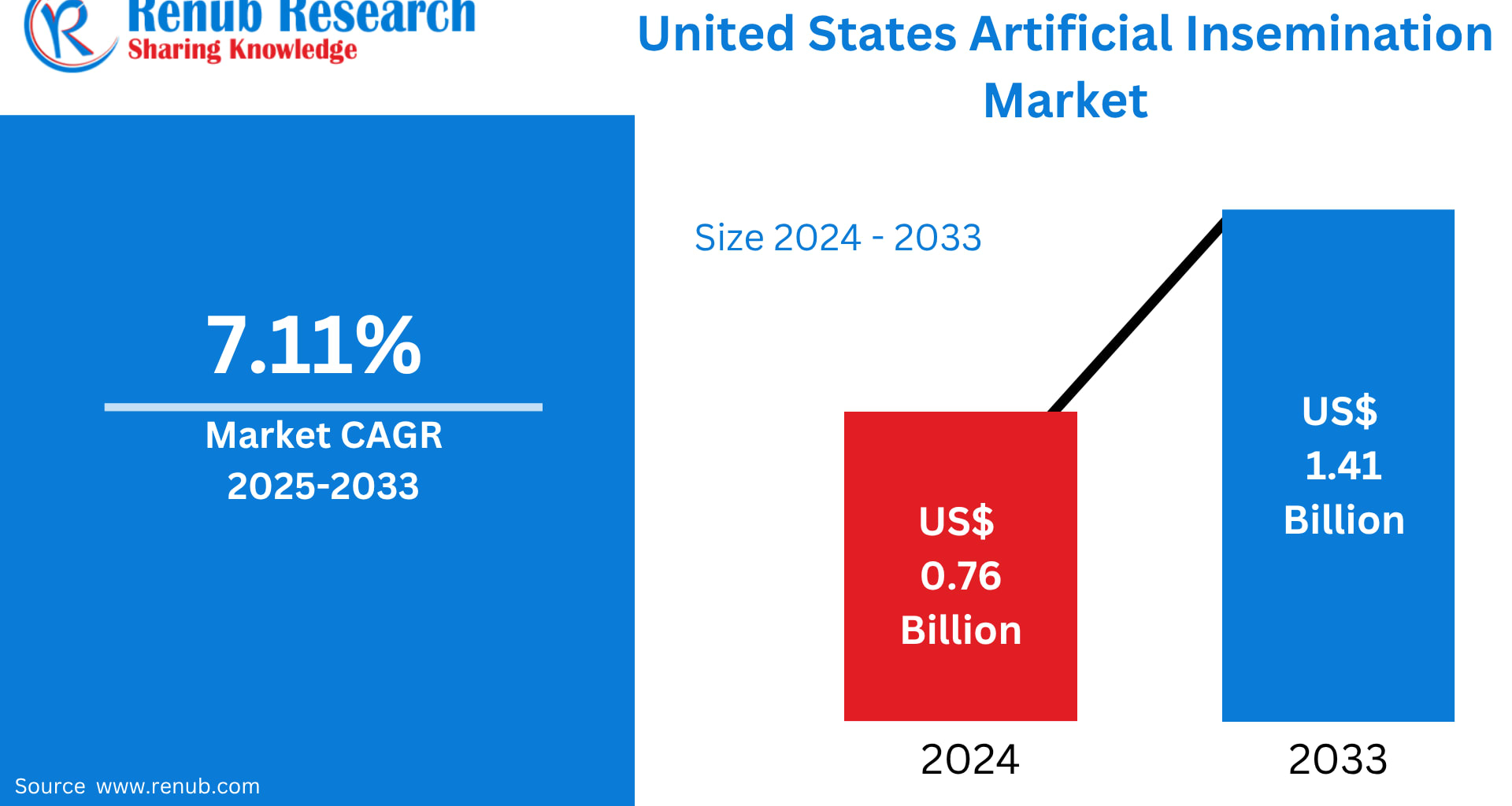
The United States Artificial Insemination Market is on a strong upward trajectory, expected to grow from US$ 0.76 billion in 2024 to US$ 1.41 billion by 2033, registering a CAGR of 7.11% during 2025–2033, according to Renub Research. This surge reflects a significant societal and healthcare shift: Americans are increasingly turning to medically assisted reproductive techniques due to rising infertility rates, lifestyle factors, technological advancements, and broader social acceptance of alternative family-building paths.
Artificial insemination (AI), once seen as a niche medical intervention, is now a mainstream, minimally invasive assisted reproductive solution adopted by a diverse demographic—infertile couples, single parents by choice, LGBTQ+ families, and individuals facing medical challenges. With sophisticated reproductive infrastructure and expanding insurance support, the U.S. landscape for fertility services continues to mature rapidly.
United States Artificial Insemination Industry Overview
Artificial insemination involves the intentional placement of sperm into a woman’s reproductive tract—typically the cervix, uterus, or fallopian tubes—without sexual intercourse. Depending on clinical requirements, the procedure is performed as:
Intrauterine Insemination (IUI)
Intracervical Insemination (ICI)
Intravaginal Insemination (IVI)
Intratubal Insemination (ITI)
Patients may use either partner sperm (AIH) or donor sperm (AID). The procedure is often combined with hormonal stimulation or ovulation tracking to increase pregnancy success rates.
Over the past decade, AI has transformed into a widely used fertility treatment with improved success rates, driven by innovations in:
Sperm washing and preparation
Cryopreservation
Timing optimization
Hormonal protocols
At-home insemination kits
Rising awareness of ART methods and more open societal attitudes are pushing artificial insemination into the mainstream. Fertility clinics nationwide are expanding accessibility, while supportive insurance coverage in several states is helping reduce financial barriers.
Key Growth Drivers in the U.S. Artificial Insemination Market
1. Rising Infertility Rates
Infertility has become a major public health concern in the United States. According to CDC data, the general fertility rate dropped to 54.5 births per 1,000 women aged 15–44 in 2023, down from 56 in 2022—a continuing downward slide.
Reasons for this trend include:
Increased maternal age due to delayed parenthood
Hormonal disorders such as PCOS
Lifestyle factors: stress, obesity, smoking, environmental pollutants
Male infertility linked to declining sperm quality
As natural conception becomes more challenging for many couples, reliance on assisted reproductive technologies—including artificial insemination—has increased substantially. Advances in reproductive medicine, improved success rates, and growing public education are further reinforcing demand.
2. Growing Awareness of Assisted Reproductive Technologies (ART)
Media coverage, celebrity disclosures, social campaigns, and improved healthcare communication have brought fertility treatments into everyday conversation. This heightened visibility has fueled demand for methods such as IUI and IVF.
Key factors contributing to rising awareness include:
Educational campaigns by fertility clinics
Increasing presence of fertility conversations on social media
LGBTQ+ advocacy promoting family-building options
Accessible webinars, community outreach, and online consultations
Trust-building through patient success stories and testimonials
As myths surrounding ART diminish, more couples and individuals are willingly exploring medical fertility options earlier and with greater confidence.
3. Rise in Accessible Fertility Clinics Across the U.S.
The growth of fertility clinics—both independent and hospital-based—has drastically improved access to reproductive healthcare. Clinics now offer:
Advanced diagnostic equipment
Patient-centric fertility programs
Sperm and embryo handling expertise
Counseling and emotional support services
Tailored protocols based on individual reproductive profiles
Furthermore, suburban and semi-urban regions are witnessing the emergence of new fertility chains, reducing the strain on large metropolitan clinics. Telehealth consultations and remote tracking technologies have widened access in rural populations as well.
With increased accessibility comes increased adoption, fueling market expansion across states.
Major Challenges in the U.S. Artificial Insemination Market
1. High Treatment Costs
Despite advancements, the affordability of fertility treatments remains a significant barrier.
Artificial insemination procedures involve expenses such as:
Diagnostic tests
Hormonal medications
Multiple insemination cycles
Ultrasound monitoring
Sperm preparation
Travel and clinical fees
Insurance coverage varies widely, and many plans cover fertility services only partially. For some patients, the high cost prevents completion of multiple cycles—often required to achieve pregnancy. Expanding reimbursement and offering flexible financing solutions remain crucial to boosting access.
2. Regulatory and Ethical Considerations
The artificial insemination industry faces a complex network of federal and state regulations governing:
Donor screening and consent
Sperm and embryo handling
Genetic testing
Storage procedures
Reporting compliance
Patient rights and confidentiality
Ethical issues—especially surrounding donor anonymity, parental rights, genetic selection, and embryo handling—add additional layers of complexity. Clinics must balance innovation with strict oversight, which can increase operational costs and lengthen adoption time for emerging technologies.
State-Level Market Insights
California: A National Leader in Artificial Insemination
California stands as one of the most advanced fertility markets in the U.S., driven by:
High public awareness
Liberal family-building policies
A diverse population including single parents and LGBTQ+ couples
World-renowned fertility specialists and research centers
Urban hubs such as Los Angeles, San Diego, and San Francisco offer state-of-the-art ART technologies, strong counseling frameworks, and supportive health programs. The state’s progressive outlook and steep adoption curve make it a powerhouse within the national market.
Texas: A Rapidly Rising Fertility Hub
Texas is emerging as one of the fastest-growing markets, powered by:
Expanding metropolitan centers like Houston, Dallas, and Austin
A booming young population
Increased acceptance of assisted reproduction
Growing networks of fertility clinics
As telehealth and mobile diagnostic services reach rural communities, access continues to widen. Awareness campaigns, lower stigma, and cutting-edge reproductive technologies are propelling strong growth in this region.
New York: A Major Urban Fertility Powerhouse
New York, especially New York City, is a prime market due to:
Dense population
High infertility awareness rates
Easy access to premium medical centers
Adoption of fertility benefits among corporate employers
Career-driven lifestyles often lead to delayed parenthood, directly increasing demand for ART procedures. With a rich ecosystem of specialists, telemedicine consultations, and strong patient support services, New York remains a significant contributor to overall U.S. growth in artificial insemination.
Florida: Expanding Market with Strong Medical Infrastructure
Florida’s artificial insemination market is shaped by:
Diverse communities
High awareness of fertility treatments
Strong healthcare infrastructure
Fast-growing urban regions like Miami, Orlando, and Tampa
Comprehensive patient care, improved rural accessibility, and rising adoption among LGBTQ+ families support sustained market expansion. Personalized treatment programs and advanced reproductive technology integration make Florida an important state in the national fertility landscape.
Recent Developments Shaping the U.S. Artificial Insemination Market
October 2024: Femasys partnered with Boston IVF to introduce FemaSeed, expanding access across nearly 30 clinics in the U.S. The collaboration aims to enhance treatment success through precision insemination technology and expanded education efforts.
March 2024: Femasys Inc. reported positive results for its pivotal FemaSeed trial, with pregnancy rates hitting 24% in severe male-factor infertility cases, outperforming standard IUI. This breakthrough paves the way for wider commercialization.
December 2023: The FDA approved Mosie Baby, the first OTC at-home artificial insemination kit, enabling consumers to perform insemination at home using fresh or frozen sperm. This innovation democratizes access and may redefine the future of low-complexity fertility treatments.
U.S. Artificial Insemination Market Segmentation
By Type
Intrauterine Insemination (IUI)
Intracervical Insemination (ICI)
Intravaginal Insemination (IVI)
Intratubal Insemination (ITI)
By Source Type
AIH – Husband
AID – Donor
By End Use
Hospitals & Clinics
Fertility Centers
Other End Users
By States (29 Viewpoints)
California, Texas, New York, Florida, Illinois, Pennsylvania, Ohio, Georgia, New Jersey, Washington, North Carolina, Massachusetts, Virginia, Michigan, Maryland, Colorado, Tennessee, Indiana, Arizona, Minnesota, Wisconsin, Missouri, Connecticut, South Carolina, Oregon, Louisiana, Alabama, Kentucky, Rest of United States.
Key Players Covered (5 Viewpoints Each)
Company Overview | Key Persons | Recent Development & Strategies | SWOT Analysis | Sales Analysis
Vitrolife
Genea Pty Limited
Rinovum Women’s Health, LLC
Pride Angel
HI-TECH SOLUTIONS
FUJIFILM Irvine Scientific
Kitazato Corporation
Rocket Medical plc
Conceivex, Inc.
Final Thoughts
The United States artificial insemination market is entering a transformative era powered by increasing infertility prevalence, advanced technological innovation, and growing public acceptance of assisted reproductive methods. With the market set to reach US$ 1.41 billion by 2033, the future of fertility care in America is defined not only by medical breakthroughs but also by shifting cultural narratives around family-building.
As more states expand insurance coverage, as more clinics adopt precision-based fertility technologies, and as at-home insemination solutions become widely accessible, artificial insemination is poised to become one of the most inclusive and rapidly evolving segments in the reproductive healthcare sector.