The state announced reductions to at least 15 programs last year as part of a broader effort to balance the state’s budget.
DENVER — Some families of Coloradans with disabilities are now learning exactly when planned Medicaid cuts will take effect. The Polis administration announced reductions to at least 15 programs last year as part of a broader effort to balance the state’s budget but the timing for many of the service reductions was unclear, until this week.
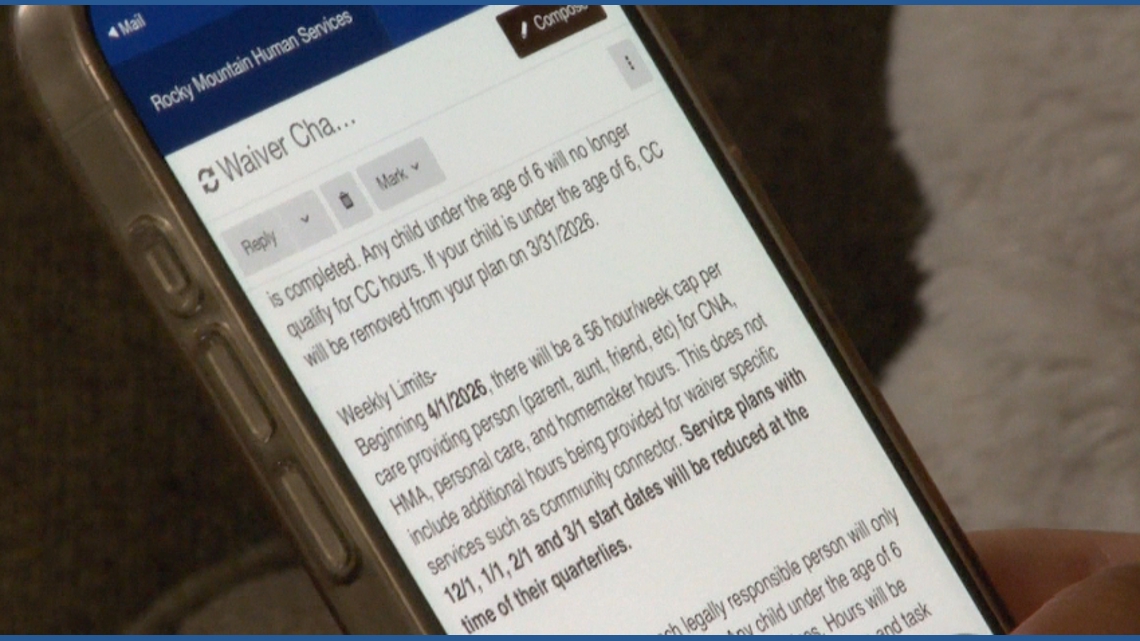
Jordyn Feckovic, mother of 3-year-old Langston, received notice Thursday from her case manager that effective April 1, the paid homemaker hours she relies on will be cut in half. Her son, who has autism, will also lose access to the Community Connector program, which helps children with disabilities develop skills through everyday activities such as visiting social places.
“When I got the letter basically saying that Community Connector would be eliminated [for children under 6] at that point, it’s like, well, that’s it,” Feckovic said. “These services have made him blossom, and without these, I’m worried that we would be facing some real regression.”
Langston is one of roughly 40,000 Coloradans impacted by reductions to Medicaid programs that support people with disabilities and their caregivers. Feckovic said the changes are a significant setback.
“This isn’t about a paycheck,” she said. “This is about providing essentials, the bare necessities, for our loved ones and our children.”
“The faster that we can achieve savings, the less reductions we have to take,” Bonnie Silva, the division director for the Office of Community Living with the Department of Health Care Policy and Financing (HCPF), said in a November interview. “So, that’s why you see us moving so quickly in a way that is not typical of state government.”
Silva acknowledged the cuts will impact some families but said the measures are targeted to ensure the sustainability of the state’s long-term care programs.
“We’re not in a position where we have to remove services in their entirety,” she said on Nov. 13. “But I don’t want to be dismissive. These changes will have an impact for some members and for some families, and I certainly recognize how difficult that is.”
In a statement on Friday HCPF said case managers have been asked to speak with affected families as early as possible to prepare them for reductions.
“We heard from many members, providers, and caregivers, and we have listened carefully to their concerns and questions,” a spokesperson for HCPF said on Friday. ” HCPF has asked case managers to have conversations now with members, ensuring members are informed as early as possible about the upcoming changes and can plan accordingly. These changes will not be effective until April 1, 2026. In most cases, the Medicaid Sustainability policy changes will affect members at their annual renewal or during their next scheduled meeting with a case manager. Depending on timing, this could happen as early as April 2026 or as late as November 2026.”
HCPF refused to answer if more reductions would be expected the next budget cycle. Feckovic fears that may be the case but she hopes those that make the decisions understand the impact.
“These people have real needs, “she said in a message to state leaders. “We want to be heard. We want to be understood and all I ask is to open your hearts.”