First, the nation is beginning to make progress in key areas of public health because biomedical science is delivering meaningful breakthroughs on some of our most difficult challenges. These advances are a powerful reminder that well-targeted innovations can drive large improvements in population health.
For the first time in decades, US obesity rates have flattened — and even begun to fall. A smaller share of Americans were obese in 2024 than in 2022, a remarkable shift largely driven by the growing use of GLP-1 medications. Once used mainly for diabetes, these drugs are now more widely available and also reduce cardiovascular risk, lower the likelihood of some cancers, and may even influence addiction and neurodegenerative diseases.
We are also seeing similar momentum in the opioid crisis. Provisional data on overdose deaths for 2024 show a drop to their lowest level since 2019, according to the Centers for Disease Control and Prevention, driven by expanded access to medication-assisted treatment such as naloxone and buprenorphine. Researchers are also developing nonaddictive pain treatments — an important step toward preventing future waves of dependency.
Meanwhile, CRISPR gene editing has given scientists the ability to adjust genes with extraordinary precision. This year, it was used to treat rare, previously untreatable genetic diseases and appears to have corrected a fatal disorder in a 5-month-old boy. Early research is exploring how CRISPR might help treat more common conditions, such as high cholesterol, and how to finance broad access to these emerging therapies so they reach the people who need them most. A similar shift is happening with GLP-1 drugs, and the Trump administration’s push to bring down their prices is an important step.
Second, for decades the federal government served as the cornerstone of health data and recommendations relied on by state and local health departments, clinicians, parents, and the public. Under Health and Human Services Secretary Robert F. Kennedy Jr., that system has become wildly dysfunctional — it’s no longer a reliable source of essential data and only rarely a source of credible guidance. Fortunately, medical societies, state leaders, and academic researchers have begun filling many of the gaps.
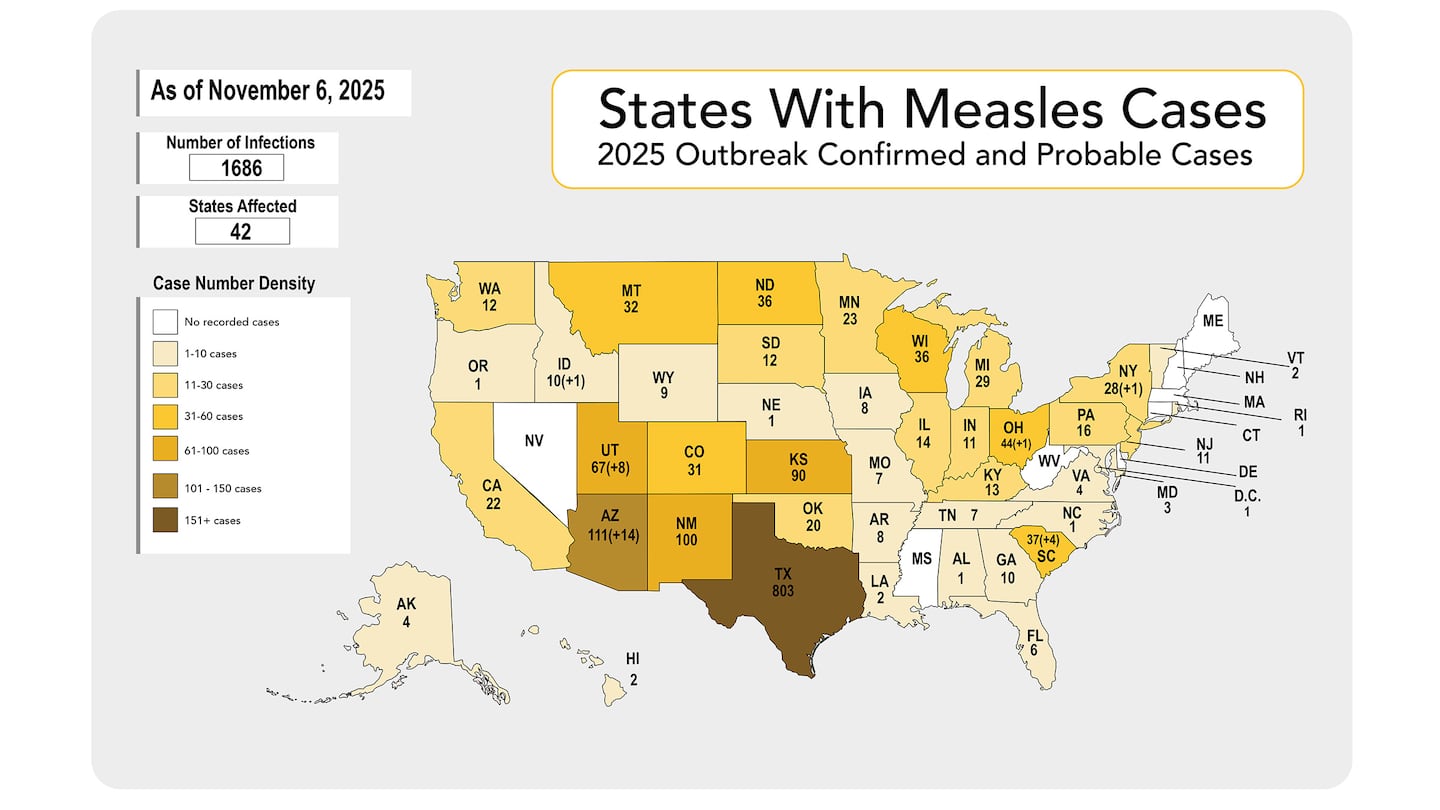
From Massachusetts to California, states have built collaboratives to coordinate vaccine recommendations, emergency planning, and disease surveillance — stepping in while the federal government ignores major public health threats and works to undermine vaccine confidence and access. And as federal dashboards for infectious diseases and mental health went dark, academic institutions and medical organizations such as the Vaccine Integrity Project provided transparent, scientifically grounded analysis.
My colleagues at the Brown University School of Public Health launched a weekly virus-tracking report that now reaches more than 10,000 subscribers and is increasingly used by local health departments seeking real-time data. Independent communicators have played a key role as well; through widely read Substacks and social media channels, public health voices like epidemiologist Katelyn Jetelina have kept much of the public informed in clear, accessible ways.
These efforts underscore the resilience of the US public health ecosystem and its ability to adapt — but they are no substitute for a high-functioning, highly trusted CDC.
Third, the federal government just reopened after the longest shutdown in US history — a self-inflicted debacle that left federal workers without paychecks and disrupted services millions rely on. Worse, the Trump administration tried to use the shutdown to cut food assistance through the Supplemental Nutrition Assistance Program.
In response, local institutions, grass-roots groups, and everyday Americans rallied to ensure people had enough to eat. In Rhode Island, veterans and volunteers collected nearly 2,000 pounds of food for the Providence Veterans Affairs hospital pantry. In Nebraska, bookstore employees organized a food drive that brought in a similar amount. In Pittsburgh, a school pantry helped dozens of families with food and hygiene products. Across the country, community food pantries saw an unexpected uptick in donations.
These efforts deserve thanks not only from those who received support but from the country as a whole. Many of the people who went without SNAP benefits or missed paychecks were our neighbors, friends, and family.
Now it’s time for Congress and the president to finally address the issue that helped spark the shutdown in the first place. Health care in the United States remains extraordinarily expensive, and the federal government and states must confront the high costs that make it so difficult to cover all Americans. It’s time to shine a bright spotlight on this fundamental challenge.
As this difficult year in public health draws to a close, it can seem quaint to take a moment to recognize what we’re thankful for, especially with so many challenges on the horizon, from soaring health care costs to rebuilding trust in science and public health. But practicing gratitude, whether in our personal lives or in public health, is not about feeling better during difficult times. It reminds us of our strengths and of what we can accomplish together.
Wishing you and your loved ones a happy Thanksgiving and a healthy holiday season.