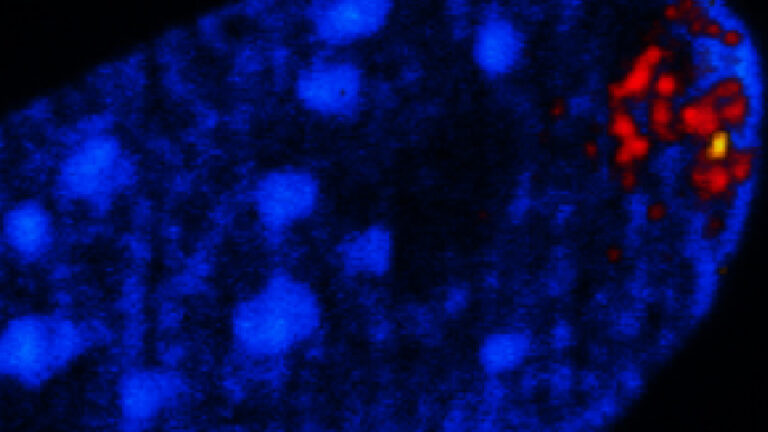
In 2022, a German researcher named Georg Schett showed the world that cell therapy could put a subset of young adult lupus patients into prolonged drug-free remission after conducting a small clinical trial. Many leading scientists now see real potential to replicate this success across other autoimmune diseases.
Drug developers have initiated studies to test this exhilarating thesis, launching more than 500 clinical trials around the world to evaluate cell therapy approaches to treat different autoimmune conditions. Schett’s eureka moment could be a watershed, helping our health care system finally move from chronic immune suppression to curative “immune reset” therapies for many autoimmune patients.
Yet despite this promise, drug developers are discovering that clinical trial enrollment is extremely challenging. Why?
Part of the answer is rooted in demographics. In a striking epidemiological pattern, women of childbearing years are the cohort most likely to develop autoimmune diseases. These ailments disproportionately impact racial and ethnic minorities in incidence and severity. Due to economic disparities in America, the patients who may stand to benefit most from investigative cell therapies are often the most inconvenienced and resource-challenged, struggling to obtain the transportation, lodging, childcare, and the time off work that participation can require.
A national study found that prevalence of systemic lupus erythematosus is higher among people experiencing poverty, food insecurity, unemployment, or reliance on public insurance.
But many autoimmune patients don’t qualify for clinical trials due to stringent U.S. regulatory requirements that they must have failed available advanced therapies, even though they often can’t get these therapies because they’re uninsured or underinsured. It’s a heartbreaking catch-22.
As a growing number of major pharmaceutical and small biotech companies enter this field, industry can play a critical role in reducing barriers to clinical trial participation. Instead of asking people with serious diseases to reconstruct their lives around our studies, drug developers should be striving to design our research around their lives.
There can be costs involved in research participation. If patients aren’t within reasonable driving distance from a site, sponsors should offer airfare, hotel, meals, and child care to ease the burden of participation.
Additionally, companies should offer fair-market compensation to all patients and caregivers for their time and willingness to advance science. A recent open letter signed by 64 leaders in medicine, public health, patient advocacy, and research ethics challenged industry’s historic reticence to fairly remunerate patients for their involvement in clinical research.
Clues from mice could help explain why women face a higher risk of autoimmune disorders
“Research participation generates immense social value, and generous compensation can reflect this value and serve as an important sign of respect and appreciation for all participants,” they wrote. “There is little empirical evidence that payments at levels commonly used in clinical trials, even those in the range of several thousand dollars, result in undue influence — that is, they do not impair the ability of prospective research participants to rationally assess the risks and benefits of participation nor result in choices that conflict with their values.”
Take it from me: Drug developers hear this call. No medically eligible patient should be denied the opportunity to participate in a clinical trial for any reason. Fair-market compensation can make a huge difference for people who wish to enroll but are struggling to make ends meet.
A Canadian study of people living with systemic sclerosis found the disease’s average total annual cost per patient was more $18,000 per year. Another study in systemic vasculitis found that more than a quarter of caregivers lost money due to caregiving; their median annual income loss was $3,000. This is why my company fairly compensates clinical trial participants and their care partners. We call on others to do so, too.
Companies should also consider mobile phlebotomy and lab testing, which reaches into the communities where patients live instead of expecting them to return each time to clinical trial sites far from home. This service can minimize patient burden and time away from home. Mobile clinical trial units can be prohibitively expensive for cash-constrained companies, but the integration of mobile blood draw and lab testing services can help boost trial enrollment by alleviating anxiety and travel burdens for patients with work and family responsibilities.
Drugmakers owe our trial participants more than financial and logistical help. We owe them radical transparency and an honest dialogue about potential risks and benefits. Each new investigational agent comes with trade-offs, and patients should be fully informed by sponsors to make fact-based decisions on what they’re willing — and have every right — to try.
In the case of cell therapy, this includes discussion of lymphodepletion regimens and possible impacts on future fertility. No prospective parent challenged with autoimmune disease should be forced to choose between the chance for better health and the chance to start or grow a family. Cell therapy developers should subsidize sperm and egg retrieval and freezing for participants who want to take precautions against fertility risk — and the government must not stand in the way.
How a company treats its clinical trial pioneers is a litmus test for corporate social responsibility. If my small biotech company with just over 100 employees can offer expansive services to address barriers for study participants and their care partners, so can every other drug developer in this space. As an industry, we have an opportunity and an obligation to guarantee equitable access to clinical trials, so biomedical innovation leaves no one behind.
Paul J. Hastings is CEO of Nkarta, a clinical-stage biotech company in South San Francisco developing natural killer cell therapy.

