Across America, hospitals are vanishing. From Alaska to Florida, towns are losing their lifelines.
And for thousands of families, it’s costing far more than convenience — it’s costing lives.
One of those lives was 78-year-old garden center owner Terry Halfen, from Chippewa Falls, Wisconsin.
When Terry was diagnosed with cancer in late 2023, he was treated at Sacred Heart Hospital in nearby Eau Claire. It was close, trusted, and familiar.
His son Eric moved back home to care for him. For a while, everything felt under control.
Then, in March 2024, Sacred Heart suddenly shut down — terminating almost 1,400 employees and leaving a gaping hole in local healthcare.
‘It was all very sudden,’ Terry’s grandson John Halfen, 20, told the Daily Mail.
‘We just heard on the news that they were closing. It made it so difficult for so many people because that was the go-to hospital. It had everything — the birthing center, the ICU, the CCU.’

John Halfen, 20, said the closure of the local hospital disrupted the care of his cancer-sufferer grandfather Terry Halfen, who died in June aged 78

Across the US, cash-strapped hospitals and emergency rooms are closing their doors to the communities they serve, including this facility in Long Beach, New York
With Sacred Heart gone, the family had no choice but to travel an hour each way to Marshfield for care.
‘The fact of not having a close hospital really made it difficult to get the proper care,’ said John.
‘Having to travel for an hour just to go see him made it very traumatic for all of us.’
His father, Eric, spent hours on the road each day — sometimes six hours total — to sit by his dying father’s bedside.
In June this year, they finally brought Terry home.
Just 48 hours later, he was gone.
‘He was a big family person,’ said John.
‘Not being able to see family as much probably made it worse. We tried to get out as much as we could, but with work and having a kid, it was hard.’
The Halfen family’s ordeal is a devastating example of a growing national crisis — what experts are calling a ‘perfect storm’ of hospital closures sweeping the United States.
Hospitals from coast to coast are closing their doors — sometimes overnight.
Facilities that once delivered babies, treated strokes, and saved lives are vanishing.
The healthcare sector is reeling from financial strain, staff shortages, low insurance reimbursements, and rising costs. A wave of cyberattacks has only added to the chaos.
‘It pains me to see that there’s so many people being affected by the closures and not getting the help they need,’ said John.
‘It creates a lot of hardship for people, and it doesn’t seem to be getting any better.’
The closure of Sacred Heart — and nearby St. Joseph’s Hospital in Chippewa Falls — was just the start.
A recent report from the Center for Healthcare Quality and Payment Reform (CHQPR) warned that Holy Family Memorial in Manitowoc, Mayo Clinic Health System Oakridge in Osseo, and Aspirus Stanley Hospital in Stanley were all at risk of being mothballed next.
Across the country, the same story repeats.
In California, Glenn Medical Center fast-tracked its shutdown. In Texas, Hunt Regional Healthcare said it was losing money so fast it had to close.In Oregon, St. Vincent Medical Center is shuttering units.In Georgia, St. Mary’s Sacred Heart Hospital is scaling back.In Missouri, Landmark Hospital of Cape Girardeau is on the brink.And in Colorado, Banner McKee Medical Center is cutting services to the bone.
Chicago-based economist Dr. Evelyn Martinez described it bluntly: ‘We’ve reached a breaking point where operating a hospital, particularly a standalone one, is simply no longer viable in certain markets.’
The closures are hitting rural America hardest — small-town hospitals that were once the beating hearts of their communities.
Pandemic debt, falling insurance payments, and rising labor costs have crippled local care.
At the same time, major healthcare corporations are consolidating, swallowing up smaller hospitals and then closing ‘duplicate’ facilities to cut costs — often with no warning.

John’s father Eric Halfen moved back with Terry to care for him in the final months of his life

Patients struggled to get a spot in this busy emergency room in Fresno, California, after other centers nearby shuttered
Critics say it’s ordinary Americans who pay the price.
When a hospital shuts down, patients can be left traveling hours for emergency care.
Doctors, nurses, and families are uprooted overnight.
In places like Wisconsin, Kansas, and Alabama, entire counties now have no full-service hospital at all.
Benjamin Anderson, CEO of Hutchinson Regional Healthcare in Kansas, recently told NBC News that staff were being pushed to the limit.
Doctors and nurses are suffering almost as badly as patients, he said, warning that hiring freezes have left workers ‘at real risk of wearing out.’
The data is stark. Becker’s Hospital Review has already counted 21 hospital closures this year alone.
More than 700 rural hospitals — nearly one in three — are now at risk of closing, according to CHQPR.
A Government Accountability Office report added that even urban hospitals are closing faster than new ones are opening, leaving city residents stranded too.
Health leaders say the trend is accelerating. Without major intervention, America’s healthcare ‘deserts’ could soon become a new national emergency.
Experts warn that the crisis is about to get worse.
Republican-led plans to cut Medicaid funding under the One Big Beautiful Bill Act could strip millions of dollars from the system — pushing already struggling hospitals to the brink.

Terry was a ‘a big family person,’ says his bereaved grandson John

Care worker union staff protested at the US Capitol in Washington, DC, in June over medical funding cuts
The Medicaid program, which covers one in four Americans, is often the financial lifeline for rural and safety-net hospitals.
If the cuts go through, facilities in small towns and poorer regions could lose millions in reimbursements.
These hospitals already operate on razor-thin margins, serving patients who rely entirely on Medicaid for care.
Critics say the cuts will create a ‘domino effect of closures’, forcing people to travel even farther for emergency treatment.
‘It pains me to see that there’s so many people being affected by the closures and not getting the help they need,’ John said again.
Republicans insist the reforms are necessary to curb waste and fraud.
But health advocates warn the human cost will be enormous.
California Representative Doug LaMalfa, a Republican, broke ranks to call the proposed cuts ‘unfair and just plain wrong.’
The White House argues that hospitals are closing because of low patient volumes, not low margins, and says the new fund will make small hospitals ‘economically viable.’
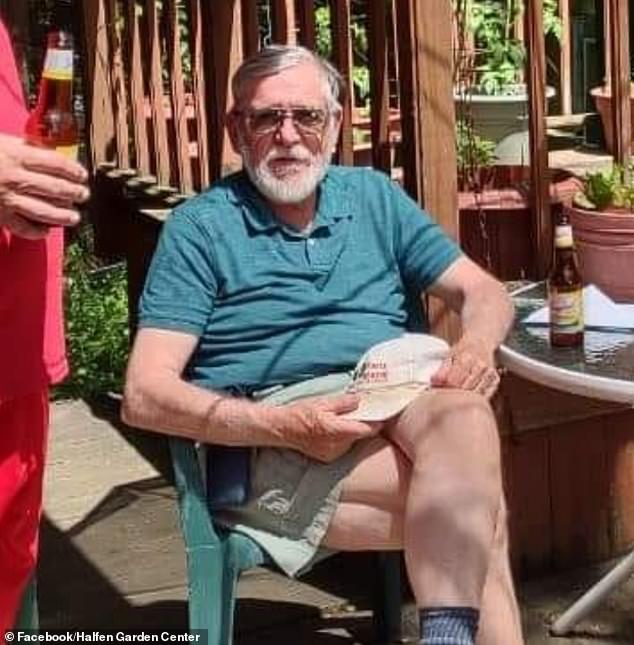
Terry was diagnosed with cancer in late 2023. His local hospital shuttered the following Spring

He cherished his garden center business and had a reputation for growing hostas, a shade-loving plant from East Asia

The green fingered Terry opened his small garden center business in the early 1990s
But in towns like Chippewa Falls, the assurances ring hollow.
The Halfens are still reeling from their loss — and the loss of their local hospital.
John remembers his grandfather as a man who never stopped working and growing his beloved hosta plants, even as his health failed.
‘He never gave up,’ John said softly. ‘Even when he was in hospice, he was joking around, saying, ‘I’m not going anywhere.”
But the hardest part, he said, was knowing that distance and bureaucracy stole precious time.
‘We just closed on his house for a buyer,’ John said.
‘That was pretty rough. He built that house himself. That’s the house I grew up in, my father grew up in. There’s been a lot of tears and laughs. It’s been a process.’
His mother, Jamie Halfen, also owes her life to Sacred Heart.
‘She had a stroke in 2021, and that hospital essentially saved her,’ John said.
‘They put in an emergency dialysis pump right there in the room because there was no time to move her. They were the best.’
Without Sacred Heart, locals have lost their birthing center, their intensive care units, and their cardiologists.
People who once drove ten minutes for care now face an hour on the road — if they can afford it.
‘It hurt a lot of people,’ John said. ‘Me, my fiancée, my son — it creates a lot of hardship, and it doesn’t seem to be getting any better.’

This medical center in Fresno, California, had to seat patients in tents after nearby hospitals closed

The White House is under pressure over looming cuts to Medicaid that threaten to shutter more hospitals
Today, John works at a behavioral group home while raising his young son. He still lives with the pain of losing his grandfather — and the frustration of a system that, in his view, abandoned them.
‘If we still had Sacred Heart,’ he said, ‘it would’ve made everything a lot easier — for him, and for us.’
He paused, then smiled faintly.
‘He was always about the garden center.’
